Abstract
Low ADAMTS13 activity is associated with an increased risk of cardiovascular disease, which is generally attributed to its proteolytic effects on Von Willebrand factor (VWF). Cardiovascular health is an important determinant of cognitive decline, but the association of either VWF or ADAMTS13 with risk of dementia is unknown. Between 1997–2002, we measured VWF antigen and ADAMTS13 activity in 6055 participants of the population-based Rotterdam Study (mean age 69.3 years, 57.2% women). At baseline, 85 participants had dementia, and during 15 years of follow-up 821 developed dementia. Higher VWF was associated with prevalence and risk of dementia, unaffected by concurrent ADAMTS13 activity, but estimates strongly attenuated over time and were no longer statistically significant at 4 years of follow-up (relative risks [95% CI] per standard deviation increase– cross-sectional: 1.37 [1.06–1.77], and longitudinal: 1.05 [0.97–1.14]). In contrast, low ADAMTS13 was associated with increased risk of dementia throughout follow-up (hazard ratio per SD decrease– 1.16 [1.06–1.28]), which alike for ischaemic stroke, was modified by the presence of diabetes (P-interaction = 0.003). In conclusion, higher VWF and low ADAMTS13 activity are associated with increased risk of dementia, but differences in time-course and lack of synergistic effects may indicate in part independent underlying mechanisms.
Similar content being viewed by others
Introduction
Von Willebrand factor (VWF) is a large multimeric glycoprotein with critical functions in haemostasis. Deficiency or dysfunction of VWF, known as Von Willebrand disease, can cause prolonged or excessive bleeding1, whereas high levels of VWF antigen have been associated with increased risk of cardiovascular disease2. In vivo effects of VWF largely depend on the proteolytic activity of ADAMTS13 (A Disintegrin And Metalloproteinase with a ThromboSpondin type 1 motif, member 13). ADAMTS13 cleaves large, haemostatically highly reactive VWF multimers into smaller, less active multimers. Consequently, high VWF may lead to a hypercoagulable state in particular when ADAMTS13 activity is low, and a combined measure of VWF and ADAMTS13 could thus more accurately capture the biological activity of VWF3. We have previously shown that low activity of ADAMTS13 itself is associated with increased risk of cardiovascular disease4,5,6,7,8, while the combination of VWF and ADAMTS13 appears indeed more strongly associated with stroke risk than what would be expected on the basis of the individual measurements5.
Vascular disease and thrombosis play an important role in the aetiology of dementia, including Alzheimer’s disease9. Accordingly, a recent meta-analysis of cross-sectional studies concluded that VWF antigen levels are higher in patients with dementia than in controls10. However, of two studies that assessed the risk of dementia by VWF11,12, neither found baseline VWF antigen levels associated with dementia risk after 4 and 17 years of follow-up, respectively, albeit the latter was hampered by substantial attrition (50%) and lack of cognitive screening at baseline. Apart from methodological considerations, release of VWF from damaged endothelial cells in later stages of cognitive impairment may explain why profound cross-sectional associations do not extend to longer term follow-up. However, the time-course of the association between VWF and dementia remains unknown, and although ADAMTS13 could aid in disentangling haemostatic effects from associations marking endothelial damage, no published studies about VWF and dementia took into account concurrent ADAMTS13 activity.
While VWF is the only known substrate for ADAMTS13, several studies suggest that ADAMTS13 might have functions beyond VWF cleavage. Suggested roles include inflammation, angiogenesis, and extracellular matrix integrity13, each of which have been implicated also in the aetiology of dementia14,15,16. A versatile role of ADAMTS13 was further suggested, when we recently showed that high activity of ADAMTS13 relates to a higher risk of diabetes in the general population17. The underlying mechanisms remain elusive, but these studies jointly highlight the need for investigation of ADAMTS13 in the context of, as well as beyond its proteolytic activity of VWF.
We aimed to determine the cross-sectional and long-term associations of VWF and ADAMTS13 with cognitive decline and dementia risk in a population-based study. We investigated independent and synergistic effects of VWF and ADAMTS13, and explored these associations in the context of prior studies linking ADAMTS13 to diabetes, angiogenesis, and extracellular matrix integrity.
Methods
This study is part of the Rotterdam Study, a large ongoing population-based cohort study in the Netherlands, with an initial study population of 7,983 participants aged ≥ 55 years from the Ommoord area, a suburb of Rotterdam. In 2000, the cohort was expanded with an additional 3011 participants who moved into the study area or reached age 55. The Rotterdam Study methods have been described previously18. Briefly, participants were interviewed at home and subsequently examined at the research centre for baseline assessment from 1990 to 1993 (baseline cohort) and 2000 to 2002 (expansion cohort), with follow-up examinations every 4 years. Citrated plasma samples were collected at the third visit of the original cohort (1997–1999), and the first visit of the expansion cohort (2000–2002), which are the baseline of the current study. Of 9,030 surviving participants at the time, 7,510 participated in this examination cycle, of whom 6,735 visited the study centre. Of these, 43 had insufficient cognitive screening to determine dementia status.
Ethical approval and data availability
The Rotterdam Study has been approved by the medical ethics committee according to the Population Study Act Rotterdam Study, executed by the Ministry of Health, Welfare and Sports of the Netherlands. Written informed consent was obtained from all participants. Rotterdam Study data can be made available to interested researchers upon request. Requests can be directed to data manager Frank J.A. van Rooij (f.vanrooij@erasmusmc.nl). We are unable to place data in a public repository due to legal and ethical restraints. Sharing of individual participant data was not included in the informed consent of the study, and there is potential risk of revealing participants’ identities as it is not possible to completely anonymize the data. This is of particular concern given the sensitive personal nature of much of the data collected as part of the Rotterdam Study.
Measurement of Von Willebrand factor antigen and ADAMTS13 activity
Fasting venous blood samples were taken at the research centre, and citrated plasma was stored at –80 °C. We determined VWF antigen with an in-house enzyme-linked immunosorbent assay using polyclonal rabbit antihuman VWF antibodies (DakoCytomation, Glostrop, Denmark) for catching and tagging. The intra-assay coefficient of variation was 5.8% and the inter-assay coefficient of variation was 7.8%. We measured ADAMTS13 activity using a kinetic assay based on the fluorescence resonance energy transfer substrate VWF73 (FRETSVWF73) assay19. This assay uses a peptide containing the ADAMTS13 cleavage site of VWF, and thus captures variation in the VWF cleavage rate determined by ADAMTS13 levels and structure. Plasma samples were measured against a reference curve of serial dilutions of normal human plasma defined to have an ADAMTS13 activity of 1 IU/mL, and we expressed ADAMTS13 activity as a percentage of this. Ten percent of the samples were retested and all were within 25% variation. From these measurements, we also calculated the ratio between ADAMTS13 activity and VWF antigen levels.
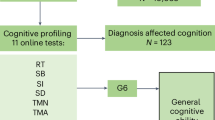
Cognitive function assessment and dementia screening
Participants underwent detailed tests to determine cognitive function, comprising the Stroop test (error adjusted time in seconds taken for completing a reading/colour naming interference task), the letter-digit substitution task (number of correct digits in 1 minute), and the verbal fluency test (number of animal species within 1 minute)20. Cognitive function was assessed at baseline (i.e. time of blood sampling) and at three subsequent follow-up examinations (after a mean follow-up of 4.4 (SD 0.6), 10.8 (SD 0.6), and 15.4 (SD 0.7) years, respectively). To obtain a composite measure of test performance, we calculated the G-factor, which explained approximately 61% of variance in cognitive test scores at each examination round in our population. For each participant, Z-scores were calculated for each test separately, by dividing the difference between individual test score and population mean by the population standard deviation.
Participants were screened for dementia at baseline and subsequent centre visits21. Those with a Mini-Mental State Examination score < 26 or Geriatric Mental Schedule score > 0 underwent further investigation and informant interview, including the Cambridge Examination for Mental Disorders of the Elderly. In addition, the entire cohort was under continuous surveillance for dementia through electronic linkage of the study database with medical records from general practitioners and the regional institute for outpatient mental health care. A consensus panel led by a consultant neurologist established the final diagnosis according to standard criteria for dementia (DSM-III-R) and Alzheimer’s disease (NINCDS–ADRDA). Within this period, participants were censored at date of dementia diagnosis, death, loss to follow-up, or 1st January 2015, whichever came first.
Other measurements
We assessed smoking status (i.e. current, former, never) and use of antihypertensive, lipid-lowering, glucose lowering, and antithrombotic (i.e. coumarine derivatives or platelet inhibitors) medication at baseline by interview. Systolic and diastolic blood pressures were measured with a random-zero sphygmomanometer. Fasting serum lipid levels, C-reactive protein (CRP) and fibrinogen were measured at baseline. Diabetes, prediabetes and normoglycaemia were defined according to WHO guidelines22. APOE genotype was determined using polymerase chain reaction on coded DNA samples (baseline cohort), and using a bi-allelic TaqMan assay (rs7412 and rs429358; expansion cohort). ABO blood group antigen phenotypes were reconstructed by haplotype analysis of 3 single nucleotide polymorphisms (rs8176749, rs8176704, and rs505922), and classified into O and non-O. We determined history of stroke and myocardial infarction by interview, consultation of medical records, and abnormalities on electrocardiography.
Measurement of other blood markers
In a subset of 1075 non-demented participants, we measured at baseline 150 plasma markers via multiplex immunoassay on human multianalyte profiles in the fasting blood samples collected at baseline (Myriad RBM Inc., Austin TX, USA; http://rbm.myriad.com). Of these, we selected markers with an identified role in angiogenesis (i.e. angiopoietin-2 (ANG-2), vascular endothelial growth factor (VEGF), platelet-derived growth factor (PDGF), transforming growth factors α and β (TGF-α, TGF-β)) or related to the extracellular matrix (i.e. matrix metalloproteinases MMP-2, MMP-3, and MMP-9, tissue inhibitor of metalloproteinase-1 (TIMP-1), Tenascin-C, connective tissue growth factor (CTGF)), based on suggested roles of ADAMTS13 beyond regulation of thrombosis13. The assay did not pass quality control (>20% unmeasurable) for TGF-α, TGF-β, MMP-2, MMP-9 and CTGF, leaving 6 markers for analysis (all with measurements in ≥92.4% of participants).
Analysis
Because of a right-skewed distribution of VWF and the ADAMTS13:VWF-ratio, we performed a natural logarithmic transformation to obtain a roughly normal distribution of the data. We computed Z-scores for each individual by dividing the difference between the individual value and the population mean by the population standard deviation.
Missing covariate data (15.0% for ABO blood type, and <5.0% for all other covariables) were imputed using 5-fold multiple imputation. Distribution of covariates was similar in the imputed versus non-imputed dataset. All analyses were adjusted for age, sex, and study subcohort. In a second model we further adjusted for systolic and diastolic blood pressure, use of antihypertensive medication, serum total cholesterol, high-density lipoprotein (HDL) cholesterol and triglycerides, use of lipid-lowering medication, body mass index, diabetes mellitus, creatinine, CRP, fibrinogen, ABO blood type, and use of antithrombotic medication.
We determined the association of VWF and ADAMTS13 with prevalence and incidence of dementia, using logistic regression and Cox proportional hazard models, respectively. As the proportional hazard assumption was violated for VWF, we also determined associations with dementia risk per year increase in follow-up. We determined risk of dementia per standard deviation (SD) increase as well as per quartile of VWF, ADAMTS13, and their ratio. In view of previously suggested threshold effects of ADAMTS13, we also compared the lowest quartile of ADAMTS13 to the highest three quartiles altogether2. We assessed effect modification by (pre-)diabetes, by testing for multiplicative interaction in the fully adjusted Cox model. We repeated the analysis after excluding participants with prevalent myocardial infarction or stroke, while censoring at time of incident myocardial infarction or stroke in the fully adjusted model. We performed further sensitivity analyses, 1) for Alzheimer’s disease only, 2) stratifying by the mean age of the study population (i.e. 69.3 years), 4) stratifying by sex, and 5) stratifying by blood type O versus non-O.
We then determined the association of VWF levels and ADAMTS13 activity with change in scores on cognitive assessment during follow-up, using linear mixed models. We fitted a model (restricted maximum likelihood) to the G-factor of cognitive scores, including age, sex, follow-up time, time*age, VWF/ADAMTS13, and time*VWF/ADAMTS13 in the model. We chose a diagonal covariance structure (heterogeneous variance and zero correlation between elements) for the random effects, including a random intercept and follow-up time, and added other covariates in agreement with the fully adjusted model described above. We repeated the analysis for all cognitive tests, stratified by diabetic status, and limited to the 1st, 2nd, and 3rd follow-up examination, respectively.
Finally, in the subset of participants with immunoassay data, we determined correlations of ADAMTS13 with ANG-2, VEGF, PDGF, MMP-3, TIMP-1, and Tenascin-C, using linear regression (of natural log-transformed values if so required to obtain normal distributions of the data). Values exceeding ± 3.5 standard deviations from the mean were excluded from analysis. We fitted univariable models, and additional models including age, sex, and each of the other biomarkers, whilst applying the Benjamini-Hochberg correction for multiple testing.
All analyses were done using SPSS Statistics 21.0 (IBM Corp, Armonk, NY, USA) or R statistical software 3.1.1 (package ‘nlme’). Alpha level was set at 0.05.
Results
Among 6,692 eligible participants, we could not determine VWF antigen in 380 participants and ADAMTS13 activity in 628 participants, mainly due to technical reasons or insufficient blood sampling, leaving 6055 (90.5%) participants with both measures for analyses. Baseline characteristics of the study population are presented in Table 1.
Prevalent dementia
At baseline, 85 participants had dementia, of whom 68 had Alzheimer’s disease. Participants with dementia had higher VWF antigen levels and lower ADAMTS13 activity than individuals without dementia (Table 2). Consequently, the ADAMTS13:VWF ratio was also lower in individuals with dementia, although adjustment for ADAMTS13 did not change the estimates for VWF, and ADAMTS13 did not modify the association of VWF with dementia (Table 2; P-interaction = 0.93). Associations of VWF and ADAMTS13 with dementia were mildly attenuated for Alzheimer’s disease only, and broadly unaltered by excluding participants with cardiovascular disease (Supplementary Table S1).
Longitudinal assessment
Of 5,970 non-demented participants at baseline, 821 participants were diagnosed with dementia during a mean follow-up of 11.6 years (follow-up was complete for 97.5% of potential person years). Of all dementia diagnoses, 671 were due to Alzheimer’s disease, and 154 were preceded by myocardial infarction or a stroke. At baseline, 5,844/5,970 (97.9%) participants underwent extensive cognitive assessment, of whom 4,582 (78.4%) underwent at least 2 assessments, and 2,934 (50.2%) attended at least three examinations.
VWF and cognitive decline/ incident dementia
Overall, VWF antigen levels were not associated with risk of dementia (adjusted HR per SD increase: 1.05, 0.97–1.14). VWF levels were, however, associated with short-term risk of dementia, but these associations attenuated over time and were no longer statistically significant beyond 4 years of follow-up (Fig. 1A; for a full table see Supplementary Table S2). Similarly, associations of VWF with cognitive test performance at baseline extended to the first re-examination at 4.4 years, but not thereafter (Fig. 1B; for results per quartile of VWF see Supplementary Table S3). The associations of VWF with cognitive decline and risk of dementia were not affected by concurrent ADAMTS13 activity (P-value for the interaction VWF*ADAMTS13 = 0.58 for all-cause dementia and and 0.85 the G-factor).
Von Willebrand factor (VWF) in relation to risk of dementia and cognitive performance over time. (A) Cross-sectional estimates at baseline (odds ratio from logistic regression) are followed by hazard ratios for the risk of incident dementia in longitudinal analyses including one extra year of follow-up from baseline per presented figure (Cox regression). Results are from the fully adjusted model. HR = hazard ratio; CI = confidence interval; SD = standard deviation. (B) Results reflect the betas per standard deviation increase for baseline VWF and the VWF*follow-up time interaction (expressed per 10 years follow-up) from a fully adjusted linear mixed model including all four examinations, and restricting analyses to the first two or three assessments, respectively. T0 = baseline; T1 = first follow-up examination after 4.4 years; T2 = second follow-up examination after 10.8 years; T3 = third follow-up examination after 15.4 years. Lower scores reflect worse performance for all tests. Presented cross-sectional estimates from the model including all examinations were robust in the time-restricted models.
ADAMTS13 and cognitive decline/ incident dementia
Low ADAMTS13 activity was associated with an increased risk of dementia (Table 3), with similar effect estimates throughout follow-up. The association was modified by the presence of impaired fasting glucose or diabetes (P-interaction = 0.003), such that low activity of ADAMTS13 related to higher risk of dementia primarily in non-diabetics, but not in those with (pre-)diabetes (Table 3). This opposite direction of effect was similar for impaired fasting glucose and diabetes (Supplementary Table S4), and unaffected by excluding individuals using antidiabetic medication. Risk estimates of ADAMTS13 itself were consistently stronger than those of the ADAMTS13:VWF ratio (Supplementary Table S5), and in contrast to ADAMTS13 there was no interaction between (pre-)diabetes and VWF on the risk of dementia (P-value for the VWF*(pre-)diabetes interaction = 0.99).
ADAMTS13 was associated with more rapid decline in cognitive test performance during 15 years of follow-up (Fig. 2), which was again most profound in individuals without diabetes (Supplementary Table S6). The ADAMTS13:VWF ratio was also associated with change in cognitive test performance, with similar effect estimates, except for a somewhat stronger association with performance on the Stroop test (Supplementary Table S7). Associations were broadly unaltered after excluding all participants who developed dementia during follow-up (Supplementary Table S8).
ADAMTS13 activity and change in cognitive test scores during four consecutive examination rounds. Change in cognitive performance per 10 years of follow-up, expressed per quartile of ADAMTS13 relative to the highest quartile, and comparing low versus normal ADAMTS13 activity. Lower scores reflect worse performance for all tests. Model adjusted for age, sex, smoking, systolic and diastolic blood pressure, antihypertensive medication, serum cholesterol, HDL cholesterol and triglycerides, lipid-lowering medication, body mass index, diabetes, creatinine, antithrombotic medication, CRP, fibrinogen, ABO blood type, and APOE genotype.
Sensitivity analyses
In further sensitivity analyses, associations of VWF and ADAMTS13 with dementia were similar for Alzheimer’s disease only, and unaffected by excluding those with prevalent cardiovascular disease and censoring participants at time of myocardial infarction or stroke during follow-up (Supplementary Figure S1). We found no evidence of effect modification by age at blood sampling, sex, or ABO blood type (Supplementary Figure S1; all P-values for interaction ≥ 0.15).
ADAMTS13 and immunoassay markers
Among a random subset of 1075 participants with immunoassay biomarker measurements, lower ADAMTS13 activity was significantly associated with higher levels of VEGF, MMP-3, and Tenascin-C, but not ANG-2 and PDGF (Table 4). The univariable association between MMP-3 and ADAMTS13 attenuated after adjustment for age and sex, but differed substantially by concurrent levels of TIMP-1 (P-value for interaction = 0.01), such that associations were strongest in the presence of high TIMP-1. A similar interaction was seen between Tenascin-C and TIMP-1 (P-value for interaction = 0.05).
Discussion
In this large population-based study, we found that higher VWF antigen levels are associated with prevalence and short-term, but not long-term risk of dementia. Low ADAMTS13 activity is associated with dementia risk during prolonged follow-up, with data suggesting an interactive mechanisms between ADAMTS13 and diabetes in the development of dementia. We did not observe synergistic effects of VWF and ADAMTS13 activity, which might indeed indicate in part independent underlying mechanisms.
The cross-sectional association between VWF and dementia in our study is in line with a recent meta-analysis, which reported similar (standardised) differences in VWF levels between individuals with all-cause dementia and controls10. However, we found associations to rapidly attenuate over the first few years of follow-up, explaining why two prior longitudinal studies did not find a significant association between VWF and risk of dementia after 4 and 17 years of follow-up, respectively11,12. The crucial role of time in this association could indicate high variability in VWF levels, either physiologically or induced by disease processes or treatment. Levels of VWF in the bloodstream may increase exponentially during the course of disease due to increasing severity of endothelial injury, and the biological effect of VWF may also vary with physiological changes in advanced stages of disease, such as wall shear stress23,24. This physiological variability could be investigated in future studies by incorporation of multiple measurements of VWF over time, which will prove important to determine to which extent prior associations of VWF with (subclinical) disease in fact reflect physiological activity of VWF, or are due to endothelial injury.
VWF has been associated with markers of cerebral small-vessel disease that are known risk factors for dementia25,26, including white matter hyperintensities on MRI and microhaemorrhages co-localised with beta-amyloid deposits27,28. As high VWF increases the risk of ischaemic stroke29, cerebral ischaemia could further link VWF to cognitive decline via (covert) brain infarcts or cortical micro-infarcts.
Such effects might be reduced in individuals with blood type O30, due to accelerated clearance and thus 25% lower levels of VWF31,32, although we did not find differential effects of VWF across blood type in our study. Beyond its direct effects, the function of VWF as a carrier protein for coagulation factor VIII (FVIII), thereby prolonging its half-life 10-fold33, might in part explain recently reported cognitive impairment with higher FVIII30. Finally, in vitro study suggests that inflammatory cytokines increase release and inhibit cleavage of VWF34, which might link inflammatory and ischaemic pathways in the pathogenesis of Alzheimer’s disease14. Future studies linking measurements of VWF to (longitudinal) magnetic resonance neuroimaging may further unravel these potential mechanisms.
In contrast to findings for VWF antigen, low ADAMTS13 activity was associated with cognitive decline and dementia risk throughout the 15-year follow-up in individuals without (pre-)diabetes. In line with reports of myocardial infarction and ischaemic stroke5,8, we observed increased risks only in the lower range of ADAMTS13, supporting a threshold effect in ADAMTS13 activity2. Nevertheless, the lower range of activity in the community is generally sufficient to maintain the equilibrium of VWF multimer formation and degradation35,36. Along with the effect estimates for ADAMTS13 generally exceeding those of the ADAMTS13:VWF ratio, this renders it unlikely that proteolytic effects of ADAMTS13 on VWF alone are accountable for the association of ADAMTS13 with dementia. Yet, most studies about ADAMTS13 have focused on its relationship with VWF or role in thrombotic thrombocytopenic purpura, and limited data are available to corroborate other pathways. Preliminary evidence suggests a role of ADAMTS13 in (downregulation of) inflammation13,37, regulation of angiogenesis13, and degradation of extracellular matrix13, which have also been described in dementia14,15,16. In mice, deficiency of ADAMTS13 enhances inflammation and plaque formation38,39, aggravates consequences of cerebral ischaemia40,41,42, and appears to regulate blood-brain barrier permeability43, possibly by controlling vascular remodeling via VEGF, ANG-2, and galectin-3 related pathways42,43. While these processes in mice often appear dependent on VWF or are observed in ADAMTS-/- mice, the levels required may be limited, and thus generally abundant in the general population. In exploratory analyses, we found associations of ADAMTS13 activity with levels of VEGF, MMP-3, Tenascin-C, and TIMP-1, which might indeed indicate involvement in vascular remodelling, and in any case encourage further study of ADAMTS13 in relation to vascular (brain) disease and neurodegeneration.
Our findings suggest that diabetes pathophysiology, rather than antidiabetic medication, modifies the association between ADAMTS13 and dementia risk. These analyses were prompted by our recent study in which we found increased risks of diabetes with higher ADAMTS13 activity17. Although the mechanisms underlying these observations are unknown, it is conceivable that ADAMTS13 has other, yet unidentified proteolytic activity, or competes/ interacts with glucose or currently unknown protein(s) to contribute to cognitive decline. One would expect that the pathological mechanism underlying this interaction shows similarly in the association of ADAMTS13 with related disease outcomes. A previous report of the Rotterdam Study has described an increased risk of ischaemic stroke with low ADAMTS13 activity5, but the link between ADAMTS13 and diabetes had not yet emerged at the time. Exploring these data further in a post-hoc analysis, we now observed patterns in the association between ADAMTS13 and risk of ischaemic stroke, similar to those with dementia in the current study (HR [95% CI] per SD decrease in ADAMTS13 for risk of ischaemic stroke in those free of (pre-)diabetes: 1.19 [1.04–1.36], versus in those with (pre-)diabetes: 0.94 [0.79–1.11]). This points towards a vascular disease related interactive mechanism, in which ADAMTS13 has a common role across diseases outcomes. While we encourage attempts for replication of our findings in other populations, we believe that current insight warrants serum glucose and diabetes history to be taken into account in future study of ADAMTS13.
Although we believe our results are reliable, there are several limitations. First, despite rigorous adjustment for known determinants of VWF and ADAMTS13, residual confounding may still exist, in particular with respect to other factors involved in hemostasis, diabetes, or possibly angiogenesis and extracellular matrix stability. Second, although follow-up for dementia was near-complete, attrition for repeated detailed cognitive assessment was substantial. Third, the association between ADAMTS13 and diabetes was first described in the same cohort as drawn from in the present analyses, and (large-scale) replication is warranted. Fourth, the Rotterdam Study population is predominantly of Caucasian descent, and levels and effects of ADAMTS13 might differ across ethnicities.
In conclusion, higher VWF and low ADAMTS13 activity are associated with accelerated cognitive decline and increased risk of dementia. However, associations with VWF are restricted to short-term risks, and do not display synergistic effects with ADAMTS13 on dementia risk. The impact of diabetes on the effect of ADAMTS13 on dementia (as well as ischaemic stroke), further emphasises the need to unravel the biological function of ADAMTS13.
References
Leebeek, F. W. G. & Eikenboom, J. C. J. Von Willebrand’s Disease. N Engl J Med. 375, 2067–2080 (2016).
Sonneveld, M. A. H., de Maat, M. P. M. & Leebeek, F. W. G. Von Willebrand factor and ADAMTS13 in arterial thrombosis: a systematic review and meta-analysis. Blood Rev. 28, 167–178 (2014).
Petersen, A.-K. et al. On the hypothesis-free testing of metabolite ratios in genome-wide and metabolome-wide association studies. BMC Bioinformatics. 13, 120 (2012).
Maino, A. et al. Plasma ADAMTS-13 levels and the risk of myocardial infarction: an individual patient data meta-analysis. J Thromb Haemost. 13, 1396–1404 (2015).
Sonneveld, M. A. H. et al. Low ADAMTS13 activity is associated with an increased risk of ischemic stroke. Blood. 126, 2739–2746 (2015).
Andersson, H. M. et al. High VWF, low ADAMTS13, and oral contraceptives increase the risk of ischemic stroke and myocardial infarction in young women. Blood. 119, 1555–1560 (2012).
Bongers, T. N. et al. Lower levels of ADAMTS13 are associated with cardiovascular disease in young patients. Atherosclerosis. 207, 250–254 (2009).
Sonneveld, M. A. et al. Low ADAMTS-13 activity and the risk of coronary heart disease - a prospective cohort study: the Rotterdam Study. J Thromb Haemost. 14, 2114–2120 (2016).
Gardener, H., Wright, C. B., Rundek, T. & Sacco, R. L. Brain health and shared risk factors for dementia and stroke. Nat Rev Neurol. 11, 651–657 (2015).
Quinn, T. J. et al. Association between circulating hemostatic measures and dementia or cognitive impairment: systematic review and meta-analyzes. J Thromb Haemost. 9, 1475–1482 (2011).
Carcaillon, L. et al. Elevated plasma fibrin D-dimer as a risk factor for vascular dementia: the Three-City cohort study. J Thromb Haemost. 7, 1972–1978 (2009).
Gallacher, J. et al. Is sticky blood bad for the brain?: Hemostatic and inflammatory systems and dementia in the Caerphilly Prospective Study. Arterioscler Thromb Vasc Biol. 30, 599–604 (2010).
Feng, Y. et al. ADAMTS13: more than a regulator of thrombosis. Int J Hematol. 104, 534–539 (2016).
Heppner, F. L., Ransohoff, R. M. & Becher, B. Immune attack: the role of inflammation in Alzheimer disease. Nat Rev Neurosci. 16, 358–372 (2015).
Rempe, R. G., Hartz, A. M. & Bauer, B. Matrix metalloproteinases in the brain and blood-brain barrier: Versatile breakers and makers. J Cereb Blood Flow Metab. 36, 1481–1507 (2016).
Qin, W. et al. Elevated plasma angiogenesis factors in Alzheimer’s disease. J Alzheimers Dis. 45, 245–252 (2015).
de Vries, P. S. et al. ADAMTS13 activity as a novel risk factor for incident type 2 diabetes mellitus: a population-based cohort study. Diabetologia. 60, 280–286 (2017).
Hofman, A. et al. The Rotterdam Study: 2016 objectives and design update. Eur J Epidemiol. 30, 661–708 (2015).
Kokame, K., Nobe, Y., Kokubo, Y., Okayama, A. & Miyata, T. FRETS-VWF73, a first fluorogenic substrate for ADAMTS13 assay. Br J Haematol. 129, 93–100 (2005).
Hoogendam, Y. Y., Hofman, A., van der Geest, J. N., van der Lugt, A. & Ikram, M. A. Patterns of cognitive function in aging: the Rotterdam Study. Eur J Epidemiol. 29, 133–140 (2014).
de Bruijn, R. F. A. G. et al. The potential for prevention of dementia across two decades: the prospective, population-based Rotterdam Study. BMC Med. 13, 132 (2015).
World Health Organization, International Diabetes Federation. Definition and diagnosis of diabetes mellitus and intermediate hyperglycemia: report of a WHO/IDF consultation. 2006.
Tsai, H. M., Sussman, I. I. & Nagel, R. L. Shear stress enhances the proteolysis of von Willebrand factor in normal plasma. Blood. 83, 2171–2179 (1994).
Siedlecki, C. A. et al. Shear-dependent changes in the three-dimensional structure of human von Willebrand factor. Blood. 88, 2939–2350 (1996).
Debette, S. & Markus, H. S. The clinical importance of white matter hyperintensities on brain magnetic resonance imaging: systematic review and meta-analysis. BMJ. 341, c3666 (2010).
Akoudad, S. et al. Association of Cerebral Microbleeds With Cognitive Decline and Dementia. JAMA Neurol. 73, 934–943 (2016).
Kearney-Schwartz, A. et al. Vascular structure and function is correlated to cognitive performance and white matter hyperintensities in older hypertensive patients with subjective memory complaints. Stroke. 40, 1229–1236 (2009).
Cullen, K. M., Kócsi, Z. & Stone, J. Microvascular pathology in the aging human brain: evidence that senile plaques are sites of microhaemorrhages. Neurobiol Aging. 27, 1786–1796 (2006).
Wieberdink, R. G. et al. High von Willebrand factor levels increase the risk of stroke: the Rotterdam study. Stroke. 41, 2151–2156 (2010).
Alexander, K. S. et al. ABO blood type, factor VIII, and incident cognitive impairment in the REGARDS cohort. Neurology. 83, 1271–1276 (2014).
Gill, J. C., Endres-Brooks, J., Bauer, P. J., Marks, W. J. & Montgomery, R. R. The effect of ABO blood group on the diagnosis of von Willebrand disease. Blood. 69, 1691–1695 (1987).
Gallinaro, L. et al. A shorter von Willebrand factor survival in O blood group subjects explains how ABO determinants influence plasma von Willebrand factor. Blood. 111, 3540–3545 (2008).
Koedam, J. A., Meijers, J. C., Sixma, J. J. & Bouma, B. N. Inactivation of human factor VIII by activated protein C. Cofactor activity of protein S and protective effect of von Willebrand factor. J Clin Invest. 82, 1236–1243 (1988).
Bernardo, A., Ball, C., Nolasco, L., Moake, J. F. & Dong, J.-F. Effects of inflammatory cytokines on the release and cleavage of the endothelial cell-derived ultralarge von Willebrand factor multimers under flow. Blood. 104, 100–106 (2004).
Mannucci, P. M. et al. Changes in health and disease of the metalloprotease that cleaves von Willebrand factor. Blood. 98, 2730–2735 (2001).
Coppo, P. et al. Predictive features of severe acquired ADAMTS13 deficiency in idiopathic thrombotic microangiopathies: the French TMA reference center experience. PLoS One. 5, e10208 (2010).
Chauhan, A. K. et al. ADAMTS13: a new link between thrombosis and inflammation. J Exp Med. 205, 2065–2074 (2008).
Gandhi, C., Khan, M. M., Lentz, S. R. & Chauhan, A. K. ADAMTS13 reduces vascular inflammation and the development of early atherosclerosis in mice. Blood. 119, 2385–2391 (2012).
Gandhi, C., Ahmad, A., Wilson, K. M. & Chauhan, A. K. ADAMTS13 modulates atherosclerotic plaque progression in mice via a VWF-dependent mechanism. J Thromb Haemost. 12, 255–260 (2014).
Fujioka, M. et al. ADAMTS13 gene deletion enhances plasma high-mobility group box 1 elevation and neuroinflammation in brain ischemia-reperfusion injury. Neurol Sci. 33, 1107–1115 (2012).
Zhao, B.-Q. et al. von Willebrand factor-cleaving protease ADAMTS13 reduces ischemic brain injury in experimental stroke. Blood. 114, 3329–3334 (2009).
Xu, H. et al. ADAMTS13 controls vascular remodeling by modifying VWF reactivity during stroke recovery. Blood. 130, 11–22 (2017).
Wang, L. et al. Recombinant ADAMTS13 reduces tissue plasminogen activator-induced hemorrhage after stroke in mice. Ann Neurol. 73, 189–198 (2013).
Acknowledgements
We acknowledge the support from the Netherlands CardioVascular Research Initiative: the Dutch Heart Foundation, Dutch Federation of University Medical Centres, the Netherlands Organisation for Health Research and Development, and the Royal Netherlands Academy of Sciences. The Heart Brain Connection collaborative research group includes Mark A. van Buchem, Geert Jan Biessels, Hans-Peter Brunner la Rocca, Anton J.de Craen†, Wiesje M. van der Flier, M. Arfan Ikram, L. Jaap Kappelle, Peter J. Koudstaal, Simon P. Mooijaart, Wiro Niessen, Robert van Oostenbrugge, Albert de Roos, Albert C. van Rossum, and Mat J. Daemen. The dedication, commitment, and contribution of study participants, general practitioners, and pharmacists of the Ommoord district to the Rotterdam Study are gratefully acknowledged. We thank all staff at the Rotterdam Study research centre, facilitating assessment of participants throughout the years, and acknowledge the valuable support of Frank J.A. van Rooij as data manager. The Heart Brain Connection collaborative research group is supported by the Netherlands Cardiovascular Research Initiative (CVON2012–06). The Rotterdam Study is sponsored by the Erasmus Medical Centre and Erasmus University Rotterdam, The Netherlands Organization for Scientific Research (NWO), The Netherlands Organization for Health Research and Development (ZonMW), the Research Institute for Diseases in the Elderly (RIDE), The Netherlands Genomics Initiative, the Ministry of Education, Culture and Science, the Ministry of Health, Welfare and Sports, the European Commission (DG XII), and the Municipality of Rotterdam. Further support was obtained from the Netherlands Consortium for Healthy Ageing and the Dutch Heart Foundation (2012T008). The present study was supported by Shire as an unrestricted research grant to F.W.G. Leebeek. This research was further supported by funding from the European Union Seventh Framework Program (FP7/2007e2013) under grant agreement no. 601055, VPH-Dare@IT (FP7-ICT-2011-9e601055); and funding from the European Union’s Horizon 2020 research and innovation program under grant agreement no. 667375 (Co-STREAM) and under grant agreement no. 678543 (European Research Council (ERC) funded project: ORACLE). None of the funding organizations or sponsors were involved in study design, in collection, analysis, and interpretation of data, in writing of the report, or in the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
All authors have made a substantial intellectual contribution to design of the study (M.A.I., F.W.L.), acquisition of data (F.J.W., P.J.K., M.K.I.), analysis and interpretation of data (F.J.W., J.B., P.S.d.V., M.A.S., P.J.K., M.P.d.M., O.H.F., M.K.I., F.W.L., M.A.I.), drafting the manuscript (F.J.W.), or revising it critically for important intellectual content (J.B., P.S.d.V., M.A.S., P.J.K., M.P.d.M., O.H.F., M.K.I., F.W.L., M.A.I.). All authors approved the final version of the manuscript for publication. M.A.I. had full access to the data in the study and takes responsibility for data integrity and accuracy of data analysis.
Corresponding author
Ethics declarations
Competing Interests
Dr. Leebeek is a consultant for uniQure, Shire, and NovoNordisk (fees to the institution), and has received research funding of CSL Behring and Shire. Dr. De Maat reports grants from Baxter Innovations GmbH, during the conduct of the study. Dr. Franco reports grants from Nestle and Metagenics, outside the submitted work. Dr. Boender reports a grant from CSL Behring, outside the submitted work. The other authors state that they have no conflict of interest.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wolters, F.J., Boender, J., de Vries, P.S. et al. Von Willebrand factor and ADAMTS13 activity in relation to risk of dementia: a population-based study. Sci Rep 8, 5474 (2018). https://doi.org/10.1038/s41598-018-23865-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-23865-7
This article is cited by
-
Multi-ancestry meta-analysis and fine-mapping in Alzheimer’s disease
Molecular Psychiatry (2023)
-
Plasma proteome profiling identifies changes associated to AD but not to FTD
Acta Neuropathologica Communications (2022)
-
Hemostasis components in cerebral amyloid angiopathy and Alzheimer’s disease
Neurological Sciences (2021)
-
The disjunctive cause criterion by VanderWeele: An easy solution to a complex problem?
European Journal of Epidemiology (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.