Abstract
Real-time PCR targeting lytA (the major autolysin gene) and piaB (permease gene of the pia ABC transporter) are currently used as the gold-standard culture-independent assays for Streptococcus pneumoniae identification. We evaluated the performance of a new real-time PCR assay – targeting SP2020 (putative transcriptional regulator gene) – and compared its performance with the assays previously described. A collection of 150 pneumococci, 433 non-pneumococci and 240 polymicrobial samples (obtained from nasopharynx, oropharynx, and saliva; 80 from each site) was tested. SP2020 and lytA-CDC assays had the best performance (sensitivity of 100% for each compared to 95.3% for piaB). The specificity for lytA and piaB was 99.5% and for SP2020 was 99.8%. Misidentifications occurred for the three genes: lytA, piaB and SP2020 were found in non-pneumococcal strains; piaB was absent in some pneumococci including a serotype 6B strain. Combining lytA and SP2020 assays resulted in no misidentifications. Most polymicrobial samples (88.8%) yielded concordant results for the three molecular targets. The remaining samples seemed to contain non-typeable pneumococci (0.8%), and non-pneumococci positive for lytA (1.7%) or SP2020 (8.7%). We propose that combined detection of both lytA-CDC and SP2020 is a powerful strategy for the identification of pneumococcus either in pure cultures or in polymicrobial samples.
Similar content being viewed by others
Introduction
Identification of the human pathogen Streptococcus pneumoniae (or pneumococcus) is an important task that may pose challenges. For example, in pneumococcal carriage studies investigating vaccine impact and resistance to antibiotics, it was found that some isolates were prone to be misidentified resulting in over-estimation of rates of antimicrobial resistance1,2,3.
The WHO recommended algorithm for routine identification of pneumococcus relies on optochin susceptibility, bile solubility, and serotyping of cultured α-hemolytic colonies. Nevertheless, atypical results to these traditional phenotypic assays have been described4,5,6. Molecular assays have been used as an alternative but were found to be hampered by the frequent genetic exchange between pneumococcus and other streptococcus of the viridans group, mainly S. pseudopneumoniae and S. mitis6.
For culture-independent assays the current method of choice is a real-time PCR assay targeting the gene lytA (lytA-CDC)7,8. LytA is the major autolysin of pneumococcus and has been described as ubiquitous and specific of this species9. The performance of this real-time PCR assay was initially tested with a collection of 67S. pneumoniae and 104 non-pneumococcal isolates. The latter group included 13 viridans group streptococci not identified to the species level. This method has been extensively used by different laboratories in both disease and carriage studies10,11.
A second real-time PCR assay, targeting piaB, a permease of an ABC transporter involved in iron uptake and virulence, has also been used to increase the specificity of pneumococcal identification11,12,13. Although this system has been described as pneumococcus-specific, it is not ubiquitous, being absent from some non-encapsulated pneumococci (non-typeable, NT)14,15. Proper identification of NTs is of relevance as they are frequently multiresistant to antibiotics, preferential hubs for horizontal gene transfer and their prevalence in carriage is significant and appears to be increasing since the introduction of pneumococcal conjugate vaccines (PCVs)16,17,18,19. From a clinical perspective NT have been frequently associated with conjunctivitis outbreaks20,21,22.
Albeit there has been some evidence that homologues of lytA (and of other pneumococcal genes) can be present in closely related species of Streptococcus, until recently, this had not been sufficiently tested6,23,24: a study from Wyllie et al., published in 2017, which included hundreds of streptococcal isolates suggested that the lytA-CDC and piaB real-time PCR assays most frequently in use are 100% specific for S. pneumoniae7,11,25.
Apart from lytA and piaB, other pneumococcal genes such as the ones encoding for pneumolysin (ply) or the pneumococcal surface adhesin A (psaA) have also been tested as targets for the identification of pneumococcus. However, these were abandoned due to poorer specificity when compared to that of lytA7,25.
Other methods have also been proposed such as determination of pneumococcal-specific sequence signatures for 16S rRNA26 or S2 ribosomal protein25, and the identification of pneumococcus by MALDI-TOF27,28,29. A potential disadvantage of these methods is that they are best suited for testing pure cultures that may not always be available, for example, when pneumococcal carriage is being detected from polymicrobial samples.
One possible candidate for accurate pneumococcal identification is SP2020. SP2020 is a putative transcriptional regulator of the GntR-family and belongs to the core genome of pneumococcus30,31. Very recently, while we were in the process of publishing our study, Croxen et al. described SP2020 as a good marker to discriminate between S. pneumoniae and S. pseudopneumoniae32. The authors performed an in silico analysis based on published complete genomes which suggested that SP2020 was nearly universally present in pneumococci and absent from all non-pneumococcal streptococci. The authors also designed a real-time PCR assay targeting this marker, and tested it on a panel of 36 pneumococci and 149 non-pneumococcal streptococcal isolates32.
In this study we aimed to evaluate the performance of a new real-time PCR assay targeting SP2020 and to compare its performance with the lytA-CDC and piaB assays previously described. For that, a large collection of α-hemolytic non-pneumococcal isolates (n = 402) was tested as well as two control collections: one included 150 pneumococcal strains (of 50 serotypes and NTs); the other consisted of 31 strains of 23 non-pneumococcal Streptococcus species. Finally, the assays were tested against a collection of polymicrobial samples obtained from the nasopharynx (n = 80), oropharynx (n = 80) and saliva (n = 80).
Results and Discussion
Evaluation of lytA, piaB, and SP2020 real-time PCR assays in pure cultures of pneumococci
To evaluate the sensitivity of real-time PCR assays targeting lytA, piaB, and SP2020, 150 pneumococcal strains were used. For all pneumococcal strains, a positive real-time PCR result was obtained for lytA, and SP2020; in addition, 143 (95.3%) strains were positive for piaB (Fig. 1). Hence, by using this collection, the sensitivity of the lytA, and SP2020 assays was 100%, whereas that of piaB was 95.3% (Table 1).
CT values obtained for 150 S. pneumoniae tested by real-time PCR for the presence of lytA, piaB and SP2020. Six NT strains (blue circles) and one 6B strain (red circle) had no amplification for piaB. Three NT strains (green circles) yielded CT values for piaB far higher than those obtained for lytA and SP2020.
The seven pneumococcal strains that had a negative result for piaB were of capsular types NT (n = 6) and 6B (n = 1) (Fig. 1, Table 2).
The absence of piaB has been previously reported for NT pneumococci14,15. Among the 14 NT isolates tested only five had CT values for piaB that were concordant with those obtained for lytA and SP2020. Three other NTs yielded CT values for piaB <40 but far higher than those obtained for lytA and SP2020; six did not have any amplification for piaB in 45 cycles (Fig. 1, Table 2). All but one strain were true NTs, i.e. they were non-encapsulated belonging to cps type NCC2a or NCC2b14. The other strain was a non-encapsulated derivative of a capsulated ST156 lineage (strain PT1683)16.
We also identified a serotype 6B isolate lacking piaB. To our best knowledge, the absence of the pia locus in capsulated pneumococci has not been described before. Whole genome sequencing of this strain (strain ATCC BAA-342, the prototype of Maryland6B-17 PMEN clone)33 confirmed the presence of the 6B capsular locus, the MLST 384 profile, and the lack of piaB. Comparison with the TIGR4 genome revealed the entire piaAD locus (3.8 kb) as well as an adjacent region of 5.6 kb was absent from ATCC BAA-342 (Fig. 2a). Since serotype 6B is targeted by pneumococcal conjugate vaccines, misidentification of pneumococcus based on piaB detection could potentially affect studies aiming to evaluate vaccine efficacy.
Genomic comparison between regions of interest in TIGR4 (NCBI accession number AE 005672.3) and strains (pneumococci and non-pneumococci) with atypical results when tested for the presence of lytA, piaB, or SP2020: (a) serotype 6B pneumococcal strain (ATCC BAA-342) testing negative for piaB; (b) S. pseudopneumoniae strains Spain2270 and Spain9880 testing positive for lytA; (c) S. pseudopneumoniae strains EL2652N1 and Spain939 testing positive for piaB; (d) S. pseudopneumoniae/S. mitis strain Spain3473 testing positive for SP2020. Regions with nucleotide identity ≥93% are represented either in red (same orientation) or in blue (reverse orientation). Regions highlighted in yellow indicate the gene of interest. All comparisons were performed by Double ACT v2 and visualized using Artemis Comparison Tool (ACT) release 17.0.1.
Evaluation of lytA, piaB, and SP2020 real-time PCR assays in pure cultures of non-pneumococcal streptococci
To evaluate the specificity of the real-time PCR assays, 433 non-pneumococcal streptococcal isolates were tested. In total 98.8% of the isolates (n = 428) gave a negative result for lytA, piaB, and SP2020. Five isolates were positive for one of the assays (Table 2). Whole genome sequencing was done for these five isolates to confirm the presence of the regions of interest (containing lytA, piaB or SP2020) and for species identification based on MLST and MLSA. None of the five isolates was S. pneumoniae (Table 2, Fig. 3). Four isolates were identified as S. pseudopneumoniae: two contained lytA and two contained piaB (Fig. 2b,c). One isolate was positive for SP2020 and could not be speciated as it fell in between S. pseudopneumoniae and S. mitis (Fig. 2d).
Phylogenetic tree based on concatenated MLSA sequences of the strains analyzed in this study and S. pneumoniae, S. pseudopneumoniae, S. mitis, and S. oralis strains deposited at the eMLSA database. Five non-pneumococcal isolates giving a positive result for at least one of the real-time PCR assays were tested. Triangles indicate strains analyzed in this study: red – lytA+, blue – piaB+, green – SP2020+.
The identification of SP2020 in a non-pneumococcal strain is novel and contrasts with the study of Croxen et al., where SP2020 was universally absent from 3,405 non-pneumococcal streptococcal genomes and 46,727 non-streptococcal genomes (viral, fungal and bacterial genomes associated with sputum and nasopharyngeal samples) publicly available at the time32.
Based on these results the specificity for lytA and piaB was 99.5% and for SP2020 was 99.8% (Table 1).
Performance of lytA, piaB, and SP2020 in pure cultures
Globally, when the results obtained for pneumococci and streptococci of other species were combined, the positive predictive values (PPV) of the real-time PCR assays were 98.7% for lytA, 98.6% for piaB and 99.3% for SP2020. The negative predictive values (NPV) were 100% for lytA and SP2020, and 98.4% for piaB (Table 1).
The assays with best performance for the identification of pneumococcus in pure samples were SP2020 and lytA-CDC (Table 1, Supplementary Table 1). Of importance, combining lytA and SP2020 assays resulted in no misidentifications: all pneumococci tested contained both genes and, among the other streptococci no strain was found carrying simultaneously the two genes (Table 1).
In silico screening for lytA, piaB, and SP2020 of pneumococcal genomes
To complement our observations, we performed an in silico analyses to screen for the absence of lytA, piaB, or SP2020 in pneumococcal genomes publicly available (https://www.ncbi.nlm.nih.gov/genome/?term=streptococcus+pneumoniae). Among 8,251 pneumococcal genomes available at NCBI database (accessed July 9, 2018), lytA was absent from one genome (0.01%, serotype 3), piaB was absent from 250 genomes (3.0%, NTs and capsulated strains of 12 different serotypes), and SP2020 was absent from 23 genomes (0.28%, NTs and capsulated strains of 4 serotypes). One genome lacked both piaB and SP2020 (Supplementary Table 2). The SP2020 region targeted by the real-time PCR assay described in this study was 100% identical in 8,181 genomes and over 99% identical in 40 genomes. For the remaining six genomes this region was incomplete but 100% identical.
Evaluation of lytA, piaB, and SP2020 real-time PCR assays in polymicrobial samples
The three real-time PCR assays were tested in 240 polymicrobial samples obtained from the nasopharynx, oropharynx and saliva of adults (n = 80 for each type of sample). Most samples (88.8% of 240) yielded concordant results (either positive or negative and with comparable CT values) for the three molecular targets (Table 3, Fig. 4, Supplementary Table 3). Of notice, five samples (three from the nasopharynx and two from the oropharynx) yielded CT values for SP2020 <40 but far higher than those obtained for lytA and piaB (Fig. 4, Supplementary Table 3).
CT values obtained for 240 polymicrobial samples tested by real-time PCR for the presence of lytA, piaB and SP2020. Samples obtained from the nasopharynx, oropharynx and saliva of healthy adults (80 each) were tested. Circles indicate samples found to contain pneumococci (based on real-time PCR results for lytA, piaB, and SP2020 and real-time PCR capsular assignment). Crosses indicate samples for which no pneumococcus was detected. Additional details on these results are provided in Table 3.
As no discrepancies were observed in the efficiency of the assays when pure cultures were tested, it seems unlikely that this would have happened in these five specific samples. Whether the large difference in CT values was due to the presence of mixed strains lacking at least one of the targets remains unclear as the specific strains yielding these results were not isolated from the polymicrobial samples (see below).
The presence of pneumococci was detected in 31.2%, 22.5% and 13.8% of the nasopharyngeal, oropharyngeal and saliva samples, respectively. For all these samples a capsular type was assigned based on real-time PCR serotyping (Table 3). The presence of NT pneumococci was detected in two additional nasopharyngeal samples that were negative for piaB (Table 3, Fig. 4, Supplementary Table 3).
A total of 25 samples tested positive for only one molecular target: 4 were positive for lytA and 21 were positive for SP2020. The lytA positive samples were all obtained from the nasopharynx (4 out of 80, 5.0%), and possibly contained S. pseudopneumoniae. The SP2020 positive samples were obtained from the nasopharynx (1 out of 80, 1.3%), the oropharynx (4 out of 80, 5.0%), and saliva (16 out of 80, 20.0%) suggesting the presence of S. pseudopneumoniae/S. mitis (Table 3, Fig. 4, Supplementary Table 3).
In an attempt to isolate from polymicrobial samples pure cultures positive for SP2020 only, the saliva sample with the lowest CT (CT of 31) was serially diluted and cultured to obtain isolated colonies. Six-hundred colonies were picked and tested by real-time PCR assays for the presence of SP2020 and lytA. All 600 colonies were negative for both assays suggesting that the bacteria that contributed to positive assays were present at low density.
Taken together, the analysis of polymicrobial samples from the nasopharynx, oropharynx and saliva suggest that, as samples become increasingly complex, the chance of detecting positive signals for individual “pneumococcal markers” increases. In the polymicrobial samples we tested, this was particularly relevant when the presence of SP2020 was tested in saliva samples.
The contrast between the results obtained for SP2020 when pure cultures were analyzed (0.23% false positives, n = 1) with the results obtained in saliva samples (20% false positives) suggests that our test collection of α-hemolytic non-pneumococcal isolates was biased. This collection was obtained from nasopharyngeal and oropharyngeal samples and appears not to be representative of the plethora of non-S. pneumoniae Streptococcus spp. present in saliva. Further studies aiming to understand streptococcal diversity in the human body would be of added value to improve molecular diagnostics of S. pneumoniae.
Conclusions
The real-time PCR assay here described targeting SP2020 is useful for the correct identification of pneumococci when used in combination with lytA. Although the individual presence of these genes was detected in non-pneumococcal strains, no misidentifications occurred when both assays were combined. In particular, all NT pneumococci, which appear to be of increasing epidemiological relevance in carriage17,19, were correctly identified.
Analysis of polymicrobial samples unveiled the complexity and risks of inferring the presence of pneumococci using molecular methods only. These observations are in line with studies from Carvalho et al. and Wyllie et al. who identified homologs of pneumococcal serotype-specific gene sequences in non-pneumococcal mitis-group streptococci, confounding the detection of pneumococci in polymicrobial samples25,34. Their findings and our results, emphasize the importance of using more than one target for the identification of pneumococci.
In conclusion, combined use of real-time PCR targeting lytA and SP2020 is an improved alternative to the detection of lytA alone or in combination with piaB and is useful for detection of pneumococci in pure cultures and in polymicrobial samples.
Methods
Study collections
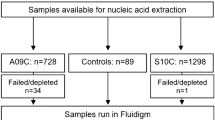
Four collections were tested: a S. pneumoniae control collection (n = 150), a non-S. pneumoniae Streptocococcus spp. control collection (n = 31), a test collection of α-hemolytic non-pneumococcal isolates (n = 402), and a test collection of polymicrobial samples collected from the nasopharynx (n = 80), oropharynx (n = 80) and saliva (n = 80).
The S. pneumoniae control collection included 150 pneumococcal strains belonging to 50 serotypes plus non-typeables (NT, n = 14). These strains were obtained from carriage studies previously described35. Strains were previously characterized based on phenotypic tests (colony morphology, optochin susceptibility and bile solubility), serotyping (PCR and/or Quellung reaction) and genotyping (PFGE and/or MLST). In addition, NT were also tested by a multiplex-PCR based strategy targeting lytA, cpsA, aliB-like ORF2, and 16SrDNA genes followed by a restriction fragment length polymorphism assay to differentiate typical from atypical lytA16,35. The represented serotypes were 1 (n = 2), 3 (n = 4), 4 (n = 2), 5 (n = 1), 6A (n = 4), 6B (n = 8), 7A (n = 1), 7F (n = 2), 8 (n = 1), 9A (n = 2), 9L (n = 2), 9N (n = 2), 9V (n = 3), 10A (n = 4), 11A (n = 4), 12A (n = 1), 12B (n = 1), 12F (n = 2), 14 (n = 8), 15A (n = 3), 15B (n = 2), 15C (n = 2), 15F (n = 2), 16F (n = 4), 17 (n = 2), 18A (n = 2), 18B (n = 2), 18C (n=2), 18F (n = 2), 19A (n = 6), 19F (n = 7), 20 (n = 1), 21 (n = 2), 22F (n = 2), 23A (n = 2), 23B (n = 2), 23F (n = 9), 24B (n = 1), 24F (n = 2), 29 (n = 2), 31 (n = 2), 33B (n = 1), 33F (n = 2), 34 (n = 2), 35B (n=1), 35F (n = 4), 37 (n = 2), 38 (n = 6), 39 (n = 1), and 42 (n = 2). This collection included the prototype strains of 27 Pneumococcal Molecular Epidemiology Network (PMEN) clones (http://www.sph.emory.edu/PMEN/index.htm): Spain23F-1, Spain6B-2, Spain9V-3, Tennessee23F-4, Spain14-5, Hungary19A-6, South Africa19A-7, South Africa6B-8, England14-9, CSR14-10, CSR19A-11, Finland6B-12, South Africa19A-13, Taiwan19F-14, Taiwan23F-15, Poland23F-16, Maryland6B-17, Tennessee14-18, Colombia5-19, Poland6B-20, Portugal19F-21, Greece6B-22, North Carolina6A-23, Utah35B-24, Sweden15A-25, Colombia23F-26, and Portugal6A-41.
The non-S. pneumoniae Streptococcus spp. control collection included 20 type strains of the following species: S. mitis (DSM-12643), S. oralis (DSM-20627), S. cristatus (DSM-8249), S. gordonii (DSM-6777), S. infantis (DSM-12492), S. parasanguinis (DSM-6778), S. peroris (DSM-12493), S. sanguinis (DSM-20567), S. sinensis (DSM-14990), S. anginosus subsp. anginosus (DSM-20563), S. constellatus subsp. constellatus (NCTC11325), S. intermedius (NCTC11324), S. salivarius subsp. salivarius (DSM-20560), S. vestibularis (DSM-5636), S. agalactiae (DSM-6784), S. canis (DSM-20715), S. dysgalactiae sub. dysgalactiae (DSM-20662), S. equi sub. zooepidemicus (DSM-20727), S. mutans (DSM-20523) and S. pyogenes (DSM-20565). In addition, it also included 11 strains of the following species: S. pseudopneumoniae (PT5479 and IS7943)2,24, S. oralis (DSM-20066 and DSM-20395), S. gordoni (DSM-20568), S. dysgalactiae sub. equisimilis (DSM-6176), S. equinus (NCTC10389 and DSM-20480) and Streptococcus spp. (DSM20377, DSM20379 and DSM20392). DSM strains were obtained from the Leibniz Institute DSMZ-German Collection of Microorganisms and Cell Cultures (www.dsmz.de) and NCTC strains were obtained from the National Collection of Type Cultures of Public Health England (www.phe-culturecollections.org.uk).
The test collection of α-hemolytic non-pneumococcal isolates included 402 isolates, recovered from humans between 1991 and 2012 from different carriage and disease studies and all belong to our collection2,36,37. Isolates were initially isolated based on the observation of α-hemolysis and colony morphology suggestive of pneumococcus, but were found to be of other streptococcal species when a combination of methods was applied (optochin susceptibility, bile solubility, serotyping, and lytA-BsaI-RFLP)2,38. Of the 402 α-hemolytic non-pneumococcal isolates tested, 346 were resistant to optochin, 25 were susceptible to optochin but bile insoluble, and 31 were susceptible to optochin and bile soluble but could not be assigned to a serotype. These latter 31 isolates were confirmed not to be pneumococcus by a multiplex PCR scheme previously described and the identification of characteristic non-pneumococcal lytA-BsaAI-RFLP signatures35,38.
The test collection of polymicrobial samples (from the nasopharynx, oropharynx and saliva, 80 each) was obtained between 2015 and 2016 from healthy adults aged 25 to 50 years old. Nasopharyngeal and oropharyngeal swabs were placed in STGG; saliva was collected by spitting into a tube and 1 ml was transferred to a tube containing 500 μl of sterile 50% glycerol. Samples were kept on wet ice and transported to the laboratory. Upon arrival samples were thoroughly vortexed and plated (100 μl for the nasopharyngeal sample and 50 μl for the oropharyngeal and saliva samples) onto blood agar plates supplemented with 5 µg/mL gentamicin, and grown overnight in anaerobic jars at 37 °C. The total bacterial growth was collected and frozen at −80 °C in STGG medium. From these tubes DNA was extracted and tested as described below.
Isolation of single colonies from polymicrobial sample
Serial dilutions up to 10−8 were performed for one polymicrobial sample from saliva. Fifty microliters of each dilution were inoculated onto blood agar plates supplemented with 5 µg/mL gentamicin, and incubated overnight at 37 °C in 5% CO2. On the following day plates were inspected for the presence of single colonies and a total of 600 colonies were picked randomly. Each colony was streaked in a 1/10 slice of a novel blood agar plate. The plates obtained (n = 60) were incubated as above. On the following day, the 10 cultures in each plate were collected from a pre-defined circle area in the center of the plate. This ensured that similar amounts of each culture were collected. Pools of 10 cultures were resuspended in PBS. These pools were used for DNA extraction.
Genomic DNA extraction
DNA was extracted from pure cultures using the MagNa Pure Compact Nucleic Acid Isolation kit (Roche Diagnostics GmbH) or the DNeasy Blood & Tissue kit (Qiagen) as recommended by the manufacturers. DNA from polymicrobial samples was extracted using the MagNa Pure Compact Nucleic Acid Isolation kit. To control for DNA contamination, during DNA extraction, for each batch of seven samples being processed, one additional sample containing only ultrapure water was processed in parallel. DNA quantification and purity were evaluated with NanoDrop (Thermo Fisher). DNA for whole genome sequencing was treated with RNase and analyzed with NanoDrop and Qubit (Thermo Fisher).
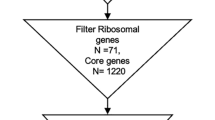
Design of real-time PCR assay targeting SP2020
SP2020 (encoding for a putative transcriptional regulator) was initially selected by in silico screening of 27 genomes of S. pneumoniae for genes that are highly conserved, universally present and specific to the species. Upon identification of SP2020 as a potential candidate, BLAST analysis was conducted against the NCBI database using the same criteria. In addition, SP2020 has been evaluated with ~15,000 samples as one of the control genes for pneumococcus in the BμG@S SP-CPS microarray (J. Hinds, personal communication).
To design the real-time PCR assay targeting SP2020, the nucleotide sequence of the TIGR4 SP2020 gene (NCBI accession number AE 005672.3, nt 1925563 to 1926291) was blasted against the NCBI database (as of November 2015). Homology was found only to pneumococcal nucleotide sequences (29 sequences, 99–100% nucleotide similarity) and not to any other Streptococcus species. One set of primers and a FAM-labeled probe were custom-designed (Metabion International AG):
SP_2020_F (5′-TAAACAGTTTGCCTGTAGTCG-3′),
SP_2020_R (5′-CCCGGATATCTCTTTCTGGA-3′), and
SP_2020_P (5′-Fam-AACCTTTGTTCTCTCTCGTGGCAGCTCAA-BHQ-3′). This combination of primers resulted in an amplicon length of 155 bp (nt 1926036 to 1926190 of TIGR4). The real-time PCR assay was tested and optimized for S. pneumoniae TIGR4 and S. pseudopneumoniae ATCC BAA-960 (NCBI accession number AM113495.1).
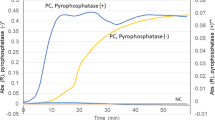
Real-time PCR targeting lytA, piaB, and SP2020
Assays were performed according to the MIQE guidelines39. The presence of the genes lytA and piaB was tested by using primers and probes previously described7,11. The presence of SP2020 was tested by using primers and probes described above. For DNA obtained from pure cultures 2.5 μL of DNA at 0.2 ng/μL were used in each reaction. For polymicrobial samples 2.5 μL of DNA were used regardless of their concentration. All reactions were performed in a final volume of 25 μL containing 1x FastStart TaqMan Probe Master (Roche), 0.15 mM each primer, 0.075 mM probe. DNA was amplified with the CFX96 Real-Time System Amplification (Bio-Rad) by using the following cycling conditions: 95 °C for 10 min followed by 45 cycles of 95 °C for 15 sec, 60 °C (for lytA-CDC and piaB) or 55 °C (for SP2020) for 1 min. Fluorescence was read after each of the 45 cycles.
All strains from S. pneumoniae control collection and non-S. pneumoniae Streptococcus spp. control collection were tested twice on different days. All strains from the α-hemolytic non-pneumococcal streptococcal collection were tested once, except when amplification occurred. In such cases, isolates were re-tested on a different day for confirmation. In addition, for each assay, a random selection of 10% of the strains from the test collection was also independently selected for re-testing. DNA from S. pneumoniae TIGR4 (positive control) and S. pseudopneumoniae ATCC BAA-960 (negative control) were used in every run. Samples were considered positive when the cycle threshold (CT) value was equal or below 40.
Similarly, polymicrobial samples were tested once, except when amplification occurred. In such cases, isolates were re-tested on a different day for confirmation.
Contamination assessment during real-time PCR assays was evaluated systematically in all runs by testing extracted ultrapure water (described above), water used in DNA dilutions, and water used in the real-time PCR reactions.
In addition, all non-pneumoccoccal streptococcal isolates giving positive results for the real-time PCR assays were further evaluated: single colonies were picked from each culture and streaked for five consecutive days to confirm sample purity. On the fifth day, a new culture stock was done, DNA was extracted, real-time PCR assays were repeated and the results were confirmed. Whole genome sequencing analysis was performed as described below.
Performance of real-time PCR assays for the identification of pneumococcus
To evaluate the performance of the real-time PCR assays for the identification of pneumococcus, four parameters were estimated: sensitivity (to estimate the percentage of pneumococci correctly identified among all pneumococci tested), specificity (to estimate the percentage of non-pneumococci correctly identified among all non-pneumococci tested), positive predictive value (PPV, to estimate the percentage of pneumococci among all isolates giving a positive result for a given assay), and negative predictive value (NPV, to estimate the percentage of non-pneumococci among all isolates giving a negative result for a given assay). Sensitivities and specificities of real-time PCR assays were compared using the McNemar test40. PPVs and NPVs of real-time PCR assays were compared using the generalized score statistic proposed by Leisenring et al.41. Both statistics were calculated using the R package DTComPair42.
Real-time PCR serotyping
All polymicrobial samples giving results suggesting the presence of pneumococci were further tested using a panel of primers and probes for serotype assignment (1, 2, 3, 4, 5, 6A/B/C/D, 7A/F, 9A/V, 11A/D, 12A/B/F/44/46, 14, 15A/F, 16F, 18A/B/C/F, 19A, 19F, 22A/F, 23A, 23F, 33A/F/3743, 8, 10A/B and 38)44 as previously described45.
Whole genome sequencing and genomic comparison with TIGR4
Genomes of five non-pneumococcal isolates testing positive for at least one of the real-time PCR assays and of one capsulated pneumococcal isolate giving a negative result for piaB were sequenced by the Illumina MiSeq platform, with a minimum coverage of 100x. Library preparation and sequencing were done at the Genomics Unit of Instituto Gulbenkian de Ciência (Oeiras, Portugal). Paired-end reads were checked for quality, trimmed, and de novo assembled using the Qiagen CLC Genomics Workbench version 9.0.1 software (Qiagen, Venlo, The Netherlands). Bubble size, word size and paired distances were automatically calculated by the software. The consensus sequences were extracted and the contigs were deposited in NCBI database and annotated with the Prokaryotic Genomic Annotation Pipeline. Read data, assembled and annotated contigs of the six sequenced isolates were deposited in the NCBI database: BioProject accession number PRJNA434586.
For the pneumococcal isolate, the assembled contigs were ordered against TIGR4 complete genome using Mauve version 2.3.146 and concatenated using Artemis release 17.0.147. Genomic comparison between TIGR4 and the pneumococcal isolate was performed using Double ACT v2 and visualized using Artemis Comparison Tool (ACT)48. For the non-pneumococcal isolates, assembled contigs were blasted against the nucleotide sequences of TIGR4 lytA (SP_1937, nt 1840405 to 1841361), TIGR4 piaB (SP_1033, nt 974409 to 975428) or TIGR4 SP2020 (SP_2020, nt 1925563 to 1926291). Comparisons between TIGR4 complete genome and the hit contigs were performed by Double ACT v2 and visualized using Artemis Comparison Tool (ACT).
Multilocus sequence analysis (MLSA) for viridans group streptococci (viridans MLSA)
DNA sequences of the seven housekeeping genes map, pfl, ppaC, pyk, rpoB, sodA, and tuf were extracted from whole genome sequencing data. Phylogenetic analysis of the concatenated sequences in comparison with the eMLSA database (http://www.emlsa.net/) was performed using MEGA6.06 (http://www.megasoftware.net) as described: alignment of sequences by ClustalW and construction of a minimum-evolution phylogenetic tree using default parameters49,50.
Multilocus sequence typing (MLST) using the S. pneumoniae MLST database
Allele assignment for the seven housekeeping genes aroE, ddl, gdh, gki, recP, spi, and xpt was inferred from whole genome sequencing data using the tool MLST 1.8 provided by the Center for Genomic Epidemiology51.
In silico screening for lytA, piaB, and SP2020 of pneumococcal genomes
An in silico analyses to screen for the absence of lytA, piaB, or SP2020 was performed for 8251 pneumococcal genomes available at NCBI database (https://www.ncbi.nlm.nih.gov/genome/?term=streptococcus+pneumoniae, accessed on July 9, 2018). Sequences were extracted as fasta files and imported into Qiagen CLC Genomics Workbench version 9.0.1 software. Blasts were performed against the nucleotide sequences of TIGR4 lytA (SP_1937, nt 1840405 to 1841361), TIGR4 piaB (SP_1033, nt 974409 to 975428) and TIGR4 SP2020 (SP_2020, nt 1925563 to 1926291).
Ethics statement
The study was conducted in accordance with the European Statements for Good Clinical Practice and the declaration of Helsinki of the World Health Medical Association and is integrated in a project approved by “Conselho de Ética para a Saúde do Instituto de Higiene e Medicina Tropical da Universidade Nova de Lisboa” (Process No. 04-2014-PN). Written, informed consent was obtained from all participants providing biological samples.
References
Richter, S. S. et al. Accuracy of phenotypic methods for identification of Streptococcus pneumoniae isolates included in surveillance programs. J Clin Microbiol 46, 2184–8 (2008).
Simões, A. S. et al. Highly penicillin-resistant multidrug-resistant pneumococcus-like strains colonizing children in Oeiras, Portugal: genomic characteristics and implications for surveillance. J Clin Microbiol 48, 238–46 (2010).
Wester, C. W. et al. Possible overestimation of penicillin resistant Streptococcus pneumoniae colonization rates due to misidentification of oropharyngeal streptococci. Diagn Microbiol Infect Dis 42, 263–8 (2002).
Arbique, J. C. et al. Accuracy of phenotypic and genotypic testing for identification of Streptococcus pneumoniae and description of Streptococcus pseudopneumoniae sp. nov. J Clin Microbiol 42, 4686–96 (2004).
Mundy, L. S., Janoff, E. N., Schwebke, K. E., Shanholtzer, C. J. & Willard, K. E. Ambiguity in the identification of Streptococcus pneumoniae. Optochin, bile solubility, quellung, and the AccuProbe DNA probe tests. Am J Clin Pathol 109, 55–61 (1998).
Whatmore, A. M. et al. Genetic relationships between clinical isolates of Streptococcus pneumoniae, Streptococcus oralis, and Streptococcus mitis: characterization of “atypical” pneumococci and organisms allied to S. mitis harboring S. pneumoniae virulence factor-encoding genes. Infect Immun 68, 1374–82 (2000).
Carvalho Mda, G. et al. Evaluation and improvement of real-time PCR assays targeting lytA, ply, and psaA genes for detection of pneumococcal DNA. J Clin Microbiol 45, 2460–6 (2007).
Satzke, C. et al. Standard method for detecting upper respiratory carriage of Streptococcus pneumoniae: updated recommendations from the World Health Organization Pneumococcal Carriage Working Group. Vaccine 32, 165–79 (2013).
Pozzi, G., Oggioni, M. R. & Tomasz, A. DNA probe for identification of Streptococcus pneumoniae. J Clin Microbiol 27, 370–2 (1989).
del Amo, E. et al. Estimation of the invasive disease potential of Streptococcus pneumoniae in children by the use of direct capsular typing in clinical specimens. Eur J Clin Microbiol Infect Dis 34, 705–11 (2015).
Trzcinski, K. et al. Superiority of trans-oral over trans-nasal sampling in detecting Streptococcus pneumoniae colonization in adults. PLOS ONE 8, e60520 (2013).
Brown, J. S., Gilliland, S. M. & Holden, D. W. A Streptococcus pneumoniae pathogenicity island encoding an ABC transporter involved in iron uptake and virulence. Mol Microbiol 40, 572–85 (2001).
Wyllie, A. L. et al. Streptococcus pneumoniae in saliva of Dutch primary school children. PLOS One 9, e102045 (2014).
Tavares, D. A. et al. Non-typeable pneumococci circulating in Portugal are of cps type NCC2 and have genomic features typical of encapsulated isolates. BMC Genomics 15, 863 (2014).
Whalan, R. H. et al. Distribution and genetic diversity of the ABC transporter lipoproteins PiuA and PiaA within Streptococcus pneumoniae and related streptococci. J Bacteriol 188, 1031–8 (2006).
Sá-Leão, R. et al. Identification, prevalence and population structure of non-typable Streptococcus pneumoniae in carriage samples isolated from preschoolers attending day-care centres. Microbiology 152, 367–76 (2006).
Nunes, S. et al. The impact of private use of PCV7 in 2009 and 2010 on serotypes and antimicrobial resistance of Streptococcus pneumoniae carried by young children in Portugal: Comparison with data obtained since 1996 generating a 15-year study prior to PCV13 introduction. Vaccine 34, 1648–56 (2016).
Chewapreecha, C. et al. Dense genomic sampling identifies highways of pneumococcal recombination. Nat Genet 46, 305–309 (2014).
Valente, C. et al. Impact of the 13-valent pneumococcal conjugate vaccine on Streptococcus pneumoniae multiple serotype carriage. Vaccine 34, 4072–8 (2016).
Shayegani, M., Parsons, L. M., Gibbons, W. E. Jr. & Campbell, D. Characterization of nontypable Streptococcus pneumoniae-like organisms isolated from outbreaks of conjunctivitis. J Clin Microbiol 16, 8–14 (1982).
Carvalho, M. G., Steigerwalt, A. G., Thompson, T., Jackson, D. & Facklam, R. R. Confirmation of nontypeable Streptococcus pneumoniae-like organisms isolated from outbreaks of epidemic conjunctivitis as Streptococcus pneumoniae. J Clin Microbiol 41, 4415–7 (2003).
CDC. Pneumococcal conjunctivitis at an elementary school—Maine, September 20-December 6, 2002. MMWR Morb Mortal Wkly Rep 52, 64–6 (2003).
Romero, P., Lopez, R. & Garcia, E. Characterization of LytA-like N-acetylmuramoyl-L-alanine amidases from two new Streptococcus mitis bacteriophages provides insights into the properties of the major pneumococcal autolysin. J Bacteriol 186, 8229–39 (2004).
Shahinas, D. et al. Whole-genome sequence of Streptococcus pseudopneumoniae isolate IS7493. J Bacteriol 193, 6102–3 (2011).
Wyllie, A. L. et al. Sequencing of the variable region of rpsB to discriminate between Streptococcus pneumoniae and other streptococcal species. Open Biol 7 (2017).
Scholz, C. F., Poulsen, K. & Kilian, M. A novel molecular identification method for Streptococcus pneumoniae applicable to clinical microbiology and 16S rRNA-sequence based microbiome studies. J Clin Microbiol (2012).
Chen, J. H. et al. Use of MALDI Biotyper plus ClinProTools mass spectra analysis for correct identification of Streptococcus pneumoniae and Streptococcus mitis/oralis. J Clin Pathol 68, 652–6 (2015).
Ikryannikova, L. N. et al. Discrimination between Streptococcus pneumoniae and Streptococcus mitis based on sorting of their MALDI mass spectra. Clin Microbiol Infect 19, 1066–71 (2013).
Werno, A. M., Anderson, T. P. & Murdoch, D. R. Association between pneumococcal load and disease severity in adults with pneumonia. J Med Microbiol 61, 1129–1135 (2012).
Obert, C. et al. Identification of a candidate Streptococcus pneumoniae core genome and regions of diversity correlated with invasive pneumococcal disease. Infect Immun 74, 4766–77 (2006).
van Tonder, A. J. et al. Defining the estimated core genome of bacterial populations using a Bayesian decision model. PLOS Comput Biol 10, e1003788 (2014).
Croxen, M. A., Lee, T. D., Azana, R. & Hoang, L. M. Use of genomics to design a diagnostic assay to discriminate between Streptococcus pneumoniae and Streptococcus pseudopneumoniae. Microb Genom 4 (2018).
Gherardi, G., Whitney, C. G., Facklam, R. R. & Beall, B. Major related sets of antibiotic-resistant pneumococci in the United States as determined by pulsed-field gel electrophoresis and pbp1a-pbp2b-pbp2x-dhf restriction profiles. J Infect Dis 181, 216–29 (2000).
Carvalho Mda, G. et al. Non-pneumococcal mitis-group streptococci confound detection of pneumococcal capsular serotype-specific loci in upper respiratory tract. PeerJ 1, e97 (2013).
Simões, A. S., Valente, C., de Lencastre, H. & Sá-Leão, R. Rapid identification of noncapsulated Streptococcus pneumoniae in nasopharyngeal samples allowing detection of co-colonization and reevaluation of prevalence. Diagn Microbiol Infect Dis 71, 208–16 (2011).
Almeida, S. T. et al. Low prevalence of pneumococcal carriage and high serotype and genotype diversity among adults over 60 years of age living in Portugal. PLOS One 9, e90974 (2014).
Rolo, D. et al. Disease isolates of Streptococcus pseudopneumoniae and non-typeable S. pneumoniae presumptively identified as atypical S. pneumoniae in Spain. PLOS ONE 8, e57047 (2013).
Llull, D., Lopez, R. & Garcia, E. Characteristic signatures of the lytA gene provide a basis for rapid and reliable diagnosis of Streptococcus pneumoniae infections. J Clin Microbiol 44, 1250–6 (2006).
Bustin, S. A. et al. The MIQE guidelines: minimum information for publication of quantitative real-time PCR experiments. Clin Chem 55, 611–22 (2009).
McNemar, N. Q. Note on the sampling error of the difference between correlated proportions or percentages. Psychometrika 12, 153–7 (1947).
Leisenring, W., Alonzo, T. & Pepe, M. S. Comparisons of predictive values of binary medical diagnostic tests for paired designs. Biometrics 56, 345–51 (2000).
R Core Team R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria, www.R-project.org/ (2013).
Pimenta, F. C. et al. Sequential triplex real-time PCR assay for detecting 21 pneumococcal capsular serotypes that account for a high global disease burden. J Clin Microbiol 51, 647–52 (2013).
Azzari, C. et al. Realtime PCR is more sensitive than multiplex PCR for diagnosis and serotyping in children with culture negative pneumococcal invasive disease. PLOS One 5, e9282 (2010).
Wyllie, A. L. et al. Molecular surveillance of nasopharyngeal carriage of Streptococcus pneumoniae in children vaccinated with conjugated polysaccharide pneumococcal vaccines. Sci Rep 6, 23809 (2016).
Darling, A. C., Mau, B., Blattner, F. R. & Perna, N. T. Mauve: multiple alignment of conserved genomic sequence with rearrangements. Genome Res 14, 1394–403 (2004).
Rutherford, K. et al. Artemis: sequence visualization and annotation. Bioinformatics 16, 944–5 (2000).
Carver, T. J. et al. ACT: the Artemis Comparison Tool. Bioinformatics 21, 3422–3 (2005).
Simões, A. S. et al. lytA-based identification methods can misidentify Streptococcus pneumoniae. Diagn Microbiol Infect Dis 85, 141–8 (2016).
Bishop, C. J. et al. Assigning strains to bacterial species via the internet. BMC Biol 7, 3 (2009).
Larsen, M. V. et al. Multilocus sequence typing of total-genome-sequenced bacteria. J Clin Microbiol 50, 1355–61 (2012).
Acknowledgements
This work was financially supported by projects LISBOA-01-0145-FEDER (Microbiologia Molecular, Estrutural e Celular, funded by FEDER through COMPETE2020 – Programa Operacional Competitividade e Internacionalização) and LISBOA-01-0145-FEDER-016417 (ONEIDA co-funded by Fundos Europeus Estruturais e de Investimento, Programa Operacional Regional Lisboa 2020 and Fundação para a Ciência e a Tecnologia (FCT)). DAT, SH and ACP were funded by fellowships SFRH/BD/70147/2010, PD/BD/128365/2017 and SFRH/BPD/99638/2014, respectively, from FCT. The authors thank Dea Shahinas for providing S. pseudopneumoniae strain IS7943 and Tiago Touret for extracting and preliminary blast analysis of pneumococcal genomes used in the in silico analysis. We thank three anonymous reviewers for their comments and suggestions that contributed to improve this manuscript.
Author information
Authors and Affiliations
Contributions
R.S.L., J.H., D.A.T. and S.H. conceived and designed the experiments; D.A.T., S.H. and R.J.C. performed the experiments; D.A.T., S.H., R.J.C. and R.S.L. analyzed the data; A.C.P. performed statistical analyses; H.L. and R.S.L. contributed reagents, materials and analysis tools; D.A.T., S.H. and R.S.L. wrote the manuscript; all authors critically revised the manuscript and approved its final version.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tavares, D.A., Handem, S., Carvalho, R.J. et al. Identification of Streptococcus pneumoniae by a real-time PCR assay targeting SP2020. Sci Rep 9, 3285 (2019). https://doi.org/10.1038/s41598-019-39791-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-39791-1
This article is cited by
-
Optimization of a high-throughput nanofluidic real-time PCR to detect and quantify of 15 bacterial species and 92 Streptococcus pneumoniae serotypes
Scientific Reports (2023)
-
Development of diagnostic tests for pathogen identification and detection of antimicrobial resistance on WHO global priority pathogens using modular real-time nucleic acid amplification test
International Microbiology (2023)
-
Strain-level resolution and pneumococcal carriage dynamics by single-molecule real-time (SMRT) sequencing of the plyNCR marker: a longitudinal study in Swiss infants
Microbiome (2022)
-
Molecular characterization and epidemiology of Streptococcus pneumoniae serotype 8 in Denmark
BMC Infectious Diseases (2021)
-
Molecular surveillance of pneumococcal carriage following completion of immunization with the 13-valent pneumococcal conjugate vaccine administered in a 3 + 1 schedule
Scientific Reports (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.