Abstract
Study design:
Cross-sectional study.
Objectives:
(1) To assess the relationship between bladder management methods and the health-related quality of life (HRQL) in patients with spinal cord injury (SCI). (2) To identify any correlation between the two questionnaires used to assess the quality of life (one validated for SCI and one validated for bladder symptoms).
Setting:
Spinal Cord Injury Centre, Royal National Orthopaedic Hospital, Middlesex, UK.
Methods:
This study is based on two questionnaires with results collected from 142 people with SCI. The two questionnaires were based on information from the Short-Form 36-Item Health Survey (SF-36) and the King's Health Questionnaire and included demographic characteristics, bladder management methods and the frequency of incontinence.
Results:
There is a moderate correlation between the results of the SF-36 and the King's Health Questionnaire. Only 21% SCI patients report normal voiding without any other form of bladder management. The type of bladder management may influence the HRQL in patients with SCI. Clean intermittent catheterization by attendant, indwelling transurethral catheterization and indwelling suprapubic catheterization are the three groups with the worst mental status. In addition, the frequency of incontinence is a strong influence on HRQL.
Conclusions:
The results of this study may provide a general baseline HRQL for patients with SCI. Our findings show the relationships between bladder management methods and quality of life in patients with SCI. In addition, the impact of incontinence on quality of life was also confirmed.
Similar content being viewed by others
Introduction
There are approximately 40 000 people with a spinal cord injury (SCI) living in the UK.1 An SCI can have a severe impact on patients and their families because of the physical and psychosocial effects of the injury. There has already been a great deal of research on neurological outcome and physical activity limitations of patients with an SCI.2, 3, 4 In addition to physical effects, an earlier study documented that the majority of the participants with an SCI suffered from various degrees of depression; indeed, 69.6% of the subjects had severe depression.5 SCI results in a significant challenge to the health-related quality of life (HRQL) of both patients and their families.
According to the results of an earlier study, HRQL is a good predictor of survival 15 years after injury,6 therefore, understanding HRQL is important in patients with an SCI. It has been reported that SCI patients with bladder problems often had a lower quality of life.7 Wyndaele et al.8 reported that conservative treatment is still the mainstay of the urological management in patients with SCI. Dahlberg et al.9 reported that patients using clean intermittent catheterization (CIC) combined with other methods (the mixed group) for bladder management had the higher frequency of urinary tract infection than other groups. Weld and Dmochowski10 reported the complication rates of each bladder management method and inferred that inappropriate selection of a bladder management method may affect patient's quality of life. However, they did not discuss thoroughly the relationship between bladder management method and quality of life. As a result, we believe that it is important to further explore the influence that different methods of bladder management have on quality of life post SCI.
An earlier study revealed that 81% of participants with an SCI suffered from various degrees of bladder dysfunction compared with 63% patients with bowel dysfunction 1 year post injury.11 Kuo12 also reported that incontinence was the most troublesome urinary problem of SCI during their study's follow-up. The severity and frequency of incontinence and its impact on quality of life has rarely been studied among patients with SCI.
The purpose of this study was to evaluate the relationships between bladder management methods and HRQL in patients with an SCI.
Materials and methods
Participants
Ethical approval was granted by the Research Ethics Committee of Royal National Orthopaedic Hospital. Each patient before participating in this study was given an information sheet explaining the procedure, the objectives and a consent form.
The principal inclusion criteria were (1) outpatients with an SCI who had returned to the Royal National Orthopaedic Hospital for a follow-up, (2) adults of both genders above the age of 16 and (3) good ability to communicate and understand the study requirements. The following reasons were considered as grounds for exclusion: (1) <1 year post injury, (2) diagnosis of cauda equina lesion, (3) presenting with other diseases involving cognitive impairment, (4) use of mechanical ventilation and (5) head injury or multiple traumas. The patients who met the criteria were invited to join the study and they were then sent one data set and two detailed questionnaires asking for their HRQL, urinary condition and demographic characteristics, such as age, gender, level of lesion, severity of cord injury, time since injury, cause of injury, marital status and educational status. The participants were invited to either answer the questionnaires by themselves or seek help if necessary (for example in the case of those participants who had a high-level cord injury).
Measures
The ‘international lower urinary tract function basic SCI data set’ was used to record the urinary information of patients with SCI.13 The data set included some questions about the urinary condition, such as the methods of bladder management and frequency of incontinence within the last 3 months.
Methods of bladder management were categorized into the following groups: normal voiding, bladder reflex voiding, bladder expression, CIC by either self-catheterization or catheterization by attendant, indwelling catheter (transurethral or suprapubic), sacral anterior root stimulation, non-continent urinary diversion/ostomy and ‘other methods’. Frequency of involuntary leakage (incontinence) was categorized into four groups: (1) no, incontinence; (2) yes, average daily; (3) yes, average weekly and (4) yes, average monthly.
This study measured participants' quality of life individually through the use of two questionnaires: the Short-Form 36-Item Health Survey (SF-36) and the King's Health Questionnaire. SF-36 is a popular generic instrument often used to assess HRQL. In addition, the King's Health Questionnaire is a condition-specific quality of life measurement, which is able to evaluate HRQL impairment because of symptoms related to the urinary tract.14 It is recommended that both generic and condition-specific instruments are used.15
The SF-36 survey is comprised of 36 questions and is organized into eight health domains: physical functioning, role physical, bodily pain, general health, vitality, social functioning, role emotional and mental health (MH). Each domain score can be transformed and ranged from 0 to 100. A higher score indicates a better health status.16 The second-order scores, the physical component score and mental component score (MCS), which are derived from the above eight scores, can provide an opportunity for more detailed interpretations. Physical functioning, physical role and bodily pain are the three health domains focusing on the physical component, whereas social functioning, emotional role and MH are the three health domains particularly related to the mental component. Furthermore, general health and vitality involve both the physical and mental components of quality of life.
The King's Health Questionnaire consists of 21 questions, which can specifically reflect the influence of urinary problem on a patient's quality of life. There are two main parts to the King's Health Questionnaire: the first part is related to general health and incontinence impact. The second part includes six health domains: role limitations, physical limitations, social limitations, personal relationships, emotions and sleep/energy.14 In addition, there are four questions related to severity of urinary problem. Each domain score is also transformed onto a scale from 0 to 100. However, unlike the SF-36, higher scores on the King's Health Questionnaire mean a worse quality of life. The SF-36 and the King's Health Questionnaire were used to evaluate the quality of life in patients with different bladder management methods and various degrees of incontinence.
Data analysis
The data was analysed using SPSS version 14.0. The data was entered twice to minimize typing errors. For descriptive purposes, the data was presented as means with standard deviations for the results of the SF-36 and the King's Health Questionnaires. The reliability of the SF-36 survey and the King's Health Questionnaire was evaluated using Cronbach's α. The results were then analysed to investigate significant interactions between the bladder management methods and the scores of the all domains of the SF-36 and the King's Health Questionnaire through analysis of variance. In addition, the interactions of frequency of incontinence with quality of life were also investigated using analysis of variance. The general linear models (GLM) were used to evaluate the significance of interactions with factors while adjusting for sex, age and severity of cord injury.17 A P-value of <0.05 was taken to indicate statistical significance, and post hoc tests were completed using Scheffe correction to control for the conduct of multiple tests. In addition, Spearman's correlation coefficients were computed to show the correlation between the King's health score and the SF-36 score in patients with SCI.
Results
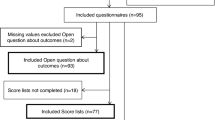
A total of 142 patients agreed to participate in this study. Ten patients refused to join because of personal reasons (participation rate was nearly 93.4%). The background characteristics of the participants are presented in Table 1.
The statistical summary for SF-36 reveals acceptable internal consistencies (Cronbach's alpha coefficient results were from 0.76 to 0.89 for all domains). The statistical summary for the King's Health Questionnaire in this study also shows good internal consistencies for the questionnaire. The results from Cronbach's alpha coefficient were from 0.77 to 0.91 for all domains.
The SF-36 scores in SCI patients using different bladder management methods are shown in Table 2. Significant differences in physical functioning, MH, physical component score and MCS can be seen. Patients who can void normally had the highest scores in the above domains. Meanwhile, there were three groups, including the CIC by attendant, indwelling transurethral catheterization and indwelling suprapubic catheterization, having the lowest scores in MH and MCS.
The scores of King's Health Questionnaire in SCI patients using different bladder management methods are shown in Table 3. Significant differences in physical limitation, personal relationship and emotions can be seen. Patients who report voiding normally had the best results (lowest scores) in all the above domains. In contrast with the group of normal voiding, those patients with indwelling catheter (suprapubic and transurethral) and those with CIC by attendant usually had the poorest condition (highest scores) in personal relationship and emotions.
Table 4 illustrates the comparisons of scores in the SF-36 for SCI patients with various degrees of incontinence. Patients without incontinence had the best scores in all domains, with significant differences in MH and MCS. The scores of the King's Health Questionnaire from SCI patients with different frequency of incontinence are shown in Table 5. Significant hierarchical differences can be seen in incontinence impact, social limitations, emotions and severity of bladder problem. Persons without incontinence also had the best results (lowest scores), in contrast to persons with daily incontinence who had the worst results (highest scores). The largest gap was found between the no incontinence and the incontinence monthly rather than between the weekly and daily subgroups in the above domains.
Spearman's correlation coefficients were used to determine the correlation between common domains of the SF-36 scales and the results from the King's Health Questionnaire. This revealed a significant correlation between the common domains and results of the two questionnaires as shown in Table 6. The correlation coefficients range from −0.52 to −0.68, indicating moderate correlations between the results of these two questionnaires.
Discussion
SCI can result in severe physical and psychosocial limitations and can affect quality of life for individuals and their families. Urological dysfunction is an important issue for patients with SCI. An earlier study recommended that choice of bladder management should include a consideration of many factors such as age, patient preference, financial concerns, functional status and patient motivation.18 As the results of this study show, quality of life should also be an important consideration.
In this study, only 21% patients with an SCI report voiding normally, 79% patients requiring specific bladder management to facilitate emptying. The results of this study indicate significant differences in the categories of physical functioning, MH, physical component score and MCS in SF-36, as well as physical limitation, personal relationship and emotions in the King's Health Questionnaire. From these results, patients who report voiding normally have the best HRQL either in physical component score or in MCS. However, those patients who need CIC by attendant or indwelling catheters (transurethral and suprapubic) report lower HRQL than patients using other methods. In addition, they also experienced some limitations in their work and activities. It is also worth noting that patients with indwelling catheters (transurethral and suprapubic) have the highest scores in their personal relationships. From the results of our research, both these indwelling catheter methods are associated with poorer reported personal interactions, possibly resulting from an obstacle to the patients' physical contact with their partners.
CIC has been shown to be the safest bladder management method for patients with an SCI in terms of urological complications.10 However, in this study, we found that patients who need CIC by attendants have the worst emotional condition. An earlier study also revealed that patients who were unable to perform catheterization independently had a 4.6-fold higher risk of depression compared with those who were able to perform self-catheterization.19
In our study, we found 56% patients had experienced incontinence in the earlier three months. From the results of SF-36, we found significant differences in MH and MCS in patients with different degrees of incontinence (Table 4). We also found some significant differences in the categories of incontinence impact, social limitations, emotions and severity of bladder problem from the results of the King's Health Questionnaire (Table 5). The frequency of incontinence is related to incontinence impact and severity of bladder problem. Incontinence also has a negative influence on patient's social function and emotion. Meanwhile, we also found that these hierarchical scores were presented in sequence and that the biggest discriminative gap was located between the no incontinence and the incontinence monthly groups (Table 5). There were only minor differences among the other groups, suggesting that the presence of incontinence would have a predictive value on social function and emotional condition.
Although the SF-36 provides a reliable assessment of quality of life, some limitations and insufficiencies of this generic instrument have been reported.20 The SF-36 still lacks a means of measuring and focusing on urinary symptoms As a result, it is necessary to combine it with the King's Health Questionnaire, a condition-specific quality of life measurement, to assess the unique impact of HRQL because of urinary problems. In this study, we found that the Spearman's correlation coefficients ranged from −0.52 to −0.68 (P-value <0.05 in all domains). This indicates that there are statistically significant moderate correlations between the scores in the SF-36 and the King's Health Questionnaires. By using these two questionnaires together, we can generate more accurate data when approaching patients with bladder problems after SCI.
There are some limitations to our study. First of all, we only collected subjects who returned to our outpatient clinic, which may not truly reflect the quality of life in SCI patients who were hospitalized as inpatients or those who do not return for follow-up appointments. Second, there were no patients using other bladder management methods (for example sacral anterior root stimulation) in this study. As a result, we cannot evaluate those SCI patients' quality of life. Third, the sample size is not large enough to purely assess the effect of bladder management on quality of life. However, the results of this study may provide a general baseline HRQL related to urinary problems in patients with an SCI. It is hoped that HRQL will become a routine part of the assessment of all patients with such a condition. In this way, we might discover other possible factors, which may increase HRQL in those with an SCI. In addition, we may do further analysis and discussion about the impact on bladder management of different factors, such as gender, level of injury and time of injury in the future.
Conclusion
There are moderate grades of correlation between the SF-36 and the King's Health Questionnaire. Only 21% of SCI patients report normal voiding, but those who are able to do so have the best quality of life in all domains. CIC by an attendant, indwelling transurethral catheters and indwelling suprapubic catheters are the three groups having the worst quality of life in their mental function. Incontinence clearly influences quality of life in patients with SCI.
References
Gall A, Turner-Stokes L . Chronic spinal cord injury: management of patients in acute hospital settings. Clin Med 2008; 8: 70–74.
Putzke JD, Richards JS, Hicken BL, DeVivo MJ . Predictors of life satisfaction: a spinal cord injury cohort study. Arch Phys Med Rehabil 2002; 83: 555–561.
Kennedy P, Rogers B . Reported quality of life of people with spinal cord injuries: a longitudinal analysis of the first 6 months post-discharge. Spinal Cord 2000; 38: 498–503.
Post MW, De Witte LP, Van Asbeck FW, Van Dijk AJ, Schrijvers AJ . Predictors of health status and life satisfaction in spinal cord injury. Arch Phys Med Rehabil 1998; 78: 395–402.
Oh SJ, Shin HI, Paik NJ, Yoo T, Ku JH . Depressive symptoms of patients using clean intermittent catheterization for neurogenic bladder secondary to spinal cord injury. Spinal Cord 2006; 44: 757–762.
Krause JS, Kjorsvig JM . Mortality after spinal cord injury: a four year prospective study. Arch Phys Med Rehabil 1992; 73: 558–563.
Westgren N, Levi R . Quality of life and traumatic spinal cord injury. Arch Phys Med Rehabil 1998; 79: 1433–1439.
Wyndaele JJ, Madersbacher H, Kovindha A . Conservative treatment of the neuropathic bladder in spinal cord injured patients. Spinal Cord 2001; 39: 294–300.
Dahlberg A, Perttila I, Wuokko E, Ala-Opas M . Bladder management in persons with spinal cord lesion. Spinal Cord 2004; 42: 694–698.
Weld KJ, Dmochowski RR . Effect of bladder management on urological complications in spinal cord injured patients. J Urol 2000; 163: 768–772.
Hicken BL, Putzke JD, Richards JS . Bladder management and quality of life after spinal cord injury. Am J Phys Med Rehabil 2001; 80: 916–922.
Kuo HC . Quality of life after active urological management of chronic spinal cord injury in eastern Taiwan. Eur Urol 1998; 34: 37–46.
Biering-Sorensen F, Craggs M, Kennelly M, Schick E, Wyndaele JJ . International lower urinary tract function basic spinal cord injury data set. Spinal Cord 2008; 46: 325–330.
Kelleher CJ, Cardozo LD, Khullar V, Salvatore S . A new questionnaire to assess the quality of life of urinary incontinent women. Br J of Obstet Gynaecol 1997; 104: 1374–1379.
Hallin P, Sullivan M, Kreuter M . Spinal cord injury and quality of life measures: a review of instrument psychometric quality. Spinal Cord 2000; 38: 509–523.
Ware JE, Sherbourne CD . The MOS 36-item short form health survey (SF-36): I. conceptual framework and item selection. Med Care 1992; 30: 473–483.
McHorney CA, Ware Jr JE, Lu JF, Sherbourne CD . The MOS 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care 1994; 32: 40–66.
Benevento BT, Sipski ML . Neurogenic bladder, neurogenic bowel, and sexual dysfunction in people with spinal cord injury. Phys Ther 2002; 82: 601–612.
Oh SJ, Ku JH, Jeon HG, Shin HI, Paik NJ, Yoo T . Health-related quality of life of patients using clean intermittent catheterization for neurogenic bladder secondary to spinal cord injury. Urology 2005; 65: 306–310.
Andresen EM, Fouts BS, Romeis JC, Brownson CA . Performance of health-related quality-of-life instruments in a spinal cord injured population. Arch Phys Med Rehabil 1999; 80: 877–884.
Acknowledgements
We thank Associate Professor Yi-Hsin Yang for her assistance with statistical analysis and Mrs Judith Grieve for her assistance with editing.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Liu, CW., Attar, K., Gall, A. et al. The relationship between bladder management and health-related quality of life in patients with spinal cord injury in the UK. Spinal Cord 48, 319–324 (2010). https://doi.org/10.1038/sc.2009.132
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2009.132
Keywords
This article is cited by
-
Experiences of people with spinal cord injuries readmitted for continence-related complications: a qualitative descriptive study
Spinal Cord (2024)
-
Validity of the Urinary Symptom Questionnaires for people with neurogenic bladder (USQNB) who void or use indwelling catheters
Spinal Cord (2021)
-
A qualitative assessment of psychosocial aspects that play a role in bladder management after spinal cord injury
Spinal Cord (2021)
-
Prevalence of urinary incontinence in women with spinal cord injury
Spinal Cord (2018)