Abstract
The aim of this study was to describe reproductive decisions in mutation carriers after predictive testing for Huntington's disease (HD) and to identify factors that play a role in decision-making. In 1987–2004, 245 individuals received a predictive test result; 89 of them were carriers and seven received an equivocal result. Quantitative data on reproductive behaviour have been collected during all follow-up contacts. The follow-up time in this study was 1–16 years (mean: 7.1 years). Qualitative data on reproductive decision-making have been collected by the means of semistructured interviews during the 5-year follow-up study.
For 46 carriers and two persons with an equivocal result, family planning was one of the motives for predictive testing. In this group, slightly more than half of the carriers (58%) had chosen to have children with prenatal diagnosis or preimplantation genetic diagnosis and about one in three (35%) decided to have no children anymore after the test. A minority (7%) was undecided or had no children for other reasons. Factors playing a role in the decision-making process were the carrier's sex, ethical issues about PD and PGD, the strength of the desire to have children, illness representations including personal experiences with HD in the family and the technological imperative. Some of these elements were in conflict and induced ambivalence towards reproductive choices. The results illustrate the complexity of the decision-making process and the necessity of in-depth counselling. Counselling should pay special attention to conflicting values and beliefs and to all kinds of pressure.
Similar content being viewed by others
Introduction
Predictive testing for Huntington's disease (HD) has been available for nearly 20 years. Several studies1, 2, 3, 4 and 5 have shown that family planning was one of the main reasons for asking for a predictive test. Genetic testing for HD indeed brought new options for reproduction: prenatal diagnosis (PD) and, since 1998 available in Belgium, preimplantation genetic diagnosis (PGD). PGD is performed on embryos the third day after in vitro fertilisation (IVF) and only non-carrier embryos are transferred to the uterus. The chance of a treatment resulting in a birth is about 20% per cycle. Direct PD and PGD can be utilised by known mutation carriers and by persons at risk. Prenatal exclusion testing, PGD exclusion testing and non-disclosure PGD can be used by at-risk persons who want to exclude carriership in their offspring but do not want to know their own carrier status.6, 7, 8, 9 and 10 The principle of exclusion testing is that transmission of the HD region of chromosome 4 from the affected grandparent is excluded by means of linkage analysis. If the linkage analysis indicates that the HD allele, which has been passed to the embryo, originated from the affected grandparent, the embryo shares the same 50% risk of being a HD carrier as the intervening parent. In that case, the pregnancy will be terminated (after PD) or the embryo will be excluded from transfer (after PGD), although on average only 50% of the embryos will contain the HD mutation. In non-disclosure PGD, direct mutation testing is used during PGD, but the parents do not receive information on the carrier status of the embryos. They only know that non-carrier embryos have been transferred. Given the practical and ethical dilemmas of non-disclosure PGD, it has been considered unacceptable by most people and institutions.7, 8, 9 and 10
In general, the uptake of PD in HD families is low.11, 12, 13, 14, 15, 16, 17 The most frequently mentioned reasons for not using PD were reluctance to pregnancy termination, the hope that an effective treatment would be found in time, the desire for a child outweighed the future threat and concern about the safety of the procedures. Already having children and religious beliefs were also factors in deciding against PD.16 Taken into account the population in each country, the proportion of reported PD was highest in the Netherlands,11, 13 the UK,12, 13 Belgium13 and Denmark.17 In Leiden, the Netherlands, for instance, Maat-Kievit reported 72 prenatal tests in 43 couples (26 proven carriers and 17 at-risk persons) in the period 1987–1997. All pregnancies with an unfavourable result (100 or 50% risk) were terminated. In Britain, the UK HD Prediction Consortium recorded data on all prenatal tests in the period 1994–1998: 146 prenatal tests were reported, 45% in carriers, 54% in at-risk parents. Sixty-one of the 66 unfavourable results were terminated. Very few prenatal tests were reported in Canada,14 Australia,15 France and Italy,13 and Greece, Germany, Austria and Switzerland.17 In general, the proportion of carriers using PD was less than 20%. Several explanations for the variation between countries have been suggested: different counselling procedures, cultural and religious views on reproduction and on pregnancy termination, and different expectations regarding treatment prospects. Reports on the uptake of PGD in HD families are scarce, but also show a low utilisation rate.8, 9
A European study in seven genetic centres of six countries focused on reproduction after predictive testing for HD (period: 1993–1998).4 In the group of 96 persons at reproductive age (⩽45 years) who reported family planning as a motive for predictive testing and with a follow-up of 3–7 years, 40/58 (69%) of the non-carriers and 15/38 (39%) of the carriers had subsequent pregnancies. Among carriers with pregnancies, the proportion using PD was slightly higher than the proportion not using it. Large differences existed between centres.
The aim of this study was to describe reproductive behaviour in carriers after predictive testing for HD. This implies that only direct mutation testing including PD and PGD was relevant for them. PD and PGD are routinely discussed during counselling for HD. In Belgium, PD and PGD are accessible for HD-mutation carriers and for persons at risk. PD is covered by public health insurance. PGD, including IVF, has only been covered since 2003.
Besides quantitative data on reproductive behaviour, we also present qualitative data to identify factors that played a role in reproductive decision-making. The current study differs from the already available literature in that a longer follow-up period after predictive testing has been covered. Moreover, it adds depth and context by including qualitative evidence on decision-making, which was lacking in most published studies.
Methods
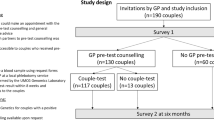
In Leuven (Belgium), predictive testing for HD has been available as a clinical service since November 1987.18 Follow-up counselling is available for all tested couples. All individuals who agreed to be contacted for follow-up were invited by phone for systematic psychological counselling at 1 week (only for carriers), 1 month, 1 year and 5 years post-test. Moreover, many carrier couples have had contacts more than 5 years after their test result (see Table 1 for details on follow-up period). Almost all carrier couples with reproductive plans have had several counselling sessions in our centre in the context of family planning and reproduction.
Five years after predictive testing, we invited carrier couples to participate in an extensive follow-up study to collect information on psychological functioning,19, 20 the partner relationship21 and reproductive decision-making after testing. Those who accepted to participate were interviewed after clinical counselling. For the introductory questions of the research interview, the tested person and the partner were interviewed together. For the rest of the interview (about 80%), they have been separately interviewed, face to face, each by another member of the HD team. For both interviews, a semistructured interview guide with open questions was used, covering the following themes: perceived changes after testing, unexpected consequences of testing, perceived advantages and disadvantages, impact of the test result on relationship with the partner and the family, reproductive decision-making, problems and worries during the past 5 years, help-seeking behaviour and perceived health status. Counselling was provided if problems emerged during the interview. The interviews took between 1 and 2 h. Moreover, psychometric questionnaires were used.19, 20, 21 (See Table 1 for participation rate in the 5-year follow-up interview.)
Quantitative data on reproductive behaviour were based on all follow-up data available (period: 1988–2005). Qualitative data on the decision-making process were based on the research interview of the 5-year follow-up study. The interview data have been analysed based on the grounded theory approach.22 Repeated reading and coding of all interview notes resulted in several topics referring to family planning and reproductive decision-making.
Categorical variables were analysed with χ2 or Fisher's exact tests, continuous variables with t-tests.
Participants
In the period November 1987–November 2004, 245 individuals had received a test result: 89 carriers, 149 non-carriers and seven with an equivocal test result (CAG repeat between 27 and 39). For 46 carriers (52%) and for two persons with an equivocal result, family planning was one of the motives for predictive testing. Table 1 presents baseline socio-demographic characteristics for carriers and for persons with an equivocal result, with and without reproductive motives for predictive testing (total group n=96). Carrier couples with reproductive motives were significantly younger and had less children at baseline than carrier couples without reproductive motives for predictive testing.
In the carrier group with reproductive motives, 32 carriers had been tested at least 5 years ago and 17 of them (53%) participated in the 5-year follow-up study; in the carrier group without reproductive motives, the participation rate in the 5-year study was 56% (15/27). We already previously showed19, 20, 21 that participants and non-participants in the 5-year follow-up study did not significantly differ regarding baseline socio-demographic data.
Results
Tested persons with reproductive motives for predictive testing
Carriers (n=46)
We have information on reproductive behaviour in 45 of the 46 carriers. Twenty-six of the 45 carriers (58%) chose to have children after testing, 16 of the 45 carriers (35%) chose to have no children after the test (and actually had no children anymore), one couple was undecided and two couples had no children because of recent divorce or relational problems. Table 2 presents details on reproduction in the 26 couples who decided to have children after predictive testing (period: 1988–2005). Twenty-three of the 26 couples had pregnancies, one couple had two IVF/PGD trials without pregnancy, one couple had just started with IVF/PGD and one couple tried to get pregnant and planned PD. The 23 couples with pregnancies had 51 pregnancies: 46 pregnancies with CVS, three after PGD and two ended in a spontaneous miscarriage. Half of the CVS test results were positive, and these pregnancies were all terminated. The other 23 CVS resulted in 23 children born to 20 couples.
In 1998, PGD became available for HD. In the period 1998–2005, seven couples had at least one IVF cycle followed by PGD, with a total of 15 cycles. After PGD became available, 13 couples had 21 pregnancies with CVS; five of them used both PD and PGD.
Adoption, or donation of gametes or embryos has not been used.
Age at baseline (a few weeks before result disclosure)
The mean age of carriers who chose to have children with PD or PGD after testing (n=26) was 26.7 (SD=3.8), and the mean age of those who had no children after testing (n=16) was 28.0 (SD=4.1). The difference was not statistically significant (t-test).
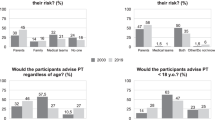
Sex
One woman was undecided and two men had no children because of divorce or relational problems. Among the other carriers, 18/23 men chose for having children with PD or PGD, whereas 5/23 men chose to have no children (78 vs 22%). Among females, 8/19 chose for having children with PD or PGD and 11/19 chose to have no children (42 vs 58%). These differences were significant (Fisher exact test; P<.05).
Having children at baseline
Eight carrier couples already had children before testing; 4/8 had pregnancies with PD or PGD and 4/8 had no children anymore (50 vs 50%). In those who had no children before testing, 22/37 chose for having children with PD/PGD after testing, whereas 12/37 chose to have no children (59 vs 32%). The differences were not statistically significant (χ2).
Pregnant during predictive testing
Three persons, who proved to be carriers, were already pregnant when presenting for predictive testing. The couples received a shortened testing procedure, including in-depth counselling on the implications of predictive testing and prenatal testing. All three chose to have PD after predictive testing. Two of them received a positive CVS result and both terminated the pregnancy.
Follow-up period
The mean follow-up period after predictive testing was 7.3 years (SD=4.5) for carriers who chose to have children with PD or PGD after testing (n=26), and 8.7 years (SD=4.0) for carriers who decided to have no children after testing (n=16). The difference was not statistically significant (t-test).
Persons with an equivocal test result (n=2)
One woman was pregnant during predictive testing. She had a CVS and intended to terminate the pregnancy in case of an extended CAG repeat (>39) in the fetus. The CVS result was in the reduced penetrance range and she continued the pregnancy. The other woman was undecided about further pregnancies.
Tested persons without reproductive motives for predictive testing
Carriers (n=43)
After the test, four children were born to three couples. One carrier couple had two children at baseline and had another child after the test, without PD or PGD. They hoped that a cure would be found before their children would develop HD. Another couple had two children after testing; they had three pregnancies with CVS, one with a favourable result and two with an unfavourable result. One of these pregnancies was terminated; the other was continued. The third couple had one child after a favourable CVS result.
Persons with an equivocal test result (n=5)
None of them had children after the test.
Qualitative data
On the basis of the data collected during the 5-year follow-up interviews, we selected themes that directly or indirectly referred to the reproductive decision-making process.
-
Spontaneously mentioned advantages/disadvantages of PD and/or PGD
A frequently mentioned benefit was having children without the HD mutation, which brought relief and peace of mind for the parents. A frequently mentioned disadvantage was the psychological and physical burden of a pregnancy termination. Both positive and negative aspects are clearly illustrated by the following comment:
Carrier (male; after several CVS and after the birth of children): It was hard to see my wife suffering after every termination. We knew that it was our personal and deliberate choice, but having children in this way required more energy, psychologically as well as physically. For both of us, but especially for my wife. It meant burden and suffering, but now we are very glad that we have children of our own and that they are free from the disease. Nor we, nor the children will have to worry about them becoming ill in the future, like I do. Otherwise we would have chosen to have children with a donor.
Another disadvantage mentioned by a few couples was the reluctance to become emotionally attached to the pregnancy until good news after the CVS was given.
Partner (female; after several CVS and after the birth of a child): During the first months of each pregnancy, we felt uncertain and numb. We could not be happy or feel attached to the pregnancy until we knew the result of the CVS. We had each time a long distressing period of waiting for the results of the CVS. And nobody knew we were pregnant… we did not want to trigger negative reactions.
This also illustrates that couples kept the pregnancy and the termination secret because of fear of rejection from others. A benefit mentioned by some was that the children could bring support and comfort for the healthy parent when the other parent got ill.
Carrier (male; after CVS and PGD and one child born): It is positive that my partner will have support from the children when I get ill and she won’t be alone when I die. Should the children be at risk, it would be an extra burden for her instead of relief. Partner: I will loose him, but part of him will stay alive in our children. It will be more bearable because of our children.
Seven couples had at least one IVF. Two of them spontaneously mentioned the artificial way of conceiving and the psychological distress associated with it.
Partner (female; after the IVF-trial): They had warned us: it would take a big effort. Indeed, it did. The injections, the pick-up, the frequent visits to the clinic, … nothing natural, and a lot of stress…
Five couples had experiences with both PD followed by a pregnancy termination and unsuccessful PGD trials. A female carrier explicitly compared both experiences:
Carrier (female, after several CVS and PGD): There was nothing romantic about getting pregnant after IVF. It was a large investment of time and energy. On the other hand, the disappointment after an unsuccessful IVF-trial was much smaller than after a positive prenatal test. In case of the IVF-trials, I had not been pregnant for 3 months and I did not have to terminate a pregnancy.
-
Decision conflicts, uncertainties and ambivalences
The decision about having children was complex and ambiguous for most couples. Several couples mentioned a conflict between the responsibility to prevent suffering and the reluctance towards pregnancy termination:
Carrier (female, after CVS): It was hard to decide. Isn’t it unethical to terminate a pregnancy if the person can be healthy for 40 years? We have considered having a child in a natural way, but that option was unacceptable for us. Could we bring a child into the world with such a high risk for a serious disease?
One of the cited reasons for being indecisive about the use of PD or PGD was the hope that a cure would be found in time. There is no certainty about a future treatment and this led to decisional difficulties in some couples. In the following situation, there was a conflict between the hope for a cure and concern that a cure would not be found in time:
Carrier (male; after CVS and one child born): It was very difficult to decide about a pregnancy termination. We hesitated … Maybe a treatment will be found in time? But if they don’t?
Even after the actions taken, parents may continue to question the decision made. In the following situation, the hope for a cure led to doubts after the pregnancy termination:
Carrier (female, after CVS and one child born): Last month, I saw a documentary on television, on transplantation for HD patients, it was so hopeful, and I thought, maybe we took the wrong decision? maybe we did not need to have had a pregnancy termination?
The following case is about a carrier with a strong desire for having children and with an ambivalent attitude towards pregnancy termination. The woman, however, felt that it was her moral responsibility to prevent the disease in the children, and therefore, she wanted PD. She already had a previous PD and a pregnancy termination. She had an (unplanned) pregnancy and PD. Even though the woman was hesitant about a pregnancy termination, the couple had planned an abortion should the foetus be carrier. They received an unfavourable CVS result. Although the partner tried to convince his spouse to terminate the pregnancy, the woman decided to continue the pregnancy. The case illustrates that ambivalence about termination, combined with a strong desire for having children, may lead to the continuation of the pregnancy after an unfavourable CVS result.
Carrier (after the unfavourable CVS): It was so difficult to decide about the PD, and I thought I took the right decision: I did not want to pass the disease to my child. But I really want that child. I was so happy being pregnant. I couldn’t stand another pregnancy termination.
Some couples expressed their concern about their children growing up with an affected parent and therefore hesitated about having children. Some of them referred to their own previous negative experiences with the disease in their parent:
Carrier (female, divorced; after CVS and one child born): Although my children can be free of the disease, I’m still worried about having children because they will see their mother becoming ill, like I did. I have made an arrangement with my sister that she will take care of my children when I become ill. That puts me more at ease.
-
The technological imperative and anticipated regret
The availability of PD and PGD may put a pressure on prospective parents. The following couple chose to have PD because not using it would confront them with feelings of guilt and regret.
Carrier (male; after CVS and PGD): My father always said: we didn’t know and there was nothing we could do. But we have the possibility to prevent the birth of a child at risk. So, we can’t say anymore that we didn’t know or that we couldn’t do anything. It would be unbearable having children and not having used PD. You knew you could do something but you didn’t.
Fifteen of the 23 couples who used PD/PGD had repeated PD and/or PGD. Some couples felt a pressure to use a medical intervention in every pregnancy:
Carrier (female; after several CVS): The repeated pregnancies and prenatal diagnoses and the repeated disappointments were hard to bear. But I felt we had to go on, otherwise all previous suffering would have been for nothing. And each time, I thought: better luck next time and I knew that once a child was born, we would forget all pain and sorrow of the last years.
In the previous situation, the carrier felt that, after the initial use of PD, they had to continue to use it in further pregnancies. The comment, moreover, illustrated that the parent expected that the eventual birth of a healthy child would counterbalance earlier negative experiences. This was also the case in the next situation:
Carrier (male, after repeated unsuccessful PGD): We want to have a healthy child as soon as possible. It has to grow up in another family than I did. I want to start a new life with my wife and child and forget the bad things in my life.
-
The choice to have no children
The decision to have no children was hard for most couples:
Carrier (female): The decision to have no children was not easy. One day we thought: yes, the other day: no. But, in the end, it was no. There was no other solution: pregnancy termination was not acceptable for me.
Carrier (female): The first year after testing was very hard, because I realised that I would never have children. I do not want that my children have an affected mother and that they go through the same as I did in my family. We have accepted it now, and I can put more time in my career now. Although I’m convinced that we took the right decision, sometimes I feel pain in my heart, when my friends are pregnant, or when I see young parents playing with their children.
Important reasons mentioned by carrier couples for having no children were objections against pregnancy termination for a late onset disease, not wanting that children have an affected parent, pessimism regarding a cure or treatment and the opinion that ‘the disease should be stopped’. The following couple refrained from having children, based on the high risk for a pregnancy termination in case of PD and on the low risk for success in case of PGD:
Partner (female): The gynaecologist told us that, in case of a pregnancy with prenatal testing, the risk to have a positive result was one in two. Thus a chance of one in two to undergo a pregnancy termination. That risk was too high. In case of PGD, the chance to have a pregnancy was only 20% per trial. The risks for bad luck and failures were too high. So, we preferred to have no children.
In the next situation, the carrier even went a step further: he did not want children, but also no relationship. His decision was based on negative childhood experiences with the disease in his parent.
Carrier (male): My father was affected with HD and I have seen what has happened in our family: my mother cried a lot and we have all suffered very much. I’m very determined: no relationship and no children. I can’t do that to anyone.
Discussion
This paper focused on reproductive behaviour in carriers after predictive testing for HD, involving a follow-up period of 1–16 years. In the group of carriers with family planning as one of the motives for predictive testing, slightly more than half of the couples (58%) had chosen for PD and/or PGD and one-third (35%) had decided to have no children anymore. A minority was undecided or had no children for other reasons, such as an unstable relationship. A previous study23 reported that 1 year after predictive testing one-third of the carriers was still undecided. These findings indicate that some couples need a long time of reflection on reproduction. In the group of carriers who did not ask the test for reproductive reasons, two couples had prenatal testing. One couple continued a pregnancy after an unfavourable CVS, and one couple had a child without PD/PGD. The group of persons with an equivocal result was too small to make general conclusions.
Most previous research found that more females than males chose to undergo PD.11, 14, 15 In our study, male carriers were more likely to choose for PD/PGD, whereas females were more likely to refrain from having children. This may indicate that the mother is still recognised as the most important person for child caring and rearing in our society. In case of a couple with a male carrier, the mother can take care of the children when the father becomes ill. In case of a couple with a female carrier, it is the prospective mother who will become affected. A considerable number of couples may feel that a mother should be available for the care of the children and may therefore choose to have no children.
Qualitative data showed that deciding about having children was complex and that multiple factors played a part. One of the salient factors was the availability of PD and PGD. On the one hand, the medical technology can prevent much distress about offspring. However, future parents interested in PD have to face the question whether it is acceptable to terminate a pregnancy for HD. The child will be healthy during three or four decades but there will be the psychological burden of the genetic risk; moreover, they will witness one of their parents becoming ill. In general, pregnancy termination proved to be less acceptable for adult-onset diseases than for congenital abnormalities or serious diseases with onset in childhood.24, 25 In our study, pregnancy termination was considered an important drawback of PD and was perceived as psychologically and physically demanding. For some couples, it was an insurmountable objection against PD. In case of IVF with PGD, the burden associated with the complex way of conceiving and the low success rate were mentioned as disadvantages by some couples. A study on attitudes towards the new reproductive genetic technologies25 reported that in general, PD was considered less acceptable than PGD because of the emotional trauma in case of an abortion. In this study, most couples had undergone PD partly because PGD only became available in 1998. In the period when PGD was available, the proportion of couples choosing for PD was still larger than the proportion choosing for PGD. This may be owing to the experimental character and the novelty of PGD in the first years after its launch, the complex way of conceiving and the low success rate. Moreover, the lack of public health insurance coverage of IVF/PGD between 1998 and 2003 may have played a part. Given the burden of a pregnancy termination, compared with PGD, it is possible that the uptake of PGD will relatively grow in the future, certainly if the baby take-home rate would considerably improve. It is, however, important to keep in mind that balancing the pros and cons of all options is a highly individual and subjective process, dependent on many factors.
The qualitative analysis showed that two additional ethical questions were important in the deliberation on reproduction: is it acceptable to have children who may develop a serious debilitating disease later in life, and is it acceptable to have children if there is uncertainty about the adequacy of the future parenting role? Some couples found it unacceptable that their child would suffer from threatening anxieties and uncertainties because of the genetic risk and therefore chose for PD or PGD. Some of them were concerned about their children growing up with an affected parent, but this was not a reason to refrain from having children. Other couples felt that it was unacceptable that the child would have a parent with a serious disease jeopardising the parental role, and therefore chose to have no children. These concerns about prevention of suffering in the children reflect parental feelings of responsibility towards their offspring. According to Downing,26 the perception of responsibility is a core concept in reproductive decision-making about HD, whether or not genetic testing is used. She illustrated in three extensive case studies how negotiating responsibility may evolve over time with maturity, changing relationships, changing risk status and testing options.
The above-mentioned ethical questions may be in conflict with each other, but also with other issues, such as the strength of the desire to have own children, resulting in ambivalence. Several studies16, 27, 28 revealed that the importance of having children overrode all other concerns. The desire to have a healthy child may be an expression of the need to have a normal life and to compensate for the previous suffering, as illustrated in this study. This desire for a compensative healthy child may be so strong that couples are ready to make difficult choices.29 In our study, a couple having a strong desire for children and an ambiguous attitude towards abortion, continued a pregnancy after an unfavourable PD. It is clear that reproductive decision-making may be a matter of conflicts and ambivalence, subject to conscious and unconscious processes. Partners within a couple, moreover, may have different attitudes towards these issues. In our study, most couples showed a consensus concerning reproductive choices. Self-selection may be an explanation: couples sharing the same values and attitudes are more likely to seek genetic testing. A more plausible explanation, however, is that partners have deliberated on reproductive issues and made shared decisions outside the counselling context, conciliating different values and beliefs.
Another factor playing a role in reproductive decisions was the personal experience with HD in the family. Some carriers referred to their own painful experiences with the disease in their parent and felt that they could not put a child through analogous negative emotions. The experience with the family disease is a subjective emotional matter, shaped by several interrelated factors:1, 2, 30, 31, 32 disease characteristics (eg age at onset), the familial context (eg patient pre-selection processes) and person characteristics (eg ego strength). According to the self-regulation model,32 not only emotional but also cognitive representations of the disease influence coping and behaviour. An important element in the cognitive representation of HD is the belief about potential treatment or cure. In general, pessimism regarding future medical progress is associated with the choice to have no children or to have children with PD/PGD. The prospects regarding therapy or treatment for HD are however unpredictable. Should promising progress be made in medical technology, then individuals who refrained from having children or who had PD/PGD may regret the decisions made.
Adam et al16 showed that the availability of the medical technology created a pressure to use it. For some couples in our study, the technological imperative indeed played a part. Not using the technology would induce feelings of guilt, irresponsibility and self-blame. These anticipated feelings confirm the importance of perceptions of responsibility in reproductive decision-making for HD.26 Some couples, moreover, expressed the feeling that all the previous suffering would have been in vain should they not continue to use PD/PGD. This feeling may exponentially grow after repeated failures. The idea that the eventual birth of a mutation-free child would compensate for all the previous efforts has compelled some couples to go on until at least one child was born.
Several other factors may (unconsciously) affect the decision-making process, such as family dynamics,26, 33 opinions and choices of relatives26 and the attitudes of professionals.34 Elger and Harding34 reported that, despite strong professional codes of non-directiveness, future physicians may be somewhat directive in some counselling situations. This shows the importance of a sustained attention to discourage unwarranted pressure on reproductive choices and to stimulate non-directive counselling.
This paper focused on decision-making, and not on quality of life of the participants. We have previously shown19 that persons who had well-defined reasons for predictive testing, such as family planning, were significantly less anxious and depressed before as well as 5 years after predictive testing, compared with persons with unspecified motives. The clinical practice, moreover, learned that, with the exception of one person who had an episode of depressive symptoms after pregnancy termination, all participants coped reasonably well after reproductive decision-making. Couples who have children with a different risk status, however, will be confronted with difficult situations in the future and this may endanger quality of life. Four couples had children before the predictive test and chose to have children who do not carry the HD mutation after testing, and one couple had a child who is not a carrier (after a favourable CVS) and another child who is a carrier (pregnancy continuation after an unfavourable CVS). In these situations, the children's different risk status will complicate the communication process on HD in the family and may lead to difficulties in the parent–child or the sib–sib relationship, undermining the developmental process of the children.24, 35 The case of the pregnancy continuation after the positive CVS result, moreover, evokes other delicate issues, such as the child's right to make its own decision about testing as an adult.10 The potential harmful effects over time highlight the importance of in-depth counselling on the implications of all possible options, to promote free, informed decision-making. Although these kinds of situations are rather exceptional, qualitative research is needed on their long-term impact on parents and children's quality of life.
This study only included persons who had undergone predictive testing. It is important to realise that, all over the world, the majority of at-risk persons had no predictive test. The most commonly reported objections against predictive testing were concern about the inability to cope with a high-risk result, the belief that important decisions do not need to depend on a test result, the lack of a treatment, concerns about the children and the potential loss of health insurance.36, 37 A study in 50 untested persons showed that most at-risk couples did not refrain from having children, although some had less children than they desired because of the genetic risk.36 The European study on PD showed that in the period 1993–1998 prenatal exclusion testing was a significant option: two-thirds of PD were by direct testing and one-third by exclusion testing.13 The interest in exclusion PGD compared with direct PGD was somewhat lower.8 Overall, large differences between centres and countries exist. It is, however, clear that a number of couples at risk attach great importance to excluding carriership in their offspring along with remaining ignorant about their own carrier status.
We have no interview data of the couples who did not participate in the 5-year follow-up study. Their baseline socio-demographic characteristics did not significantly differ from the group of participants. It is, however, possible that other or additional themes have played a part in their reproductive decision-making process.
Given the broad range of topics covered in the interview, the qualitative data gathered are rather explorative. Further in-depth qualitative research focusing on reproductive decisions should deepen the findings. Especially the experiences with IVF-PGD for HD need further investigation, given the relative novelty of this procedure.In conclusion, it is clear that reproductive decision-making is a complex process, subject to emotional and unconscious elements. Several factors play a role and some are in conflict, inducing ambivalence. Given these complexities, extensive in-depth counselling is needed, preferably by a counsellor with expertise in genetic testing for HD. The predictive testing counselling sessions are ideal occasions to discuss these issues, before as well as after testing: they offer the participants sufficient time to reflect on the information given to weigh the pros and cons, taking into account personal values, beliefs and emotions. Some couples need considerable time to come to reproductive decisions. This means that long-term follow-up counselling is necessary. Counselling should be non-directive and should aim to enhance personal control and free informed decision-making. Special attention should be paid to conflicting values and beliefs and to all kinds of pressure. This requires considerable time, a personal involvement of the counsellor and high standards of knowledge and counselling skills to communicate clearly and sensitively with the counselees in a safe environment.
References
Evers-Kiebooms G, Decruyenaere M : Predictive testing for Huntington's disease: a challenge for persons at risk and for professionals. Patient Educ Counsel 1998; 35: 15–26.
Tibben A, Frets PG, Van de Kamp JJ et al: On attitudes and appreciation 6 months after predictive DNA testing for Huntington's disease in the Dutch program. Am J Med Genet 1993; 48: 103–111.
Craufurd D : Huntington's disease. Prenat Diagn 1996; 16: 1237–1245.
Evers-Kiebooms G, Nys K, Harper P et al: Predictive DNA-testing for Huntington's disease and reproductive decision making: a European collaborative study. Eur J Hum Genet 2002; 10: 167–176.
Goizet C, Lesca G, Dürr A : On behalf of the French group for presymptomatic testing in neurogenetic disorders: presymptomatic testing in Huntington's disease and autosomal dominant cerebellar ataxias. Neurology 2002; 59: 1330–1336.
Evers-Kiebooms G, Fryns JP, Demyttenaere K et al: Predictive and preimplantation genetic testing for HD and other late onset dominant disorders: not in conflict but complementary (letter). Clin Genet 1996; 50: 275–276.
Braude PR, de Wert GM, Evers-Kiebooms G, Pettigrew RA, Geraedts JP : Non-disclosure preimplantation genetic diagnosis for Huntington's disease: practical and ethical dilemmas. Prenat Diagn 1998; 18: 1422–1426.
Geraedts J, Liebaers I : Preimplantation genetic diagnosis for Huntington's disease; in Evers-Kiebooms G, Zoeteweij MW, Harper PS (eds): Prenatal Testing for Late-Onset Neurogenetic Diseases. Oxford: BIOS Scientific Publishers Ltd, 2002, pp 107–118.
Moutou C, Gardes N, Viville S : New tools for preimplantation genetic diagnosis of Huntington's disease and their clinical applications. Eur J Hum Genet 2004; 12: 1007–1014.
de Wert G : Ethical aspects of prenatal testing and preimplantation genetic diagnosis for late-onset neurogenetic disease: the case of Huntington's disease; in Evers-Kiebooms G, Zoeteweij MW, Harper PS (eds): Prenatal Testing for Late-Onset Neurogenetic Diseases. Oxford: BIOS Scientific Publishers Ltd, 2002, pp 129–158.
Maat-Kievit A, Vegter-van der Vlis M, Zoeteweij M et al: Experience in prenatal testing for Huntington's disease in the Netherlands: procedures, results and guidelines (1987–1997). Prenat Diagn 1999; 19: 450–457.
Simpson SA, Harper PS : On behalf of the UK Huntington's disease Prediction Consortium. Prenatal testing for Huntington's disease: experience within the UK 1994–1998. J Med Genet 2001; 38: 333–335.
Simpson SA, Zoeteweij MW, Nys K et al: Prenatal testing for Huntington's disease: a European collaborative study. Eur J Hum Genet 2002; 10: 689–693.
Creighton S, Almqvist AW, MacGregor D et al: Predictive, prenatal and diagnostic genetic testing for HD: the experience in Canada from 1987 to 2000. Clin Genet 2003; 63: 462–475.
Richards FH, Rea G : Reproductive decision making before and after predictive testing for HD: an Australian perspective. Clin Genet 2005; 67: 404–411.
Adam S, Wiggins S, Whyte P et al: Five year study of prenatal testing for HD: demand, attitudes, and psychological assessment. J Med Genet 1993; 30: 549–556.
Yapijakis C, Laccone F, Sorenson SA : Predictive and prenatal testing for HD in Greece, Germany, Austria, Switzerland and Denmark; in Evers-Kiebooms G, Zoeteweij MW, Harper PS (eds): Prenatal Testing for Late-Onset Neurogenetic Diseases. Oxford: IOS Scientific Publishers Ltd, 2002, pp 69–82.
Decruyenaere M, Evers-Kiebooms G, Boogaerts A et al: Predictive testing for Huntington's disease: risk perception, reasons for testing and psychological profile of test applicants. Genet Counsel 1995; 6: 1–13.
Decruyenaere M, Evers-Kiebooms G, Cloostermans T et al: Psychological distress in the 5-year period after predictive testing for HD. Eur J Hum Genet 2003; 11: 30–38.
Decruyenaere M, Evers-Kiebooms G, Boogaerts A et al: Partners of mutation-carriers for Huntington's disease: forgotten persons? Eur J Hum Genet 2005; 13: 1077–1085.
Decruyenaere M, Evers-Kiebooms G, Cloostermans T et al: Predictive testing for Huntington's disease: relationship with partners after testing. Clin Genet 2004; 65: 24–31.
McAllister M : Grounded theory in genetic counselling research. J Genet Counsel 2001; 10: 233–250.
Decruyenaere M, Evers-Kiebooms G, Cloostermans T et al: Prediction of psychological functioning one year after the predictive test for Huntington's disease and impact of the test result on reproductive decision making. J Med Genet 1996; 33: 1–7.
Craufurd D : Counselling aspects of prenatal testing for late-onset neurogenetic diseases; in Evers-Kiebooms G, Zoeteweij MW, Harper PS (eds): Prenatal Testing for Late-Onset Neurogenetic Diseases. Oxford: BIOS Scientific Publishers Ltd, 2002, pp 179–190.
Kalfoglou AL, Doksum T, Bernhardt B et al: Opinions about new reproductive genetic technologies: hopes and fears for our genetic future. Fertil and Steril 2005; 83: 1612–1621.
Downing C : Negotiating responsibility: case studies of reproductive decision-making and prenatal genetic testing in families facing HD. J Genet Counsel 2005; 14: 219–234.
Frets P, Duivenvoorden H, Verhage F et al: Factors influencing the reproductive decision after genetic counseling. Am J Med Genet 1990; 35: 496–502.
Richards F : Couples’ experiences of predictive testing and living with the risk or reality of Huntington disease: a qualitative study. Am J Med Genet 2004; 126A: 170–182.
Jacopini G, Decruyenaere M, Harper R, Simpson S : Case histories of prenatal testing for HD; in Evers-Kiebooms G, Zoeteweij MW, Harper PS (eds): Prenatal Testing for Late-Onset Neurogenetic Diseases. Oxford: BIOS Scientific Publishers Ltd, 2002, pp 11–24.
Kessler S, Bloch M : Social system responses to HD. Fam Process 1989; 28: 59–68.
Helder D : Living with Huntington's Disease. Leiden, 2002, doctoral dissertation.
Leventhal H, Nerenz DR, Steele DF : Illness representations and coping with health treats; in Singer A, and Singer J (eds): A Handbook of Psychology and Health. Hillsdale: Erlbaum, 1984, pp 219–252.
Demyttenaere K, Evers-Kiebooms G, Decruyenaere M : Pitfalls in counseling for predictive testing in Huntington's disease; in Evers-Kiebooms G, Fryns JP, Cassiman JJ & Van den Berghe H (eds): Psychosocial Aspects of Genetic Counseling. March of Dimes Birth Defects. New York: Wiley-Liss, 1992; 28: 105–112.
Elger B, Harding T : Huntington's disease: do future physicians and lawyers think eugenically? Clin Genet 2003; 64: 327–338.
Codori AM, Zawacki KL, Petersen GM : Genetic testing for hereditary colorectal cancer in children: long-term psychological effects. Am J Med Gen 2003; 15: 117–128.
Decruyenaere M, Evers-Kiebooms G, Boogaerts A et al: Non participation in predictive testing for Huntington's Disease: individual decision making, personality and avoidment behaviour in the Family. Eur J Hum Genet 1997; 5: 351–363.
Van der Steenstraten I, Tibben A, Roos RA, Van de Kamp JJ, Niermeijer MF : Predictive testing for Huntington disease: nonparticipants compared with participants in the Dutch program. Am J Hum Genet 1994; 55: 618–625.
Acknowledgements
We express special gratitude to the couples who participated in this study. We thank Professor A De Paepe (Ghent) and Professor J Dumon (Antwerp) for their permission to include testees from their centre. Also thanks to Trees Cloostermans who had a major role in the follow-up counselling.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Decruyenaere, M., Evers-Kiebooms, G., Boogaerts, A. et al. The complexity of reproductive decision-making in asymptomatic carriers of the Huntington mutation. Eur J Hum Genet 15, 453–462 (2007). https://doi.org/10.1038/sj.ejhg.5201774
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ejhg.5201774
Keywords
This article is cited by
-
Genetic counseling and testing practices for late-onset neurodegenerative disease: a systematic review
Journal of Neurology (2022)
-
Perceptions of genetic testing in patients with hereditary chronic pancreatitis and their families: a qualitative triangulation
European Journal of Human Genetics (2021)
-
Informing about genetic risk in families with Huntington disease: comparison of attitudes across two decades
European Journal of Human Genetics (2021)
-
Comparison of Patients’ Ethical Perspectives of Preimplantation Embryo Genetic Testing for Aneuploidy (PGT-A) vs. Monogenic Disorders (PGT-M)
Reproductive Sciences (2021)
-
Reproductive options for families at risk of Osteogenesis Imperfecta: a review
Orphanet Journal of Rare Diseases (2020)