Abstract
Study design:
Longitudinal analysis of SCI registry merged with VHA administrative-data and Medicare claims files (FY1999–2002).
Objectives:
To estimate the prevalence of mental illness (MI) and substance use disorders (SUDs) among veteran health administration (VHA) clinic users with spinal cord injuries (SCI) and examine subgroup variations by demographic, socioeconomic characteristics, and duration and level of SCI.
Setting:
VHA clinic users (N=8338) with SCI who were alive by the end of FY2002.
Methods:
ICD-9-CM codes were used to identify individual MI (anxiety disorders, bipolar, depressive disorders, psychoses, post-traumatic stress disorder (PTSD) and schizophrenia) and categories of SUDs (tobacco, alcohol and drug abuse). Chi-square tests and multinomial logistic regression were used to examine the demographic and socio-economic profile of VHA users with SCI and MI and/or SUD.
Results:
Over a 2-year period, 46% VHA users with SCI had either a MI or SUDs: 20% had MI only; 12% had SUD only and 14% had both. The most common MI was depressive disorder (27%) and tobacco use was highly prevalent (19%). African-Americans (versus whites) were less likely to be diagnosed with MI only. Increased duration of SCI lowered the likelihood of MI and/or SUDs. Mood and anxiety disorders were highly prevalent in veterans with SCI with chronic physical conditions such as diabetes, heart disease, hypertension, and respiratory diseases.
Conclusions:
Mental illness and SUDs are highly prevalent in the VHA population with SCI and is complicated by the high rates of chronic physical conditions, presenting challenges in their healthcare management
Similar content being viewed by others
Introduction
Individuals with spinal cord injury (SCI) may be considered at high risk for mental illness (MI) because of the negative consequences of SCI on physical and social functioning.1 Studies show elevated rates of MI among individuals with SCI,2 others challenge this notion. In one study, two-thirds of the study sample did not exhibit depressive or anxiety symptoms.3 Depression may vary over the course of the illness and be attenuated over time. Thus, evidence of higher prevalence of MI among SCI patients is inconclusive and a recent systematic review of psychological morbidity concluded that further clarification is needed concerning psychological consequences in SCI.4
Many veterans may be prone to post-traumatic stress disorder (PTSD), because of events in wartime.5 However, a comparison of individuals with and without SCI showed that neither tetraplegia or paraplegia nor trauma-recency was significantly correlated with PTSD symptoms though before trauma was implicated.6 In fact, rates of trauma-related distress after SCI were comparable with those after other traumas;7 patterns of MI in individuals with SCI were not found to be significantly different from those without SCI.8
Although the rates of MI may not be higher in individuals with SCI compared with the general population, individuals are at increased risk for substance use disorders (SUD).1 Community-based studies reported alcohol (21%) 9 and marijuana (16%)9 use, and SUD (52%) 10 during the post-injury period. It is not clear from these studies as to whether SUD was a problem premorbidly that led to the SCI itself, however, Fullerton et al.11 did find evidence of premorbid psychiatric illness (hypomania and depression) and alcohol abuse related to the accident. There is also some evidence on the relationship between SUD and medical complications among individuals with SCI. Using National Institute of Disability Research and Rehabilitation (NIDRR) Model SCI systems data, it has been shown that among individuals with SCI, pressure ulcers and SUD are related.10
Spinal cord injury is a life-long condition requiring ongoing healthcare management. Although the common post-injury secondary complications are urinary tract infections (UTI) and decubitus ulcers,2 the natural aging process with SCI increases the risk of developing cardiac complications and high blood pressure. Individuals with SCI compared with age-matched controls from the general or non-disabled population have a higher incidence of hypertension and ischemic heart disease. Earlier findings from the NIDRR data show that heart disease is the leading cause of mortality (35–46%) for patients surviving >30 years after SCI and among those over age 60.12 Age-adjusted cardiovascular disease mortality rates in the SCI population are more than double the rates in the non-disabled population.
Spinal cord injury and the veteran population
In the veteran population, SCI is highly prevalent with 42 000 veterans being eligible for medical care and other benefits within the Veteran Health Administration (VHA).13 However, information on the types of MI and their prevalence in the veteran population is scarce.
There are no nation-wide studies that are current in documenting the prevalence or the co-occurrence of MI and SUD among SCI-veterans. Often MI and SUDs co-occur, and are highly prevalent in the veteran population.14 There is also growing evidence of co-occurring medical illnesses in those with a MI. For example, a review of literature based on 44 202 abstracts, notes that compared with the general population, individuals with schizophrenia have a higher prevalence of cardiovascular diseases, diabetes, and other diseases.15 Similarly, major depression is an established precursor for cardiovascular diseases, development of type 2 diabetes and hypertension. Depression has been related to adverse outcomes among those with SCI including lower functioning, reduced activity levels, and increased secondary medical complications.16
With the growing population of veterans with traumatic injuries, our study may be particularly useful for healthcare programs/services for this population. Co-occurring MI and SUDs (including tobacco use) in SCI-veterans is challenging in terms of care coordination and resource utilization. Further complicating care coordination is that many of these veterans are dually eligible, using both VHA and Medicare systems for their healthcare.
Therefore the primary aims of this study are to: (a) estimate the prevalence of MI and SUDs; (b) estimate rates of various types of MIs and SUDs; (c) examine the subgroup differences in MI and SUDs; and (d) explore the relationship between commonly occurring MI and physical disorders. These aims will be achieved by utilizing a multisystem and nation-wide data from the VHA, Medicare, and the Spinal Cord Dysfunction Registry (SCD-R) of the VHA.
Methods
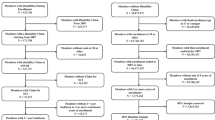
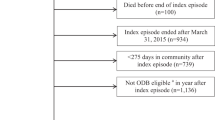
Veterans with SCIs or disorders
The SCD-R data consist of a cohort of SCI-veterans and related-disorders who utilize VHA for their care.17 It includes information about veterans including demographics, level and completeness of injury, etiology and date of onset (N=13 097 with valid date of SCI onset). These data were then merged with the VHA and Medicare claims data to obtain the demographic and other information regarding medical illnesses, MI and SUD conditions.
The dataset was a longitudinal cohort of veterans who had an outpatient face-to-face use of services or hospitalization either in VHA or Medicare facilities between 1999 and 2002. We excluded veterans who: (1) had no VHA or Medicare face-to-face encounters or hospitalization; (2) date of onset occurred later than FY 2001; and (3) died during or before the study began. Employing these exclusionary criteria provided us with a study population of 8338 SCI-veterans. Among these patients, 21% had missing data on race/ethnicity and 2% on marital status, region, urbanicity, and SCI severity. In multivariate analysis, we included missing indicators for these variables and every attempt was made to pick up SCI status and other details (missing from the registry) from the administrative data using International Classification of Diseases, 9th edition (ICD-9-CM) diagnosis codes.
Measures
Dependent variables
Mental illness and SUD categories: Mental illness was identified based on International Classification of Diseases, 9th edition (ICD-9-CM) codes (made by physicians and psychologists) occurring over a 2-year period between FY 2000-2001. MI included psychiatric conditions such as schizophrenia, depression, bipolar, other psychoses, anxiety and PTSD.
Substance use disorder included alcohol, drug, and tobacco use over a 2-year period between FY 2000 and FY 2001. SUD was also identified by using ICD-9-CM codes. For drug and alcohol use, we further distinguished between abuse, dependence, and other (that is, occasional use). Owing to high co-occurrence of both codes (dependence and abuse) and lower rates of only dependence (drug abuse 1% and alcohol abuse 2%), we combined dependence and abuse diagnoses into alcohol and drug use. MI/SUD categories were constructed broadly by combining MI and SUD to create four subgroups: (1) No MI/SUD; (2) MI only; (3) SUD only; and (4) both MI/SUD.
Independent variables
Demographics were gender, race/ethnicity, age and marital status and contextual variables were region and urbanicity (Table 1). The supplemental insurance variable consisted of Medicare Fee-For-Service (FFS) enrollment. Duration and level of SCI were also included. Owing to high levels of missing data in the registry (28%) regarding SCI level of injury, every attempt has been made to determine SCI status and other details from the administrative data (we now have only 2.4% missing).
We explored the complexity of medical conditions in SCI-veterans by examining diabetes, heart disease, hypertension, and chronic pulmonary disease (COPD) based on their higher prevalence and the commonly occurring SCI-specific conditions (UTI and pressure ulcers).1
Statistical procedures
Chi-square tests were used to examine the bivariate associations between MI/SUD categories and the independent variables. Multinomial logistic regression was used to analyze the predictors of the MI/SUD categories. As race (21%), marital status (2.0%) and geographic area (2.3%) had missing data, we also created a missing indicator for these variables and included them in the regression analysis (not shown).
Findings
Overall, 34% had a MI; the most common being depression (27%) followed by anxiety (10%) and PTSD (6%) (Table 1). Tobacco use was common (19%) followed by alcohol (9%) and drugs (8%).The majority of SCI-veterans (Table 2) were male (98%), and a large proportion of them were classified as service-connected disabled by the VHA (45%) or classified as low income (38%); 54% were paraplegic and 44% were tetraplegic.
Owing to smaller sample sizes for some MI and SUDs, we created three mutually exclusive categories of MI and/or SUD. Using this categorization, overall 20% had MI only, 12% had SUD only and another 14% had both (Table 2, col 3–10). Subgroup comparisons by the three MI/SUD categories showed that women veterans had higher MI and lower SUD, patients <50 years had higher MI/SUD, as did African-Americans and minorities compared with men, 75 plus years and white race.
In multivariate analysis (Table 3), controlling for all demographic, geographic and SCI-related factors, we found women were significantly more likely to have MI only with adjusted odds ratio (AOR=2.11, 95% CI (1.494–2.99)). Older individuals (age > 65 years) were less likely to have either SUD only or in combination with MI. For example, old individuals in the age group 75 or older were 43% less likely to have SUD –only (AOR=0.57) and 62% less likely to have MI/SUD (AOR=0.38) compared with those who were <50 years old.
Compared with whites, African-Americans had lower odds of having MI –only (AOR=0.74) and Latinos had lower odds of having SUD only (AOR=0.51). Other minorities had higher odds of having both MI/SUD compared with whites (AOR=1.92). Duration of SCI was negatively associated with the prevalence of MI or SUD or both. As the duration of SCI increased, the likelihood of MI or SUD either alone or in combination was lower. Similarly, paraplegics were more likely to have SUD only or MI/SUD.
Table 4 shows the highly prevalent chronic conditions in our population during the period of study. Substance abuse (26%), pressure ulcer (32%), hypertension (34%), and UTI (41%) were the most prevalent followed by heart disease (15%), diabetes (16%), and COPD (12%). Veterans with SCI also had multiple comorbidities with 77% suffering from one or more chronic physical conditions and with the majority (53%) having two more conditions (not shown). A higher proportion of those with diabetes (28%), COPD (25%), heart disease (31%), and UTI (24%) had MI compared with those without diabetes (19%), without COPD (20%), without heart disease (18%) and without UTI (18%).
As shown in Table 4, across all conditions mood and anxiety disorders were highly prevalent in individuals with physical illnesses compared with those without these physical illnesses. For example, among those with COPD, depression was almost twice as likely (41.2 versus 24.8%) as those without COPD. Similarly, among those with heart disease, anxiety disorders were almost twice as likely as those without heart disease (15.9 versus 8.8%). Across all the MIs, substance abuse was consistently twice as likely in depression (43 versus 21%) and anxiety (16 versus 8%), but three times as high in PTSD (12 versus 4%) compared with those who did not abuse substances. We did not find uniformly high rates of PTSD across all types of physical illnesses (Table 4).
Discussion
Among veterans with SCI, the prevalence of MI or SUD was high (47%) over a 2-year period, with 34% having any MI and 26% having any SUD. These figures are higher than the 15% reported by an earlier veteran-based study.8 However, the percentage of those with SCI and depression was comparable with those reported in a recent study of SCI-veterans over a 3-year period.18 Our findings showed that depression was the most common diagnosis in this population of veterans All other diagnoses were present in < 10% of the population. These findings suggest that regular screening of depression among SCI-patients may assist in the early detection and treatment.
We found many subgroup differences in the prevalence of MI/SUD; veterans with a longer duration of SCI were less likely to have any MI/SUDs. This finding is consistent with other studies that find patients may experience depressive symptomotolgy after the rehabilitation phase, but this abates over time. Rehabilitation for SCI is lengthy where the individual is in frequent contact with health professionals (for example, nurses, social workers, therapists) trained to recognize symptoms of depression or substance abuse for further evaluation. The professionals’ therapeutic interaction alone may facilitate adjustment. However, researchers have found in one study of SCI-veterans, that despite the fact that 22% of their sample of 3678 veterans received a depression diagnosis during at least one healthcare encounter (for example, visit for blood pressure monitoring, etc.) and 72% of those individuals received prescriptions for antidepressants, only 33% actually continued the antidepressant course for 6 months.14 This points to the need for targeted follow-up by clinicians to determine causes of non-compliance (that is, ineffectiveness, misdiagnosis) and also to ensure patient treatment compliance.
A noteworthy finding of our research was the lower likelihood of MI only in African-Americans possibly pointing to under-recognition of co-occurring mental conditions. Further examination of racial differences in unadjusted analyses without any other controls, also found the same pattern; no other significant differences existed between whites and African-Americans in the other two groups (SUD only or both MI/SUD). This is consistent with the findings in the general population which found more services for medications and less for mental conditions among African-Americans.19
We also found higher rates of mood and anxiety disorders among SCI-veterans and chronic physical conditions, and the likelihood of MI or SUD was dependent on the type of physical illness. Although those with diabetes were more likely to have MI only, we also found that those with both COPD and hypertension were more likely to have MI or SUD in all combinations. We also found higher rates of SUD across all types of MI examined. Further studies should be undertaken to understand the health services use and needs of this sub population for adequate treatment of the associated mental disorders including integrated treatment that considers SUD in light of patient's other medical conditions. Interventions that integrate mental health care and substance abuse programs need to be tailored for those with SCI, and be accessible. SUD has been noted as a barrier to the receipt of rehabilitation services for those with SCI, and reduces self-care. Clinicians need to be aware of this to enhance rehabilitation outcomes and community re-integration.
Across cultures, it is believed that emotional or mental health problems necessarily follow SCI.20However, our study and a few others3 point to the complex and varied nature of MI, SUD and SCI over time where such unqualified conclusions are unsupported. Although not longitudinal, our study examined the prevalence of MI and SUD over time by the duration of SCI and found that as duration of SCI increased, the likelihood of MI and/or SUD decreased. Similarly a study in the UK concluded that the relationship between post-traumatic medical improvement and psychological well-being was complex and individuals living with SCI learn to manage the consequences of their disability without significant levels of psychopathology over time.3
Our study has a number of strengths and some limitations. Strengths included our use of the SCD-R as the base and linked that registry with the VHA administrative and Medicare claims data, yielding a nation-wide overview of the prevalence of psychiatric and SUDs in those with SCI; we were able to capture detailed information on the current comorbid conditions and SCI-related information. However, the registry did not include data on the pre-morbid (MI and SUD) status of the patients, an important determinant of subsequent morbidity. Another limitation of our study is the use of ICD-9-CM codes to identify MI and SUD. However we do note that in the absence of DSM IV diagnostic criteria for MI, many studies use ICD-9-CM codes to identify MI or SUD in a variety of settings. These studies use payor claims data such as Medicare, VHA, and private insurance, collected at facilities, and national surveys. Also we did not examine concomitant SCI and traumatic brain injury (TBI), known co-occurring disorders that are frequently undiagnosed as such, TBI may have increased the prevalence of depression and PTSD.8
Despite these limitations, our study highlights the complexity of illness among veterans with SCI. The high prevalence of MI, substance abuse, and medical illness in the SCI population and their occasional mutual associations suggest not only a need for an awareness of these problems but, in the individual with coincidental complications, an investigation for causative relationship—medical or psychological.
References
Lin VW (ed) Spinal Cord Medicine: Principles and Practice. Demos; New York, 2003.
Dryden DM, Saunders LD, Rowe BH et al. Depression following traumatic spinal cord injury. Neuroepidemiology. 2005; 25: 55–61.
Pollard C, Kennedy P . A longitudinal analysis of emotional impact, coping strategies and post-traumatic psychological growth following spinal cord injury: a 10-year review. Br J Health Psychol 2007; 12: 347–362.
Craig A, Tran Y, Middleton J . Psychological morbidity and spinal cord injury: a systematic review. Spinal Cord 2009; 47: 108–114.
Stimpson NJ, Thomas HV, Weightman AL, Dunstan F, Lewis G . Psychiatric disorder in veterans of the persian gulf war of 1991.A systematic review. Br J Psychiatry 2003; 182: 391–403.
Chung MC, Preveaz E, Papandreaou K, Prevezas N . The relationship between posttraumatic stress disorder following spinal cord injury and locus of control. Affect Disord 2006; 93: 229–232.
Radnitz CL, Hsu L, Tirch DD, Willard J, Lillian LB, Walczak S et al. A comparison of posttraumatic stress disorder in veterans with and without spinal cord injury. J Abnorm Psychol. 1998; 107: 676–680.
Radnitz CL, Broderick CP, PerezStrumolo L, Tirch DD . The prevalence of psychiatric disorders in veterans with spinal cord injury: a controlled comparison. J Nerv Ment Dis 1996; 184: 431–433.
Young ME, Rintala DH, Rossi CD, Hart KA, Fuhrer MJ . Alcohol and marijuana use in a community-based sample of persons with spinal cord injury. Arch Phys Med Rehabil 1995; 76: 525–532.
Heinemann AW, Doll MD, Armstrong KJ, Schnoll S, Yarkony GM . Substance use and receipt of treatment by persons with long-term spinal cord injuries. Arch Phys Med Rehabil 1991; 72: 482–487.
Fullerton DT, Harvey RF, Klein MH, Howell T . Psychiatric disorders in patients with spinal cord injuries. Arch Gen Psychiatry 1981; 38: 1369–1371.
Imai K, Kadowaki T, Aizawa Y, Fukutomi K . Problems in the health management of persons with spinal cord injury. J Clin Epidemiol 1996; 49: 505–510.
VA.Fact Sheet: VA and Spinal Cord Injury. Available at: http://www1.va.gov/opa/fact/spinalcfs.asp; Accessed 25 November 2008.
Banerjea R, Sambamoorthi U, Smelson D, Pogach LM . Chronic illness with complexities: mental illness and substance use among veteran clinic users with diabetes. Am J Drug Alcohol Abuse 2007; 33: 807–821.
Leucht S, Burkard T, Henderson J, Maj M, Sartorius N . Physical illness and schizophrenia: a review of the literature. Acta Psychiatr Scand 2007; 116: 317–333.
Elliott TR, Frank RG . Depression following spinal cord injury. Arch Phys Med Rehabil 1996; 77: 816–823.
Samsa G, Hoenig H, Carswell J, Sloane R, Bovender CR, VanDeusenLukas C et al. Developing a national registry of veterans with spinal cord dysfunction: experiences and implications. Spinal Cord 1998; 36: 57–62.
Smith BM, Weaver FM, Ullrich PM . Prevalence of depression diagnoses and use of antidepressant medications by veterans with spinal cord injury. Am J Phys Med Rehabil 2007; 86: 662–671.
Hatzenbuehler ML, Keyes KM, Narrow WE, Grant BF, Hasin DS . Racial/ethnic disparities in service utilization for individuals with co-occurring mental health and substance use disorders in the general population: results from the national epidemiologic survey on alcohol and related conditions. J Clin Psychiatry 2008; 69: 1112–1121.
DellOrto AE, Power PW (eds) The Psychological and Social Impact of Illness and Disability. Springer Publishing Co; New York, 2007.
Acknowledgements
This research was supported by Grants from Dr Sambamoorthi (IEA-05-255) and Dr Pogach, (REA-03–021). The findings and opinions reported here are those of the authors and do not necessarily represent the views of any other individuals or organizations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Banerjea, R., Findley, P., Smith, B. et al. Co-occurring medical and mental illness and substance use disorders among veteran clinic users with spinal cord injury patients with complexities. Spinal Cord 47, 789–795 (2009). https://doi.org/10.1038/sc.2009.42
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2009.42
Keywords
This article is cited by
-
Evaluation of clinical outcomes and employment status in veterans with dual diagnosis of traumatic brain injury and spinal cord injury
Quality of Life Research (2024)
-
Increased psychological distress among individuals with spinal cord injury is associated with central neuropathic pain rather than the injury characteristics
Spinal Cord (2018)
-
Dual-energy X-ray absorptiometry and fracture prediction in patients with spinal cord injuries and disorders
Osteoporosis International (2017)