Abstract
Study design:
Quasi experiment; single experimental group with matched historical control.
Objectives:
To evaluate the effect of an additive robotic-assisted gait training (RAGT) using the Lokomat system on the neurological and functional outcomes of patients with subacute spinal cord injury (SCI).
Setting:
Department of Physical Medicine and Rehabilitation.
Methods:
A total of 28 subacute SCI patients were treated by RAGT, 2–3 times a week, 30–45 min every treatment, concomitantly with regular physiotherapy. As control, for each patient, we matched a comparable patient treated in the same department in previous years, according to age, severity of injury, level of injury and cause. The main outcomes were: the AIS (American Spinal Injury Association impairment scale) the spinal cord independence measurement (SCIM) score, the walking index for SCI II (WISCI II) and functional ambulation category scale (FAC).
Results:
At the end of rehabilitation, both groups showed a significant improvement in both the FAC score and the WISCI score (P<0.01) without differences between the groups. Functional abilities, according to the SCIM score, were also improved, with a significant interaction effect; the RAGT patients improve by 30±20 points, which was significantly greater gain as compared with the controls, 21±14 points (P=0.05). This improvement was mainly due to the change in the SCIM motor subscales.
Conclusion:
RAGT is an important additional treatment to improve the functional outcome of subacute SCI patients. Larger, controlled studies are still required to determine the optimal timing and protocol design for the maximal efficacy of RAGT in SCI patients.
Similar content being viewed by others
Introduction
Ambulation recovery in spinal cord injury (SCI) patients is depending mainly on motor recovery.1 Recent statistics indicate that more than 50% of people with SCI have motor incomplete lesions.2 In patients with an initial motor incomplete SCI, more than 75% of patients regain some form of ambulatory function. Factors associated with better recovery are age, level of the lesion and American Spinal Injury Association impairment scale.3 Approximately half of motor recovery occurs within the first 2 months after initial injury with a decreasing rate after 3 to 6 months.4 In Israel, survival and neurological recovery rates after SCI rehabilitation are close to those reported in other countries.5
Although conventional rehabilitation programs enhance performance of functional tasks, the loss of strength and coordination substantially limits one's capacity for overground ambulation training.6 In patients with incomplete or complete SCI, a bilateral leg muscle activation combined with coordinated stepping movements can be induced in partially unloaded patients standing on a moving treadmill.7 This locomotor training that incorporates high repetitions of task-oriented practice using body-weight support treadmill training (BWSTT) was introduced as a promising treatment concept for SCI patients. BWSTT enables early initiation of gait training, integration of weight-bearing activities, stepping and balance by use of a task-specific approach and a symmetrical gait pattern.8 However, despite BWSTT's theoretical potential to become an invaluable therapeutic tool, its effect on walking outcomes was disappointing when compared with conventional training of the same duration.9
To facilitate the delivery of BWSTT in SCI patients, a motorized robotic-driven gait orthosis was developed,10 which has many advantages over the conventional BWSTT methods including less effort for the physiotherapists, longer duration, more physiological and reproducible gait patterns, and the possibility to measure a patient's performances. Two different commercial robotic devices for locomotor training had been employed in different studies, the Lokomat (Hocoma Inc., Zurich, Switzerland) a treadmill-based walking machine with robotic arms to move the patients’ legs,11 and the ‘Gait Trainer’ consisting of two footplates whose driven movements simulated stance and swing.12 Although the gait patterns induced by these motor-driven devices have not been characterized and compared,13 the results of clinical trial with both of these systems were similar. This emphasizes that the effect of locomotor treatment by robotic-derived gait orthosis is independent of the type of device used.
Several studies showed that robotic-assisted gait training (RAGT) improves overground walking ability in individuals with incomplete SCI.14, 15, 16, 17, 18 According to these trials, RAGT increased the odds of becoming independent in walking; however, great variations were found among these trials regarding the time of treatment initiation, duration and frequency of treatment as well as differences in the ambulatory status of the patients. Most of these studies were not controlled and included a relatively small number of patients, and the locomotor treatment was initiated quite late after the SCI.
The aim of this study was to evaluate the clinical effect of combine treatment of RAGT using the Lokomat system (Hocoma Inc.) and conventional physical therapy as compared with conventional physical therapy alone in subacute SCI patients. Our hypothesis was that the combined treatment of RAGT with regular physiotherapy will prove to be superior to conventional treatment regarding the regaining of walking abilities and rate of improving of functional level.
Materials and methods
Participants
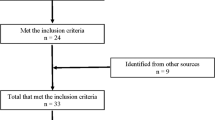
Between 1 September, 2005 and 30 September, 2009, all SCI patients admitted to the Department of Physical Medicine and Rehabilitation at Hadassah Medical Center in Jerusalem were evaluated and patients who were eligible were offered to participate in the study. Inclusion criteria were spinal cord lesion as a result of traumatic or non-traumatic causes and exclusion criteria were patients with pressure sores, severe limitation of range of motion of the hips and knee joints, and patients with severe cognitive impairment The study was approved by Ethical Board Committee of Hadassah Medical Center and all patients agreed to participate in the study. The design of the study was a quasi-experimental trial with historical controls. During this period 28 SCI patients were treated by RAGT using a robotic-driven gait orthosis device (Lokomat; Hocoma Inc.): 6 patients with complete SCI (AIS A), 22 patients with incomplete SCI (7 patients with AIS B, 13 with AIS C, and 2 patients with AIS D). The classification was done upon admission to rehabilitation just before Lokomat training was initiated. As control, for each patient in the study group, we matched a comparable SCI patient treated in our department in previous years according to age, severity of injury (AIS scale), level of injury (cervical, thoracic and lumbar) and cause traumatic or non-traumatic.
Intervention
The Lokomat system
The Lokomat system (Hocoma Inc.), includes a treadmill, a body-weight support system and two light-weight robotic actuators that attach to the subject's legs. The speed of the treadmill can be adjusted from 0 km h−1 to approximately 3 km h−1. During the treatments, the velocity of the treadmill was set individually, to the maximum speed tolerated by the patients. At the beginning of the treatment, approximately 50% of each subject's body weight needed to be supported by the harness system. During the following walking sessions, the body-weight support was reduced in approximately 10% increments per session as tolerated without substantial knee buckling or toe drag.
The study group
The study group received RAGT by the The Lokomat system (Hocoma Inc.) for 2–3 times a week and regular physiotherapy 5 times a week in the rest treatment days. The overall time of the RAGT treatment was 1 h whereas the net robotic gait training was for 30 min and the regular physiotherapy treatment lasted for 30–45 min.
The control group
The historical control group was treated by regular physiotherapy for 30–45 min five times a week using Bobath principles.
Measurements
All patients were assessed upon admission and upon discharge from the rehabilitation department. All evaluations were performed by a rater who was not involved directly in treating the study patients. The main outcomes were the ability to walk independently according to the functional ambulation category (FAC) scale19 and functional motor assessment by the walking index for SCI II (WISCI II20). The FAC scores ranged between independent walking over a 15-m surface irrespective of aids used (4 or 5), walking on level surfaces without manual contact of another person but, for safety, requires stand-by guarding or the need for verbal cuing to complete the task (3), dependency in walking (1 or 2) and unable to walk (0).21 The WISCI II is a 20-item scale measuring the walking status of a patient based on the requirements of assistance and/or bracing and/or walking aids. Grade 0 means that the patient has neither standing nor walking abilities and grade of 20 means that no assistive device, no brace and no assistance is needed for at least 10 meters walking. The neurological status was assessed using the AIS.3 The daily living functions were evaluated using the Spinal Cord Independence Measurement (SCIM), by an independent assessor unaware to the patient's allocation. The SCIM is a disability scale developed specifically for patients with SCI and was found to be reliable and sensitive tool in measuring functional changes in SCI patients.21 The total SCIM score ranges from 0 to 100 including the following areas of function: self-care (subscore 0–20), respiration and sphincter management (0–40) and mobility (0–40). Each area is scored according to its proportional weight in the patient's general activity. The score of first 8 items represents the non-motor functional ability and the rest items represent the motor functioning including special locomotor subscore including items 12–14. People scoring three or less in the locomotor subscore were classified as dependent walkers.22
Statistical analysis
Descriptive analysis of the demographic and injury characteristics was done using frequency distribution for categorical data, and mean (s.d.) for continuous variables. Differences between groups were assessed by a t-test (for continuous variables) and a χ2-test (for categorical variables). Treatment effect on functional performance (SCIM) was subjected to repeated-measures analysis of variance with group as the between-subject factor (Lokomat vs Control) and time as the within-subject factor (admission and last rehabilitation measures). As the WISCI II, FAC and AIS are all ordinal scales, frequencies and medians were used as descriptive statistics for these outcomes, and non-parametric tests were used to assess the relative effect of the treatments. Differences were calculated between WISCI II admission and last measurements. Within-group comparisons of treatment effects relative to baseline were carried out with the Wilcoxon test, and between-group comparisons were performed with the Mann–Whitney U test. Results were considered statistically significant when the P-value was ⩽0.05. Data were analyzed using an SPSS-v.17 statistical package (SPSS Inc., Chicago, IL, USA).
Results
Demographic data
Demographic and injury data of both groups are presented in Table 1. In both groups, 46% of the patients suffered from cervical injury and the rest suffered from paraplegia as a result of thoracic and lumbar injuries without difference between the groups. In both groups, the cause of SCI was traumatic in 57% of the cases. The majority of the patients in the RAGT group suffered from traumatic SCI due to MVA and fall from height (16). In the non-traumatic group, 50% of the patients in both groups suffered from spondylotic myelopathy, 25% suffered from transverse myelitis and the rest suffered from non-traumatic hematoma and metastasis. No significant difference was found in any of the outcomes measures in both RAGT and controls groups between traumatic and non-traumatic patients. All patients were treated in rehabilitation facility within the first year after the injury. The mean inpatient rehabilitation period was approximately 3 months (mean of 114±79 days in the RAGT group and 112±84 days among the controls, P=0.75). The rehabilitation period was longer in patients who suffered from traumatic SCI as compared with non-traumatic causes (126±85 days vs 104±74 days, respectively, P=0.36). The RAGT treatment was started at a mean of 75 days (range 13–367 days) after the injury and the mean number of treatments was 25 (range 6–110).
Motor function and gait abilities improvement during study—FAC and WISCI II
Walking abilities were evaluated using the FAC and the WISCI II scales. At baseline both groups showed severe ambulation disability; more than 20 patients in each group have FAC score of 0 (Table 2). At the end of the rehabilitation period, both groups showed a significant improvement in ambulation ability according to FAC (Wilcoxon signed ranks test Z=−5.21, P<0.01), with no significant differences between groups. During the rehabilitation period both groups achieved a significant improvement in walking ability according to the WISCI II. The median score for total sample changed from 0.5 (IQR 0–3) at entry time to 6 (IQR 0–13; Wilcoxon signed ranks test Z=−5.41, P<0.01). No significant interaction effect between groups over time was noted; the RAGT group showed change from median score of 1 (0–2) at entry time to 7.5 (1.2–13.7) at the end of the trial as compared with median score of 0 (0–6) at entry time to 6 (0–11.2) at the end of the trial (Table 2) for the control group.
Neurological and functional improvement during study—AIS and SCIM
The neurological and functional status of the patients during the study were evaluated using the AIS and SCIM, respectively. At the beginning and at the end of the rehabilitation period both groups showed similar AIS grades distributions (χ21=3.34, P=0.34 and χ21=0.88, P=0.83, respectively); both groups improved significantly over time (P<0.01). At the end of the study, in the RAGT group, there were 4 patients with complete SCI (AIS A) and 24 patients with incomplete SCI as compared with 6 patients with complete SCI and 22 patients with incomplete SCI in the control group without statistical significance difference between the groups (Table 2).
The SCIM scores of the RAGT and control groups were comparable at the beginning of the rehabilitation process (t54=0.83, P=0.40), both groups improved significantly in their SCIM scores during the rehabilitation period with significant interaction effect; the RAGT patients showed significant greater gain as compared with the controls (the RAGT group improve from 34±19 points to 64±17 points, as compared with 34±21 to 55±22 among the controls, F1:54=8.84, P=0.05, Figure 1). In order to recognize the specific functional abilities in which the robotic treatment was significantly effective, we analyzed the motor versus non-motor sub domains of the SCIM. As can be seen in Table 3, the RAGT patients showed significant greater differences in the motor and the locomotor sub domains of the SCIM and not in the non-motor domains as compared with control.
Discussion
The main finding of our study was that the incorporation of RAGT into the rehabilitation treatment of severely disabled SCI patients did not change significantly their ability for independence walking according to the FAC and WISCI II scores as compared with historical controlled patients treated with regular physiotherapy alone. However, the RAGT group achieved better functional gain as measured by the total and motor subscales of the SCIM. RAGT allows severely affected SCI patients to perform efficient locomotor training without any specific side effects.
Thus far there is no clear evidence for the effectiveness of RAGT in SCI patients. Several systematic reviews including a Cochrane review article were published recently addressing this question, however, there is insufficient evidence to draw conclusion about the effectiveness of this treatment on motor independence, gait parameters, patient's daily functional outcome and social participation.23, 24 Overall, data regarding only 50 SCI patients treated by RAGT were found in the literature; among them only 22 patients in two RCT studies used robotic treatment as one of the treatment arms, and other similar cases were reported in quasi-experimental trials and pre-experimental studies such as case reports and uncontrolled studies.
Only few articles address our main hypothesis that the addition of RAGT to regular rehabilitation treatment will improve the ability to walk independently with fewer walking aids and less support. In these studies, most of them examined chronic SCI patients, no difference was found regarding the independence in walking abilities or the need for walking aid as measured by the WISCI II scores.15 In the only RCT study involving subacute SCI patients, Hornby et al.17 compared different gait trainings in three groups of subacute SCI injury patients with a recent (<6 months) history of traumatic or non-traumatic, non-progressive SCI. They found that all three groups improved significantly from baseline to follow-up with respect to FIM-L, WISCI II and LEMS scores, however, there was no advantage of the robotic treatment over the manual BWSTT and the overground walking training groups. Our study has many similarities to this study including subject population, timing of treatment and treatment protocol, and likewise we also did not find difference between the groups regarding the achieving of walking independence using the FAC and WISCI II scores.17 On the other hand, we found significant improvement in the RAGT group in SCIM locomotor score comparing with no improvement in FIM locomotor in their study. This difference can be explained by the fact that the SCIM is more specific regarding the independence in walking as compared with the FIM-L.
Our study was the first to investigate the influence of robotic locomotor treatment on the total and sub domains of the SCIM in SCI patients. The SCIM has been proven to be valid and highly reproducible in complete and incomplete SCI.22 In our study, the RAGT group showed better results in their function gain as measured by the total SCIM score. This finding was further elaborated and we found, in accordance with our hypothesis, that the significant change was found only in the motor sub domains of the SCIM and not in the non-motor sub domains. The SCIM was found to be a sensitive tool for monitoring functional improvement during the first year after a persistent complete SCI in patients with paraplegia and quadriplegia.25 In this study, similar to our results, SCI patients improved in approximately 30 SCIM units in the first 3 months after the injury. As in our study, no correlation was found between the functional recovery according to the SCIM and the motor recovery rate according to the motor AIS in paraplegic patients.25
The ideal timing and treatment protocol of RAGT is unknown. In our study, the mean interval between the trauma and treatment initiation was relatively shorter to other published studies, 75 days (range 13–367 days). In this relative short period after the injury there is still option for neurological improvement even in patients with complete SCI as defined by AIS grade A. In our group, similar to others,3 two patients (7.1%) from each group, RAGT and control, improve from AIS A grade to better grade without difference between the groups. Therefore, we conclude that in our small group, RAGT did not increase the recovery rate of complete SCI patients. Another important parameter is the number and frequency of the robotic locomotor treatments given. Similar to others,15, 17 we used a regimen of 2–3 session per week for an average of 12 weeks whereas others used more intensive regimen of 20 min each session, five times a week for 4 weeks.16 Our regimen is feasible in a regular setting of rehabilitation of SCI whereas the more intensive high frequency regimen given in other studies is typically not performed in clinical setting because of lack of manpower.
Our study had several limitations: the number of patients per group was relatively small, and included patients with diverse etiologies as well as a mixture of paraplegic and tetraplegic patients. Another weakness is the fact that the subjects were not randomized and the control group was historical. Although simple quasi-experimental designs using historical controls has many weaknesses, it is an accepted approach in evaluation of occupational injury interventions.26 In our study, however, both groups were treated in the same facility by the same multidisciplinary team, and the SCIM evaluation was done by a blinded observer to the allocated group.
In summary, our study adds to the wealth of data showing that RAGT is an important additional treatment to improve the functional outcome of subacute SCI patients, however, the timing and frequency of this treatment as well as the different effect on diverse SCI populations is still unknown. Larger, controlled studies are still required to determine the appropriate candidates, optimal timing and best protocol design for the maximal efficacy of robotic locomotor therapy in SCI patients.
References
Waters RL, Adkins RH, Yakura JS . Motor and sensory recovery following incomplete paraplegia. Arch Phys Med Rehabil 1994; 75: 67–72.
Eng J, Teasell R, Miller W, Wolfe D, Townson A, Aubut JA et al. Spinal Cord Injury Rehabilitation Evidence (SCIRE). www.icord.org/scire/pdf/SCIRECOMPLETE.pdf 2006.
Waters RL, Adkins R, Yakura J, Vigil D . Prediction of ambulatory performance based on motor scores derived from standards of the American Spinal Injury Association. Arch Phys Med Rehabil 1994; 75: 756–760.
Piepmeier JM, Jenkins NR . Late neurological changes following traumatic spinal cord injury. J Neurosurg 1988; 69: 399–402.
Tchvaloon E, Front L, Gelernter I, Ronen J, Bluvshtein V, Catz A . Survival, neurological recovery and morbidity after spinal cord injuries following road accidents in Israel. Spinal Cord 2008; 46: 145–149.
Gittler MS, McKinley WO, Stiens SA, Groah SL, Kirshblum SC . Spinal cord injury medicine. 3. Rehabilitation outcomes. Arch Phys Med Rehabil 2002; 83: S65–S71.
Wernig A, Muller S, Nanassy A, Cagol E . Laufband therapy based on ‘rules of spinal locomotion’ is effective in spinal cord injured persons [published erratum in: Eur J Neurosci 1995;7:1429]. Eur J Neurosci 1995; 7: 823–829.
Dietz V, Wirz M, Curt A, Colombo G . Locomotor pattern in paraplegic patients: training effects and recovery of spinal cord function. Spinal Cord 1998; 36: 380–390.
Dobkin B, Apple D, Barbeau H, Basso M, Behrman A, Deforge D et al. Weight-supported treadmill vs over-ground training for walking after acute incomplete SCI. Neurology 2006; 66: 484–493.
Colombo G, Joerg M, Schreier R, Dietz V . Treadmill training of paraplegic patients with a robotic orthosis. J Rehabil Res Dev 2000; 37: 693–700.
Jezernik S, Schärer R, Colombo G, Morari M . Adaptive robotic rehabilitation of locomotion: a clinical study in spinally injured individuals. Spinal Cord 2003; 41: 657–666.
Hesse S, Schmidt H, Werner C . Machines to support motor rehabilitation after stroke: 10 years of experience in Berlin. J Rehabil Res Dev 2006; 43: 671–678.
Regnaux JP, Saremi K, Marehbian J, Bussel B, Dobkin BH . An accelerometry-based comparison of 2 robotic assistive devices for treadmill training of gait. Neurorehabil Neural Repair 2008; 22: 348–354.
Colombo G, Wirz M, Dietz V . Driven gait orthosis for improvement of locomotor training in paraplegic patients. Spinal Cord 2001; 39: 252–255.
Wirz M, Zemon DH, Rupp R, Scheel A, Colombo G, Dietz V, Hornby TG . Effectiveness of automated locomotor training in patients with chronic incomplete spinal cord injury: a multicenter trial. Arch Phys Med Rehabil 2005; 86: 672–680.
Hornby TG, Zemon DH, Campbell D . Robotic-assisted, body-weight-supported treadmill training in individuals following motor incomplete spinal cord injury. Phys Ther 2005; 85: 52–66.
Hornby TG, Campbell DD, Zemon DH, Kahn JH . Clinical and quantitative evaluation of robotic-assisted treadmill walking to retrain ambulation following spinal cord injury. Top Spinal Cord Inj Rehabil 2005; 11: 1–17.
Nooijen CF, Ter Hoeve N, Field-Fote EC . Gait quality is improved by locomotor training in individuals with SCI regardless of training approach. J Neuroeng Rehabil 2009; 6: 36–46.
Holden MK, Gill KM, Magliozzi MR . Gait assessment for neurologically impaired patients. Phys Ther 1986; 66: 1530–1539.
Ditunno Jr JF, Barbeau H, Dobkin BH, Elashoff R, Harkema S, Marino RJ . Validity of the walking scale for spinal cord injury and other domains of function in a multicenter clinical trial. Neurorehabil Neural Repair 2007; 21: 539–550.
Catz A, Itzkovich M, Agranov E, Ring H, Tamir A . SCIM–spinal cord independence measure: a new disability scale for patients with spinal cord lesions. Spinal Cord 1997; 35: 850–856.
Catz A, Itzkovich M, Steinberg F, Philo O, Ring H, Ronen J et al. The Catz-Itzkovich SCIM: a revised version of the Spinal Cord Independence Measure. Disabil Rehabil 2001; 23: 263–268.
Mehrholz J, Kugler J, Pohl M . Locomotor training for walking after spinal cord injury. Cochrane Database Syst Rev 2008; (2) CD006676.
Swinnen E, Duerinck S, Baeyens JP, Meeusen R, Kerckhofs E . Effectiveness of robot-assisted gait training in persons with spinal cord injury: a systematic review. J Rehabil Med 2010; 42: 520–526.
Wirth B, van Hedel HJ, Kometer B, Dietz V, Curt A . Changes in activity after a complete spinal cord injury as measured by the Spinal Cord Independence Measure II (SCIM II). Neurorehabil Neural Repair 2008; 22: 145–153.
Zwerling C, Daltroy LH, Fine LJ, Johnston JJ, Melius J, Silverstein BA . Design and conduct of occupational injury intervention studies: a review of evaluation strategies. Am J Ind Med 1997; 32: 164–179.
Acknowledgements
This work was supported by a grant from the Israeli Ministry of Health, grant 3–3161.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Schwartz, I., Sajina, A., Neeb, M. et al. Locomotor training using a robotic device in patients with subacute spinal cord injury. Spinal Cord 49, 1062–1067 (2011). https://doi.org/10.1038/sc.2011.59
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2011.59
Keywords
This article is cited by
-
Settings matter: a scoping review on parameters in robot-assisted gait therapy identifies the importance of reporting standards
Journal of NeuroEngineering and Rehabilitation (2022)
-
Advanced rehabilitation technology in orthopaedics—a narrative review
International Orthopaedics (2021)
-
Increased gait variability during robot-assisted walking is accompanied by increased sensorimotor brain activity in healthy people
Journal of NeuroEngineering and Rehabilitation (2019)
-
Robotic assisted gait as a tool for rehabilitation of individuals with spinal cord injury: a systematic review
Journal of NeuroEngineering and Rehabilitation (2017)
-
Ankle voluntary movement enhancement following robotic-assisted locomotor training in spinal cord injury
Journal of NeuroEngineering and Rehabilitation (2014)