Abstract
Study design:
Description of a technique and prospective follow-up study.
Objectives:
The aim of this study was to present our experience in the surgical treatment of ischial pressure sores, especially recurrence.
Setting:
The Department of Plastic and Reconstructive Surgery and Spinal Injuries Unit, CTO Hospital, Rome, Italy.
Methods:
From 1995 to 1997, the authors used in 12 consecutive paraplegic patients, who had a grade III or IV decubitus ulcer in the ischial area only, two different and independent flaps coupled together in a ‘criss-cross’ musculocutaneous flap: a split-muscle gluteus maximus flap and a rhomboid fasciocutaneous local flap. The average follow-up period was 3 years and 9 months. Details of the operative procedure are presented to prove that this criss-cross closure of the ischial pressure sore beneficial for patients with spinal cord injury.
Results:
All flaps survived; recurrence of the decubitus ulcer occurred in one patient (8%). Pressure-sore-free survival after surgery was 20 months in the patient with recurrence and an average of 26 months in patients without recurrence.
Conclusion:
The results obtained confirm this procedure to be safe and useful. We believe this technique to be a valuable alternative for the reconstruction of primary or recurrent ischial pressure ulcers.
Similar content being viewed by others
Introduction
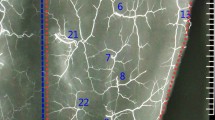
Early and stable reconstruction of deeply located grade III and IV pressure sores is of primary importance for the plastic surgeon, because recurrences can be prevented and early rehabilitation programs can be started. Persistent pressure above a certain threshold in the end capillary arterioles, in combination with other provoking factors such as anatomical location, immobility, infection and associated medical problems, will cause pressure sores in bedridden patients. Ideally, pressure sores should be treated with well-vascularized tissues. A number of various fasciocutaneous and musculocutaneous flaps have been described for the reconstruction of tissue affected by pressure sores. Gluteus maximus musculocutaneous flaps are among the well-defined and frequently used flaps. However, the risk for late recurrences of sores, especially of ischial sores, remains throughout the life of a paraplegic patient. Paraplegic patients may require several flaps during their lifetimes for the closure of ischial pressure ulcers. In its surgical management, it is very important to discuss the long-term results as well as the type of flap closure. In our series, we used a different technique in which other surgical options have failed: the association of two independent flaps, a transposed fasciocutaneous flap and a rotated split-muscle gluteus maximus flap. We assumed that simple rotational flaps, either fasciocutaneous or musculocutaneous, can be insufficient when the area to be repaired is under repeated mechanical stress, such as the ischial area, because of their unique source of vascular supply. Thus, we surmised that coupling two flaps with the vascular source derived from different and independent anatomical planes (that is, the superficial fasciocutaneous and the deeper muscular) (Figure 1) reduces the sensitivity to impacts, prompting an easier and faster healing of both microtraumas and macrotraumas with a more widespread and increased blood supply.
Materials and methods
Between September 2000 and August 2003, 12 consecutive cases of patients with ischial pressure sores grade III or IV, according to the classification of Shea, were treated with the ‘criss-cross’ musculocutaneous flap, with one flap for each sore. There were ten men and two women, with a mean age of 52 years (range, 17–85 years). The patients were paraplegic with a decubitus ulcer in the ischial area only. Seven patients had recurrent ulcers, three patients had diabetes mellitus and one patient had chronic renal failure treated with dialysis. Each patient received perioperative antibiotics, starting 3 days before surgery using teicoplanin 200 mg intravenously once a day and ceftazidime 1 g intravenously twice a day, and continuing for 10 days after surgery. During the postoperative period, dressings were changed daily, and the drains were kept in place for 7–10 days. Sutures were removed, on an average, on postoperative day 15. At 4 weeks after surgery, a physical therapy program was started for the range of motion of the lower extremities.
Surgical technique
The patient was placed in a prone position on the operating table with hips elevated and flexed, and a temporary anal purse-string suture was placed to prevent fecal contamination during the procedure. We designed a rhomboid rotation flap from a well-vascularized area of the posterior thigh skin, with the main axis encompassing the ulcer and parallel to the inferior gluteal fold (Figure 2a). The ulcer was stained with methylene blue, the margins to be excised were marked, and the decubitus ulcer was excised along with granulation tissue and surrounding bursa until viable bone was reached. The ischial tuberosity was conservatively reduced and rasped to a smooth contour.
A 55-year-old paraplegic man affected by an ischial pressure sore. (a) Preoperative view. We designed on the skin a rhomboid rotation flap from a well-vascularized area of the posterior thigh skin, with the main axis encompassing the ulcer and parallel to the inferior gluteal fold. (b) First intraoperative view. The gluteus maximus muscle was split and rotated on the residual bone. (c) Second intraoperative view. The rhomboid fasciocutaneous flap was transposed over the split-muscle flap. (d) Final intraoperative view. Result after skin closure. (e) Postoperative view. Result after 3 years and 3 months.
A proximally based thigh flap was designed. Two triangular flaps from the area of the rhomboid flap already drawn were elevated, and the semimembranosus-semitendinosus muscles, biceps femoris muscle and lower and medial parts of the gluteus maximus muscle were identified. The main belly of the gluteus muscle was split, starting from the inferior medial border, with the dissection parallel to the desired bulk of muscle fibers, to fill the gap left by removal of the ulcer. The result was a muscle flap isolated on the avascular plane over the ischial insertions of the semitendinosus-semimembranosus muscles. Flap shape and dimensions varied according to the defect. The gluteal flap was rotated on the residual bone of the previous ischial ulcer area (Figure 2b) and anchored to the periosteum with stitches using a 3-0 polydioxanone suture.
The last step was to transpose the previously designed, independent rhomboid fasciocutaneous flap over this muscular flap (Figures 2c and d). An important point in flap design is to consider donor-site closure; the donor site can be closed directly, even after large flap transpositions, considering the fact that a flap larger than 8 × 18 cm creates difficulty in the primary closure of the donor site.
We certify that all applicable institutional and governmental regulations with regard to the ethical use of human volunteers were followed during the course of this research.
Results
Twelve ischial wound closures were performed using this ‘criss-cross’ musculocutaneous flap. This method of reconstruction has validly been applied for ischial sores as wide as 13 × 9 cm and, in every case, it has appropriately and easily covered the ischial tuberosity, the main purpose of these reconstructions.
The average operative time was 2 h. Every flap survived; however, two distal cutaneous partial necroses of the flaps occurred, which were treated using hyaluronic acid skin substitutes and healed. In one patient, suture dehiscence at the wound edges occurred, and the wound was resutured. A hematoma under the flap with wound dehiscence occurred in a patient with diabetes. After serial drainage procedures, the flap was raised again and, resecting the pseudocapsule without damaging the vascularization, the flap was sutured secondarily. The flap healed completely after the second procedure.
Patients were not allowed to lie or sit on their flaps for 3 weeks after the operation. During follow-up, evidence of pressure sore recurrence was obtained by means of direct patient interview at an outpatient clinic or mail/telephone interview. After an average follow-up of 3 years and 9 months (ranging from 9 months to 5 years and 7 months), there has been no recurrence of ulcer in 11 of the 12 closures. One recurrence (8%) was observed in a patient who did not follow the physical therapy program guidelines. This patient refused a second procedure that we proposed. Pressure-sore-free survival after surgery was 20 months in the patient with recurrence and an average of 26 months in patients without recurrence (Figure 1e).
Discussion
Managing ischial pressure sores from a well-vascularized flap is still a challenging problem for the reconstructive surgeon. Despite various surgical methods described in literature, the rate of recurrence is high.1, 2, 3, 4 Repeated recurrence of sores sometimes occurs in patients who pay no attention to instructions regarding pressure sores and in others who have treatment complications. Yamamoto et al.5 described a higher recurrence rate for ischial sores than for sacral sores.
Ideally, pressure sores should be treated with well-vascularized tissues such as muscle and musculocutaneous flaps that, for this reason, remain reliable options. Muscle and musculocutaneous flaps have been used successfully for their excellent blood supply and durability.6, 7, 8 Gluteus maximus musculocutaneous flaps are among the most well-defined and frequently used flaps, although their use is not without drawbacks.9, 10 Use of the entire gluteus maximus muscle results in functional deficits and possible functional losses, interfering with future physical therapy.11, 12 Muscle atrophy arises as a major problem in bedridden patients, and these patients require early physical therapy. Using partial-thickness gluteus maximus muscle precludes functional loss. The major advantage of this technique is preservation of most of the gluteus maximus muscle for stair climbing and single-limb support in the ambulatory patient;13, 14 however, some authors advocate using partial muscle mass in paraplegic patients as well, to avoid or delay recurrence of the decubitus ulcer.15 Nevertheless, fasciocutaneous and the most recent fasciocutaneous perforator flaps have been used successfully and, for some authors, with a lower rate of recurrence.16, 17, 18, 19, 20 The type of myocutaneous or fasciocutaneous flap that should be used is still disputed.
Our main purpose was to identify an effortless and effective surgical method to approach either primary or secondary ischial ulcers in paraplegic patients, to combine the advantages of both fasciocutaneous and muscle flaps by using two different and independent flaps. The two flaps are coupled in a ‘criss-cross’ musculocutaneous flap, using a split-muscle gluteus maximus flap raised from its caudal edge and a fasciocutaneous local flap designed as a rhomboid flap. According to this approach, the muscle flap was shaped to fill the gap of tissue created by removal of the ulcer. The increased blood supply to the bone controls residual infection and reduces tissue hypoxia due to the mechanical stress of the patient's prolonged sitting position. The fasciocutaneous flap was used to strengthen tissue closure by moving in a thick pad of tissue to replace the superficial layers lost because of the decubitus ulcer and its debridment. The rhomboid flap was chosen because the resulting scar is well oriented and does not affect the patient while sitting and pressing on the ischial area. Furthermore, the rhomboid flap allows a reproducible pattern adequate to the requirements of physical therapy and adequate to the prolonged sitting position. Other advantages of the ‘criss-cross’ musculocutaneous flap are that even if it is a combination of two flaps, the technique is still easy to perform and relatively quick. In addition, this technique uses flaps that are local, the dissection required is minimal and other flap options are preserved. Last but not the least, the independence of blood supply sources of the inner and outer flaps of the ‘criss-cross’ technique makes the flap more resilient and more resistant to the adverse factors that chronically weaken the tissues in the ischial area and that are responsible for the failure of the classic techniques used. The major limitation of this technique, apart from patients who cannot follow the physical therapy program guidelines, is that it excludes patients with multiple ulcers, sores bigger than 13 × 9 cm and patients who have scars (that is, previous surgery) that make impossible the elevation and/or transposition of the rhomboid fasciocutaneous flap over the muscular flap.
The results obtained, with 8% recurrence and an average pressure-sore-free survival after surgery of 26 months, confirm that this procedure is safe and useful. We have found this ‘criss-cross’ musculocutaneous flap to be a valuable alternative for the reconstruction of primary or recurrent ischial pressure ulcers.
References
Relander M, Palmer B . Recurrence of surgically treated pressure sores. Scand J Plast Reconstr Surg 1988; 22: 89–92.
Disa JJ, Carlton JM, Goldberg NH . Efficacy of operative cure in pressure sore patients. Plast Reconstr Surg 1992; 89: 272–278.
Mandrekas AD, Mastorakos DP . The management of decubitus ulcers by musculocutaneous flaps: a five-year experience. Ann Plast Surg 1992; 28: 167–174.
Rimareix F, Lortat-Jacop A . Comparative study of 2 surgical techniques in the treatment of ischial pressure ulcers in paraplegic patients: retrospective study of 90 cases. Ann Chir Plast Esthet 2000; 45: 589–596.
Yamamoto Y, Tsutsumida A, Murazumi M, Sugihara T . Long-term outcome of pressure sores treated with flap coverage. Plast Reconstr Surg 1997; 100: 1212–1217.
Mathes SJ, Alpert B . Advances in muscle and musculocutaneous flaps. Clin Plast Surg 1980; 7: 15–26.
Hurteau JE, Bostwick J, Nahai F, Hester R, Jurkiewicz MJ . V-Y advancement of hamstring musculocutaneous flap for coverage of ischial pressure sores. Plast Reconstr Surg 1981; 68: 539–542.
Angrigiani C, Grilli D, Siebert J, Thorne C . A new musculocutaneous island flap from the distal thigh for recurrent ischial and perineal pressure sores. Plast Reconstr Surg 1995; 96: 935–940.
Fisher J, Arnold PG, Waldorf J, Woods JE . The gluteus maximus musculocutaneous V-Y advancement flap for large sacral defects. Ann Plast Surg 1983; 11: 517–522.
Stevenson TR, Pollock RA, Rohrich RJ, Vanderkolk CA . The gluteus maximus musculo-cultaneous island flap: refinements in design and application. Plast Reconstr Surg 1987; 79: 761–768.
Parkash S, Banerjee S . The total gluteus maximus rotation and other gluteus maximus musculocutaneous flaps in the treatment of pressure ulcers. Br J Plast Surg 1986; 39: 66–71.
Jósvay J, Sashegyi M, Kelemen P, Donáth A . Clinical experience with the hatchet-shaped gluteus maximus musculocutaneous flap. Ann Plast Surg 2005; 55: 179–182.
Baran CN, Celebioğlu S, Civelek B, Sensöz O . Tangentially split gluteus maximus myocutaneous island flap based on perforator arteries for the reconstruction of pressure sores. Plast Reconstr Surg 1999; 103: 2071–2077.
Gould WL, Montero N, Cukic J, Hagerty RC, Hester TR . The ‘split’ gluteus maximus musculocutaneous flap. Plast Reconstr Surg 1994; 93: 330–336. Comment in Plast Reconstr Surg. 1995; 95: 941–942.
Ramirez O, Swartz WM, Futtrell JW . The gluteus maximus muscle: experimental and clinical considerations relevant to reconstruction in ambulatory patients. Br J Plast Surg 1987; 40: 1–10.
Yamamoto Y, Ohura T, Shintomi Y, Sugihara T, Nohira K, Igawa H . Superiority of the fasciocutaneous flap in reconstruction of sacral pressure sores. Ann Plast Surg 1993; 30: 116.
Ichioka S, Okabe K, Tsuji S, Ohura N, Nakatsuka T . Triple coverage of ischial ulcers with adipofascial turnover and fasciocutaneous flaps. Plast Reconstr Surg 2004; 114: 901–905.
Coşkunfirat OK, Ozgentaş HE . Gluteal perforator flaps for coverage of pressure sores at various locations. Plast Reconstr Surg 2004; 113: 2012–2017; discussion 2018-9.
Aydin G, Zekeriya K, Zafer O . Long-term outcome with the adductor perforator flap for ischial pressure sores. Plast Reconstr Surg 2008; 122: 49e–50e.
Homma K, Murakami G, Fujioka H, Fujita T, Imai A, Ezoe K . Treatment of ischial pressure ulcers with a posteromedial thigh fasciocutaneous flap. Plast Reconstr Surg 2001; 108: 1990–1996; discussion 1997.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Borgognone, A., Anniboletti, T., De Vita, F. et al. Ischiatic pressure sores: our experience in coupling a split-muscle flap and a fasciocutaneous flap in a ‘criss-cross’ way. Spinal Cord 48, 770–773 (2010). https://doi.org/10.1038/sc.2010.25
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2010.25
Keywords
This article is cited by
-
Fasciocutaneous and/or myocutaneous flaps versus perforator flaps: systematic review and meta-analysis for reconstruction of ischial pressure sores
European Journal of Plastic Surgery (2020)
-
The use of a combined profunda femoris perforator-based fasciocutaneous flap and gracilis muscle flap in the treatment of ischial pressure wounds in patients with limited mobility
European Journal of Plastic Surgery (2019)