Abstract
Study design:
Longitudinal audit.
Objectives:
To develop evidence-based maps of rehabilitation for different lesion categories.
Setting:
Midlands, UK.
Methods:
Over a 5-year period data for all newly injured neurologically damaged patients aged 18 years or more were collected and analyzed (n=280). Data were collected from a functional independence measure (the Needs Assessment Checklist), patient records (paper and electronic) and patient goal planning records. The patients were grouped into different lesion categories. Standard milestones that patients in a given category would be expected to reach in rehabilitation were identified using goals set at goal planning meetings. Time when patients reached these milestones and variation between patients around time in reaching these milestones were calculated.
Results:
Median times from onset to admission, onset to rehabilitation and length of rehabilitation are given. Pictorial representations of rehabilitation (rehabilitation maps) were produced, using goals identified, median times of achievement and variation. This paper provides examples of these maps from one particular group, T8–T12 Frankel A.
Conclusion:
Pathways of care can be used in a number of ways: to identify the need for service change; to audit service change; to provide evidence-based expectations for staff, patients and external parties; to look at variances affecting care; to make this service transparent; to provide figures for comparison with other philosophies of care; and to ensure consistency across the service.
Similar content being viewed by others
Introduction
A process map is a ‘picture’ of a plan of care.1 It outlines a care process, identifying milestones and placing these in a timeframe, indicating what patients may cover in rehabilitation and in what time scale. This makes complex medical pathways clearer.
Spinal cord injury (SCI) rehabilitation is complex, and is difficult for those new to the process to understand easily. Maps help to define the process and are useful for anyone outside or new to the rehabilitation service, including patients, relatives, new staff,2 commissioners and international colleagues. For patients, knowledge of the journey's steps and stages reduces anxiety and fear.2 Evidence-based statistical predictions of rehabilitation progress are useful for discharge planning.
The complexity of rehabilitation presents challenges when producing process maps. Differences in level and completeness of injury affect rehabilitation and independence potential, and therefore result in considerable variation in the rehabilitation path. Maps produced must reflect this. There can also be wide variation within lesion categories. Variation may be due to a range of factors. Identifying and adjusting features affecting progress is one aim of process mapping. The effects of internal programme factors3 are manipulable and therefore potentially minimizable. Non-programme or ‘exogenous’4 factors, such as the age of the patient, are beyond programme control. Considerable variation makes mapping for SCI more difficult than for other care processes with greater standardization. Variation also reduces the usefulness of maps, as averages are less applicable to individual patients. These two factors may explain why, although integrated care pathways are not a new concept,5 they have not been well developed in spinal injuries in the United Kingdom.
Different types of care maps can be produced, as determined by their purpose. If mapping the whole of rehabilitation, the map produced would be broad. Care can be mapped through reflection on accepted best practice, using simulations of patient journeys6 or using analysis of evidence of past patient journeys.2 Maps may describe an ideal rehabilitation path experienced without complications or limitations, or maps may describe the average rehabilitation path experienced in reality. The ‘ideal patient’ without any complicating factors is the exception not the norm, and expectations based on ideal maps may be less helpful.
The first step towards developing care maps for SCI rehabilitation was taken by Duff et al.7 They created maps of current rather than ideal care, using data from their goal planning system. This study was limited by small sample size (n=63). Individual variance might therefore have had a disproportionate impact, particularly for categories with small numbers (for example, n=4 for Category C4, Frankel A–C). Also, within lesion categories there was no differentiation between different levels of completeness, except placing those with Frankel grade D injuries in a separate category. Second issue was a systematic bias in patient selection. All patients included in the study were working with a clinical psychologist. This could indicate potential psychological or behavioural issues, which could impede progress, thereby biasing the averages found. Our study was set out to improve on these care maps.
This study aimed at producing care maps of the rehabilitation service at the Midland Centre for Spinal Injuries. This was primarily for clinical purposes: to give patients and their families realistic expectations about what could be achieved for their level of injury, and when; and to support new staff in understanding the rehabilitation process. Secondarily, care maps would be useful for service development and commissioning. They would be the first step in creating service templates for rehabilitation, supporting strategic service planning to prevent bottlenecks. They could highlight variation as a step towards its reduction. Care maps could provide information and transparency for commissioners. In the United Kingdom, blocks of care from supra-regional services such as specialist spinal injury centres are commissioned by consortia of primary health-care teams. Care maps could enable commissioners to understand the rehabilitation process more clearly and hold realistic expectations of performance based on data collected from the service.
Materials and methods
Setting
These process maps were developed at the Midlands Centre for Spinal Injuries (MCSI), UK. The MCSI is a 44 bed specialist Spinal Injuries Centre offering acute, rehabilitation and outpatient services. It implements a philosophy of conservative management of SCI, and offers a service for life from injury. This includes outpatient reviews initially at 6 weeks and then increasing over time to an ongoing 2-year review, consisting of multidisciplinary management of multisystem dysfunction following SCI.
Participants and inclusion criteria
In this study n=280 participants. Participants who fell under the inclusion criteria were adults (over 18 years) and newly injured on their initial admission to MCSI from 1 January 2000 to 1 January 2005. Patients who fell under the exclusion criteria were as follows:patients on first admission but not newly injured and those who were neurologically intact.
Design
The study used a longitudinal design across 5 years. Basic descriptive data of the patient journey were calculated for all participants, including time between injury and admission and time in acute specialist care before rehabilitation.
Where goal planning took place, the rehabilitation process was measured. Maps of goals achieved and the times for goal achievement were produced, according to lesion category.
Procedure
Patients were categorized by lesion level and Frankel grade on admission (Table 1). Rehabilitation maps were produced for each category. Frankel grades were used as these were systematically recorded as part of clinical process. There were no patients of the category C4 Frankel D.
Rehabilitation was measured using the patient notes, Needs Assessment Checklist (NAC) and goal planning sheets. Details of patient dates of injury, level of injury, admission and discharge from the MCSI were sourced from patient notes. The NAC8, 9 is an SCI-specific measure of independence outcomes covering all areas of rehabilitation. The first administration of the NAC was used as the marker of the beginning of rehabilitation. It is a policy for the NAC to be taken within the first 2 weeks following mobilization, or for those unable to mobilize (for example, due to pressure sores), when the patient enters the goal planning system. The NAC is also administered within 3 weeks of the end of rehabilitation. The end of rehabilitation is defined as discharge, or in the case of delayed discharge, as the last goal-setting meeting plus 2 weeks to meet outstanding goals. ‘Delayed discharge’ is where a patient remains at the MCSI when rehabilitation is complete due to lack of available community placement.
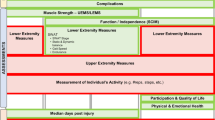
The NAC structures rehabilitation into a number of domains and subdomains (see Table 2) and these were used to structure the maps into sections. Information about patient progress in rehabilitation was identified through the goal planning system. The goal planning system is based on that developed at the National Spinal Injuries Centre.10 Patients have a fortnightly meeting with their individual rehabilitation team, at which specific goals are set and a plan for the following fortnight is produced (a goal sheet). Goal sheets from each lesion category were reviewed, with goals assigned to rehabilitation domains and used to produce the list of goals in each map. At each meeting, goal achievement for the previous 2 weeks is reviewed. This information describes when goals were achieved.
Not every patient in a lesion category had goal sheets. The number of participants who actually had goal sheets is indicated in Table 3. It is from these patients that the maps were produced. Of those patients who did have goal sheets, not every patient had every goal listed. This is likely to be due to the individualized nature of the goal planning process. Goals are not standardized, rather being generated on an individual basis for each patient, depending on their specific needs. The times given for each goal are only based on those patients who had this particular goal listed.
Times were calculated in weeks. For each goal the median and interquartile range (IQR) times at which that goal was started and achieved were found. These measures of central tendency and variation were used because the mean and the s.d. were highly affected by extreme values.
Results
Fifty-one patients did not go through the goal planning process. Reasons for this are not consistently recorded. However, some were transferred elsewhere for rehabilitation, such as to rehabilitation units for the elderly. Others, though showing neurological deficit on admission, may have improved on bed rest to the extent that they did not go into goal planning.
Median time periods from onset to admission, onset to rehabilitation, admission to rehabilitation and length of rehabilitation were calculated for each lesion category (Table 4). The IQR for length of rehabilitation is also shown. Onset to rehabilitation, admission to rehabilitation and length of rehabilitation could only be calculated for those who went through the goal planning process. To provide a figure for comparison, onset to admission was calculated twice: once for all participants, and again for those with goal sheets only.
Two types of care map were produced. Only examples of each type of map are provided here. Full data are available as Supplementary Information. One type shows all the goals for a given lesion category with median start and achievement times. An example of part of such a map is given in Figure 1. In the map, the black arrows run from the median start time to the median achievement time for each goal. The second type of map shows each rehabilitation domain individually including the variation around median start and achievement times. An example of this is given in Figure 2. Again, in these maps black arrows run from median start time to median achievement time. Lines with circle ends show variation. They run from the beginning of the IQR for the start time (when 25% of those with this as a goal have begun working towards this goal) to the end of the IQR for the achievement time (when 75% of those with this as a goal have achieved this goal). In the Supplementary Information, all data for all lesion categories are provided.
Discussion
This study aimed at producing realistic maps of rehabilitation to develop realistic expectations for patients and families, to support the learning of new staff and to support commissioning of services. Data about the median time from onset to admission, from admission to rehabilitation and length of rehabilitation were given. Examples of the rehabilitation maps produced are provided. The median rehabilitation path as followed by real patients was mapped, using data collected from one service. By including variations, the maps offer realistic expectations of progress within this system. Maps reflecting the actual experience of service users are useful to subsequent patients who pass through the service.
This study improves on the Duff et al. study7 because it had a much larger number of patients (n=280). Such large and detailed bodies of data are unusual in this field. The Uniform Data System11 and the clinical outcome data from the Model Systems12 are other examples. With a larger number of patients than in the Duff et al.7 study, there was no need to assume parity across Frankel grades. However, once categories were divided by Frankel grade, this study also suffered from small numbers in some categories. This study also improves on Duff et al. by excluding a potential systematic bias, as our information has been collected across the whole rehabilitation service. Finally, it is a longitudinal study rather than a retrospective study.
This study has some limitations. It utilizes Frankel grades from neurology checks taken on admission. One improvement would be to use a neurology measure taken at the beginning of rehabilitation for categorization, as neurology may change in the time between admission and rehabilitation. This could have implications for the functional level achievable by patients, reducing the comparability of patients within the lesion categories used in this study. Second, the use of ASIA grades would provide standardized scales with greater international acceptability. Precision could be improved by recording exactly when a goal was completed, rather than waiting for the next goal planning meeting. Greater standardization of the way that goals are written would be helpful in data comparison and would improve the development of care maps. However, this pulls against the individualized, patient-centred philosophy at the core of the goal planning approach to rehabilitation.10 The desire and need to standardize for research purposes must be balanced against clinical need and benefit of the intervention for the particular patients served.
These care pathways include information about time variation. They could therefore be used to support a warning system for patients falling behind. On the basis that past achievement is a reasonable benchmark for future expectations, the IQR could be said to represent a time period for ‘reasonable variation’ around start and achievement times. If patients take longer to start or achieve their goals than the 75th percentile, then that could be flagged up as a particular problem for action.
Accurate maps of the current process are an important first step in minimizing variation and delay in the rehabilitation process. Arguably, the shorter end of the IQR (that is, the 25th percentile) represents a reasonable time to aim at for improvement of services at this unit, as a time achieved with a reasonable number of patients. However, categorization was determined by neurology on admission. By the start of rehabilitation, neurology may have improved, such that the lower end of the IQR may in some cases be misrepresentative, particularly where movement is more likely, such as with the incomplete lesions. In the future, reasons for variation around the care pathway may be examined using information collected as part of the goal planning audit about reasons for non-achievement of goals. Identifying reasons for variation is the second step in minimizing them.
These care maps can be used to inform the development of an integrated care pathway. Care pathways are frequently produced in the form of a structured, evidence-based plan of care, which forms the complete clinical record.2 The first stage of integrated care pathway development is essentially a baseline review of current practice for the chosen group of patients,1 which these care maps constitute. Developing clinical care pathways for rehabilitation is one of the stated aims of the South of England Review Group.13 These care maps could be supplemented with current guidelines, expert opinion, protocols and evidence drawn from the literature to develop an integrated care pathway.
Conclusions
Care maps are an important step in describing rehabilitation and making it transparent for those new to or outside the service. Maps of the average rehabilitation process as experienced, including variations, are realistic and appropriate to many patients. They are difficult to produce for complex services, such as rehabilitation for SCI, where patients of any category are few and individual differences are many, and where the depth and detail of the data required is so great. These maps are a step forward in the production of care maps for SCI, and are the best currently available in the United Kingdom. Development of this work may include better maps, an early warning system for those struggling in rehabilitation and a systematic approach to minimizing negative variation in the system.
References
Middleton S, Barnett J, Reeves D . What is an Integrated Care Pathway? Hayward Medical Communications 2003, www.evidence-based-medicine.co.uk.
Layton A, Moss F, Morgan G . Mapping out the patient's journey: experiences of developing pathways of care. Qual Health Care 1998; 7 (supp): S30–S36.
Wakefield L . An integrated care pathway for diabetic ketoacidosis. Paediatr Nurs 2004; 16: 27–30.
Funnell S . Developing and using a program theory matrix for program evaluation and performance monitoring. In: Rogers P, Hacsi T, Petrosino A, Huebner T (eds). Program Theory in Evaluation: Challenges and Opportunities. New Dir Eval, Jossey Bass Publishers: San Francisco, CA, USA, Vol 87, 2000, pp 91–101.
De Luc K . Developing Care Pathways: the tool kit. Radcliffe Medical Press: Oxford, 2001.
Katsaliaki K, Brailsford S, Browning D, Knight P . Mapping care pathways for the elderly. J Health Organ Manag 2005; 19: 57–75.
Duff J, Evans MJ, Kennedy P . Goal planning: a retrospective audit of rehabilitation process and outcome. Clin Rehabil 2004; 18: 275–286.
Kennedy P, Hamilton LR . The needs assessment checklist: a clinical approach to measuring outcome. Spinal Cord 1999; 37: 136–139.
Berry C, Kennedy P . A psychometric analysis of the Needs Assessment Checklist. Spinal Cord 2003; 41: 409–501.
Kennedy P . Ecological evaluation of goal planning and advocacy in a rehabilitation environment for spinal cord injured people. Paraplegia 1991; 29: 197–202.
Uniform Data System for Medical Rehabilitation. www.usdmr.org.
Stover S, De Lisa JA, Whiteneck GG (eds). Spinal Cord Injury: Clinical Outcome from the Model Systems. Aspen: Maryland, 1995.
Joint Standard Development Groups of the South of England Review Group. Standards for Patients Requiring Spinal Cord Injury Care; http://www.secscg.nhs.uk/home/consortia/spinal-injuries/.
Acknowledgements
We thank Mr W El Masri, Dr D Short, Mr A Osman and Mr R J Chowdhury, other medical staff, all the nurses, occupational and physiotherapists, the resettlement team and generic workers for their support, participation and hard work in enabling the collection of data without which the publication of this paper would not have been possible.
Author information
Authors and Affiliations
Corresponding author
Supplementary information
Rights and permissions
About this article
Cite this article
Goodwin-Wilson, C., Watkins, M. & Gardner-Elahi, C. Developing evidence-based process maps for spinal cord injury rehabilitation. Spinal Cord 48, 122–127 (2010). https://doi.org/10.1038/sc.2009.94
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2009.94
Keywords
This article is cited by
-
Effect of a computerized decision support system on the treatment approach of stage III or IV pressure injury in patients with spinal cord injury: a feasibility study
BMC Health Services Research (2023)
-
The value of the whole picture: rehabilitation outcome measurement using patient self-report and clinician-based assessments after spinal cord injury
Spinal Cord (2022)
-
Pharmacologic and Acute Management of Spinal Cord Injury in Adults and Children
Current Treatment Options in Neurology (2022)
-
Challenges and potential improvements in the admission process of patients with spinal cord injury in a specialized rehabilitation clinic – an interview based qualitative study of an interdisciplinary team
BMC Health Services Research (2017)