Abstract
Exposure to environmental polycyclic aromatic hydrocarbons (PAHs), such as benzo(a)pyrene (B(a)P), has been linked to several health-threatening risks. PAHs were also shown to hinder adrenergic receptor (ADR) responses. As we previously demonstrated that B(a)P can directly interact with the β2ADR, we investigated here whether B(a)P could decrease β2ADR responsiveness by triggering receptor desensitization phenomena. We firstly showed that exposure to B(a)P reduced β2ADR-mediated epinephrine-induced induction of NR4A gene mRNAs and of intracellular cAMP. Analysis of β2ADR protein expression demonstrated that B(a)P rapidly decreased membrane expression of β2ADR with a subsequent degradation of receptor protein. B(a)P exposure concomitantly rapidly increased the β2ADR mRNA levels. The use of the β-blockers, propranolol and ICI 118.551, demonstrated the involvement of β2ADR itself in this increase. However, sustained exposure to B(a)P induced a diminution of β2ADR mRNA steady-state as a result of the acceleration of its degradation. Together, these results show that, beside the well-known activation of the aryl hydrocarbon receptor, PAH deleterious effects may involve the dysfunction of adrenergic responses through, in part, the desensitization of β2ADR. This may be taken in consideration when β2-agonists/antagonists are administered in patients exposed to important concentrations of PAHs, e.g. in cigarette smokers.
Similar content being viewed by others
Introduction
Polycyclic aromatic hydrocarbons (PAHs), such as the prototypical molecule benzo(a)pyrene (B(a)P), constitute an ubiquitous family of environmental contaminants, that are notably found in cigarette smoke, exhaust particles, grilled foods and industrial waste by-products1, 2. Exposure to these pollutants has been correlated to various pathological situations, including inflammation, cancer development, cardiovascular and pulmonary diseases3, 4. Therefore, PAHs have been classified as priority toxicants by the United States Environmental Protection Agency (US-EPA), the World Health Organization (WHO) and the European Union5. Most of the PAH-related deleterious effects are mediated by activation of the cytosolic aryl hydrocarbon receptor (AhR), and its subsequent binding to specific xenobiotic responsive elements which are found in the promoter of PAH-responsive genes6. However, some PAH-related effects may be initiated in an AhR-independent manner, e.g. the transient increase in intracellular calcium concentration by B(a)P7 and the induction of CXCL8 by nitro-PAHs8, 9. Our attempts to explain these AhR-independent effects have recently revealed an important role of β2-adrenergic receptor (β2ADR) signaling pathway10, 11. Interestingly, this role seems to involve a direct activation of β2ADR by PAHs, thus adding these pollutants to the list of β2ADR-interacting agents10.
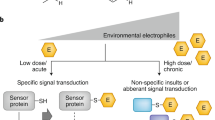
β2ADR is a G-protein coupled receptor (GPCR), that is originally activated by catecholamines, i. e. adrenaline or epinephrine (EN) and noradrenaline or norepinephrine, resulting in the regulation of crucial physiological functions, including the control of smooth muscle contraction, blood pressure, bronchodilation, and of glycogenolysis12, 13. Upon stimulation, β2ADR activates the adenylyl cyclase (AC) via a Gs protein, leading to production of cAMP from ATP and activation of downstream effectors, such as protein kinase A (PKA) and exchange protein factor directly activated by cAMP (EPAC)14. In parallel to the activation of these signaling pathways, exposure to β2-agonists leads to receptor desensitization; i.e. agonist-induced time-dependent loss of β2ADR responsiveness. This negative feedback loop is a multi-step process that results in the reduction of receptor number at both the surface and the inner of the cell by (i) the degradation of the receptor itself after its internalization, and (ii) the decrease of its synthesis via the acceleration of mRNA decay15.
Interestingly, exposure to PAHs, or to PAH-related pollutants such as the carcinogenic halogenated 2,3,7,8-tetrachlorodibenzo-para-dioxin (TCDD), has been correlated to desensitization-like effects on β2ADR. Indeed, exposure to some environmentally relevant PAHs impaired β2ADR-mediated airway relaxation in human, resulting in a reduced responsiveness to standard therapy of asthma16. Moreover exposure to TCDD decreased β-adrenergic responsiveness in chick embryo cardiac muscle cells17. These observations highlight the impact of PAH exposure on β2ADR responsiveness. However, to date, understanding of the underlying molecular mechanisms is still limited.
The present study was thus designed to investigate the effect of B(a)P exposure on β2ADR responsiveness to EN in a human cardiovascular cell model, and to verify whether this effect was associated to β2ADR desensitization through focusing on the related cellular mechanisms. Our results revealed that B(a)P decreased the receptor responsiveness to β2-agonists with a concomitant β2ADR internalization and, for more sustained exposures, receptor degradation at both protein and mRNA levels.
Results
Validation of cell model for the study of β2ADR activation by EN
For this work, we used the physiological catecholamine EN as a referent agonist of β2ADR activation. As a study cell model, the human microvascular endothelial cells HMEC-1 were used since they constitute an established model for the study of β2ADR activation10, and since they are derived from the cardiovascular system, known to be a major target of PAH toxicity3. To validate this choice, the effects of EN on the expression of nuclear receptor 4A (NR4A) mRNAs were evaluated in the presence or absence of β2ADR-antagonists (Fig. 1). Indeed, NR4A subfamily is a group of orphan nuclear receptors, including Nur77 (NR4A1), Nurr1 (NR4A2), and NOR1 (NR4A3), whose expressions are rapidly induced by EN through the activation of β2ADR pathway18. As expected, EN induced mRNA expression of NR4A1, 2 and 3 in HMEC-1 cells after 1 h of exposure, in a dose-dependent manner (Fig. 1a,b,c respectively). This effect was strongly hindered by antagonizing β2ADR using the non-selective β-blocker propranolol, or the selective β2-blocker ICI 118.551 (Fig. 1a,b,c), thus demonstrating the involvement of β2ADR in the induction of NR4A genes by EN in our cell model, in accordance with previous reports19. This involvement was further consolidated by the ability of the selective β2ADR-agonist salbutamol to increase mRNA level of NR4A family members in a dose-dependent manner (Supplementary Figure S1).
B(a)P decreased β2ADR-mediated induction of NR4As expression triggered by epinephrine (EN). (a,b,c) HMEC-1 cells were either untreated or exposed to indicated concentrations of EN for 1 h, in the presence or not of 10 µM propranolol (nonselective β-blocker) or 10 µM ICI 118.551 (selective β2-bloker). mRNA expressions of β2ADR-target genes, NR4A1 (a), NR4A2 (b) and NR4A3 (c) were next determined by RT-qPCR. (d,e,f) HMEC-1 cells were exposed to indicated concentrations of B(a)P or vehicule (DMSO) for 24 h before being co-exposed, or not, to 10 µM EN for 1 h. mRNA expressions of β2ADR-target genes, NR4A1 (d), NR4A2 (e) and NR4A3 (f) were next determined by RT-qPCR. Data are expressed relatively to mRNA levels found in untreated cells, arbitrarily set to 1 unit, and are the means ± S.D of at least three independent assays. *p < 0.05; **p < 0.01 when compared to B(a)P-untreated cells.
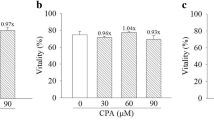
B(a)P decreased β2ADR-mediated EN-triggered induction of NR4As expression
To test whether B(a)P was able to desensitize β2ADR responsiveness to EN, we evaluated the impact of B(a)P pre-exposure on EN-induced NR4As expressions. HMEC-1 cells were exposed during 24 h to various concentrations of B(a)P (0, 0.1, 1, or 10 µM), and then co-exposed during 1 h to 10 µM EN before analyzing NR4As mRNA levels. As shown in Fig. 1, B(a)P pretreatment, which did not affect cell viability whatever the dose used (Supplementary Figure S2), strongly decreased the EN-induced enhancement of mRNA expression of NR4A1 (Fig. 1d), NR4A2 (Fig. 1e) and NR4A3 (Fig. 1f). In addition, the effect of B(a)P was dose-dependent, starting at 0.1 μM and becoming significant from 1 µM.
B(a)P pre-treatment decreased EN-induced intracellular cAMP production
As mentioned above, β2ADR is a member of a specific subfamily of GPCRs that is linked by Gs protein to adenylyl cyclase; upon stimulation, this enzyme hydrolyzes ATP and generates the universal second messenger cAMP which can in turn activate downstream effectors20,21,22. Therefore, the increase of cAMP intracellular concentration is widely considered as a hallmark of β2ADR activation. Accordingly, we found that EN rapidly (10 min) and markedly increased cAMP level in HMEC-1 cells (Fig. 2). To further evaluate the influence of B(a)P pretreatment on β2ADR responsiveness to EN, we therefore decided to analyze the effect of EN on intracellular cAMP concentration, with or without prior exposure to B(a)P. Results showed that B(a)P used at 1 µM for 24 h significantly inhibited the EN-induced cAMP increase, thereby confirming our observation on NR4As mRNAs and the ability of B(a)P to decrease cellular responsiveness to stimulation by EN (Fig. 2).
B(a)P pre-treatment decreased EN-induced intracellular cAMP production. HMEC-1 cells were exposed to 10 μM B(a)P or vehicule (DMSO) for 24 h, and were then co-exposed, or not, to 10 µM EN for 10 min. cAMP levels (pmol/well) were next determined, as described in Materials and Methods section. Data are the means ± S.D of three independent assays. *p < 0.05 when compared to untreated cells; # p < 0.05 when compared to EN treated counterparts.
In order to decipher the mechanisms underlying the B(a)P-induced decrease in cell responsiveness to EN, we hypothesized that B(a)P might trigger β2ADR desensitization as a consequence of their direct interaction previously described in HMEC-1 cells10. To test this hypothesis, we analyzed the impact of B(a)P exposure on i) the number of available β2ADR at cell surface, ii) the potential degradation of the receptor at protein level, and iii) the reduction of receptor synthesis brought about by the decrease of its mRNA stability.
Short-term exposure to B(a)P reduced β2ADR density at cell surface
Agonist-induced reduction in membrane β2ADR density is usually related to receptor internalization after few minutes of exposure to agonist23. To examine the hypothesis that B(a)P might generate such an effect, we performed immunolocalization assays to evaluate the density of β2ADR at the cell surface of HMEC-1 after a 45 min-exposure to 10 µM of EN (used here as a positive control for the activation of β2ADR) or to 1 µM of B(a)P. As previously demonstrated24, activation of β2ADR by EN led to a marked reduction in fluorescent signal at the cell surface, thus reflecting a decrease in receptor number (Fig. 3a). Similarly, exposure to B(a)P reduced the β2ADR signal density (Fig. 3a). To consolidate these results, fluorescence signals were quantified (Supplementary Figure S3). To determine whether this decrease was associated or not with protein degradation, we next realized a Western blot analysis of total protein extracts of HMEC-1 cells treated or not with 1 µM of B(a)P for 45 min. As no reduction of β2ADR protein level was detected (Fig. 3b), results of immunolocalization argue in favor of the internalization of β2ADR without any protein degradation at this time point.
B(a)P triggered an early reduction of β2ADR expression at cell membrane and a late degradation of β2ADR protein. (a) HMEC-1 cells were exposed to 10 µM EN, 1 µM B(a)P or vehicle (DMSO) for 45 min. β2ADR was then analyzed by immunolocalization for the expression at cell membrane. Data shown are representative of three independent assays. (b) HMEC-1 cells were exposed to 1 µM B(a)P or vehicle (DMSO) for 45 min. β2ADR protein content was then determined by Western-blotting. (c) HMEC-1 cells were exposed to indicated concentrations of B(a)P or vehicle (DMSO) for 24 h. β2ADR protein content was then determined by Western-blotting. (b and c) Bottom panel, a representative blot is shown for β2ADR and P38 protein levels. Upper panel, for each concentration of B(a)P, data were quantified by densitometric analysis, normalized to P38 protein level and expressed relative to β2ADR found in untreated cells, arbitrarily set at the value of 100%. Results are the means ± S.D of values from three independent assays. *p < 0.05 when compared to untreated cells.
Sustained exposure to B(a)P triggered β2ADR protein degradation
It is well known that the rapid internalization of β2ADR may be followed, upon sustained stimulation, by its downregulation partly due to the degradation of the receptor protein. In order to investigate the potential role of B(a)P in triggering similar effects, cells were exposed during 24 h to different concentrations of B(a)P (0, 0.1, 1, 5, or 10 µM), before studying β2ADR protein levels by Western blotting of total protein extracts. Results shown in Fig. 3c indicated that B(a)P reduced β2ADR protein level. This effect was detected at all tested doses, but was only statistically significant at 1 and 10 µM of B(a)P (Fig. 3c).
Sustained exposure to B(a)P induced β2ADR mRNA degradation
In addition to the degradation of receptor protein, the agonist-induced down-regulation of β2ADR is also the output of decreased receptor synthesis resulting from the acceleration of its mRNA decay15. We therefore decided to analyze the influence of B(a)P exposure on the β2ADR mRNA expression at several time points in HMEC-1 cells. To do so, cells were exposed to 1 µM B(a)P or 10 µM EN (as a positive control for β2ADR activation) during 0, 0.5, 1, 2, 3, 6 or 8 h before measuring β2ADR mRNA levels.
Figure 4a demonstrates that B(a)P and EN induced similar biphasic modifications on the mRNA level encoding the β2ADR in our cellular model. Indeed, the addition of either B(a)P or EN rapidly increased the expression of β2ADR mRNA, with a peak at 1 h of exposure. This first phase was then followed, after a more sustained exposure, by a reduction in the steady-state mRNA level, with the lowest level reached after 6 h of treatment (reduction by 50% compared to DMSO control condition); a return to basal levels was then observed at 8 h (Fig. 4a).
B(a)P exposure influenced β2ADR mRNA level. (a) HMEC-1 cells were exposed to 10 µM EN, 1 µM B(a)P or vehicle (DMSO) for indicated times before analyzing β2ADR mRNA expressions by RT-qPCR. Data are expressed relatively to mRNA levels found in corresponding control cells, arbitrarily set to 1 unit, and are the means ± S.D of at least three independent assays. *p < 0.05 when compared to corresponding control cells. (b) HMEC-1 cells were exposed to indicated concentrations of B(a)P or vehicle (DMSO) for 1 h. mRNA expressions of β2ADR were then analyzed by RT-qPCR. Data are expressed relatively to mRNA levels found in control cells, arbitrarily set to 1 unit, and are the means ± S.D of at least three independent assays. (c,d) HMEC-1 cells were exposed to 10 µM EN, 1 µM B(a)P or vehicle (DMSO) for 1 h, in the presence or absence of 10 µM actinomycin D (c), or in the presence or absence of 10 µM propranolol or 10 µM ICI 118.551 (d). mRNA expressions of β2ADR were then analyzed by RT-qPCR. Data are expressed relatively to mRNA levels found in corresponding control cells, arbitrarily set to 1 unit, and are the means ± S.D of at least three independent assays. *p < 0.05 when compared with conotrol cells. # p < 0.05 when compared to EN- or B(a)P-treated counterparts. (e,f) HMEC-1 cells were either untreated or exposed (1 h) to 10 µM EN (e), or were exposed to indicated concentrations of B(a)P or vehicle (DMSO) (f), Half-lives of β2ADR mRNA were then calculated as described in Materials and Methods section. Data correspond to mRNA half-lives, expressed in minutes, and are the means ± S.D of three independent assays. *p < 0.05 when compared with untreated cells. # p < 0.05 when compared to EN- or B(a)P-treated counterparts. Representative curves of mRNA decay kinetics in the absence (Ct) or presence of EN are given in the insert (e).
To get more insight about the B(a)P-induced biphasic modulations of β2ADR mRNA level, we then separately studied each of these two phases.
Regarding the early transient increase, it was shown to depend on the concentration of B(a)P used at 1 h of exposure. As demonstrated in Fig. 4b, the effect of B(a)P was from 10 nM of B(a)P and maximal at 1 µM (EC50 = 11.44 ± 2.69 nM). In addition, when HMEC-1 cells were pretreated with the transcriptional inhibitor actinomycin D (5 μg/ml) and then stimulated with B(a)P 1 µM or EN 10 µM (used as a positive control of β2ADR activation) for 1 h, mRNA analysis demonstrates that actinomycin D completely abolished the B(a)P and EN induced effect, as shown in Fig. 4c. Furthermore, the non-selective β-blocker propranolol, and the selective β2-blocker ICI 118.551, both inhibited this induction of β2ADR mRNA level observed in presence of B(a)P and EN (Fig. 4d). These results demonstrate the transcriptional nature of the B(a)P-triggered induction of β2ADR mRNA and the involvement of the receptor itself. Taking into account that similar observations were associated to β2-agonist exposure25, these results pointed to an agonist-like effect of B(a)P on β2ADR.
With regard to the reduction of β2ADR transcript level, it has been suggested that β2-agonists may reduce receptor mRNA stability15. We thus analyzed the influence of B(a)P on the half-life of β2ADR mRNA, as described in Materials and Methods section. Under control conditions, results demonstrated that in our cell model and culture conditions the half-life of β2ADR mRNA was 91.2 ± 13.3 min, in accordance with the literature15. In presence of EN, this half-life value was reduced to 50.6 ± 6.6 min (Fig. 4e), thus indicating an accelerated rate of decay of β2ADR mRNA upon receptor activation. Under the same experimental conditions, we determined β2ADR mRNA half-lives in the presence of various concentrations of B(a)P, i.e., 0, 10, 100, 1000, or 10000 nM. Our results indicated that B(a)P exposure elicited a dose-dependent reduction of β2ADR mRNA half-life (Fig. 4f). This effect was noticeable at 10 nM and significant from 100 nM of B(a)P.
Discussion
We previously demonstrated that the prototypical environmental pollutant B(a)P can directly bind to β2ADR to activate the adenylyl cyclase/cAMP/Epac-1/inositol 1,4,5-trisphosphate/Ca2+ pathway10. While additional studies are needed, those results have suggested that B(a)P could behave like a β2ADR agonist. Since it is well documented that activation of β2ADR initiates a desensitization of the receptor26, the focus was herein on putative β2ADR desensitization phenomena triggered by B(a)P. Our results indicate that the referent PAH is able to markedly reduce HMEC-1 cells’ responsiveness to β2ADR activation by β2-agonists (e.g. EN), as a consequence of receptor desensitization, i.e. receptor internalization followed by receptor mRNA and protein degradation. These results are the first demonstration, to the best of our knowledge, of the molecular mechanisms of the previously documented β2ADR loss-of-function after exposure to PAH and PAH-related contaminants16, 27.
The decrease of β2ADR responsiveness to EN after exposure to PAHs was supported by the capacity of B(a)P (i) to inhibit EN-triggered β2ADR-mediated induction of NR4A1, 2 and 3 expressions and (ii) to reduce the cAMP signal induced by EN. It is noteworthy that this loss of responsiveness to EN was detected at relatively low concentrations of B(a)P (Figs 1d,e,f, 3c and 4f). Even if these concentrations of B(a)P remain higher than those to whom humans are exposed28, one might speculate that synergic effects of various B(a)P-related PAHs, which exist as mixtures in the environment and in cigarette smoke, might contribute to β2ADR loss-of-function at more environmentally relevant concentrations. This hypothesis may be supported by (i) the capacity of other PAHs, such as pyrene (10 µM, 24 h), to diminish EN-induced cAMP increase in HMEC-1 cells (Supplementary Figure S5), and by (ii) previous observations, such as the impairment of β2ADR function in asthmatic children who are exposed to mixtures of PAHs16, and the down-regulation of β2ADR in rat lung alveolar macrophages after chronic exposure to cigarette smoke29.
We reported in this study that short-term exposure to B(a)P, reduced β2ADR number at the cell surface (Fig. 3a). Mechanistically, this effect seems to essentially result from the internalization of β2ADR as no protein degradation was detected at this exposure time (Fig. 3b). However, further studies would be required to confirm this conclusion and to characterize the underlying molecular mechanisms. In this context, it might be interested to consider the phosphorylation of β2ADR by protein kinases, e.g. PKC, β-arrestin or β2-ARK26, as well as the implication of clathrin-coated vesicles known to interfere with agonist-induced β2-ADR internalization30.
We also reported that B(a)P can induce β2ADR down-regulation by enhancing receptor degradation at both mRNA and protein levels (Figs 3c and 4f). It is worthy noting here that B(a)P-induced modulations of mRNAs encoding the β2ADR were of biphasic nature (Fig. 4a): a short-term exposure (up to 1 h) stimulates the transcription of β2ADR mRNA, whereas more prolonged exposure decreases β2ADR mRNA level (Fig. 4a) due to the reduction of β2ADR mRNA half-life associated to the acceleration of mRNAs degradation (Fig. 4f). Interestingly, similar biphasic modifications in β2ADR mRNA expression were also correlated to EN exposure in our cellular model (Fig. 4a), thus confirming previous observations25. Therefore, our results argue in favor of an agonist-like effect of PAHs on β2ADR transcripts. While the functional interpretation of the first increasing phase in the integral β2ADR response is still unclear, it is well documented that the late reduction of β2ADR expression could contribute to the receptor loss-of-function after agonist stimulation31.
To continue this work, it would be interesting to thoroughly study the molecular effectors contributing to PAH-induced biphasic regulation of β2ADR. Indeed, short activation of β2ADR by B(a)P increases intracellular cAMP concentration, via the activation of adenylyl cyclase10. We might speculate that this cAMP elevation could be sufficient to activate a PKA-dependent CREB pathway, thus inducing the transcription of genes containing in their promoter the cAMP responsive element (CRE), such as β2ADR gene. This β2ADR/cAMP/PKA/CREB/CRE pathway is known to exert a positive transcriptional autoregulation26, thereby likely contributing to the early increase in β2ADR mRNA expression observed after receptor activation by B(a)P. However, when receptor stimulation by B(a)P is chronic, desensitization processes would be initiated. In this case, it could be observed the cAMP-dependant activation of β-ADR mRNA-binding protein (β-ARB) or of A/U rich mRNA binding factor (AUF1) that causes the β2ADR mRNA decay. This pathway is usually associated with receptor down regulation observed during desensitization process32, 33. Beside these G protein-dependent mechanisms, the β-arrestin-dependent, G protein-independent pathway may also explain the observed effects on β2ADR mRNA. This β-arrestin-dependent pathway is known to create a link between β2ADR activation and many cellular pathways including the recruitment of c-SRC kinase and the activation of the MAP kinase signaling network, both known to be implicated in the β2ADR desensitization34,35,36,37. Whether B(a)P, by its capacity to activate β2ADR, could trigger this β-arrestin-dependent desensitization pathways will therefore be worth considering.
Interestingly, beside its role in regulating β2ADR desensitization, c-SRC kinase is also known to be associated to the cytosolic AhR multiprotein complex. Binding of AhR ligands, such as B(a)P, to this complex leads to dissociation, activation and translocation to plasma membrane of c-SRC, which may then represent a molecular link between AhR and membrane proteins (including GPCRs) as an element of the non-genomic pathway of AhR38. However, c-SRC kinase is not the only one potential link between the AhR and GPCR pathways; cAMP and intracellular calcium signals are also known to play important roles in both AhR- and GPCR-depending function and regulation. Indeed, AhR ligands as TCDD and B(a)P, are able to increase intracytosolic calcium concentration and/or the production of cAMP10, 39. Both Ca2+ and cAMP represent classical second messengers associated to GPCR activation and desensitization, as known for β2ADR, and also exhibit the capacity to influence the nuclear translocation of AhR40, 41. In this context, the question that arises next is: does it exist a reciprocal regulation between AhR and GPCRs pathways? In line with this, it is noteworthy that similar crosstalk has already been demonstrated between GPCRs and other nuclear receptors such as the glucocorticoid receptor42, 43.
In conclusion, we showed that exposure to B(a)P triggered β2ADR desensitization and consequently reduced cellular capacities to react to the stimulation by the physiological ligand EN. Keeping in mind that functional β2ADR signaling is required for normal cardiovascular and pulmonary44,45,46 as well as for the neurodevelopment47,48,49, and that humans are continuously exposed to PAHs, our work therefore suggests that the interaction between PAHs and β2ADR might contribute to PAHs toxicity, not only by eliciting cellular responses such as calcium signal or CXCL8 release, but also by disrupting of cardiovascular, pulmonary and neurological physiological homeostasis. These results also suggest that even if the majority of cellular effects of PAHs are attributed to AhR activation, the implication of other signaling pathways, such as that of β2ADR, in PAH-related toxicity can no longer be discarded.
Material and Methods
Chemical and Reagents
B(a)P, EN, ICI 118.551, salbutamol, propranolol and actinomycin D were provided by Sigma-Aldrich (Saint-Quentin Fallavier, France). Rabbit monoclonal antibody anti-β2ADR and control antibody were obtained from Santa Cruz Biotechnology (Santa Cruz, CA). All other compounds were commercial products of the highest purity available. Chemicals were used as stock solutions in DMSO; the final concentration of this solvent in culture medium was always <0.2% (v/v), and control cultures received the same dose of vehicle as exposed cultures.
Cell Culture
Human microvascular endothelial cells HMEC-1, obtained from the Center for Disease Control and Prevention (Atlanta, GA), were routinely maintained in MDCB-131 medium containing epidermal growth factor (10 ng/mL), hydrocortisone (1 µg/mL), glutamine (10 mM), penicillin (50 units/ml) and streptomycin (50 µg/ml) and supplemented with 10% fetal calf serum. Before each treatment, cells were cultured over night in medium without calf serum, for serum catecholamines weaning.
Intracellular cAMP Measurements
Cellular concentration of cAMP (pmol/well) was quantified by the chemiluminescent immunoassay cAMP-ScreenTM System (Applied Biosystems, Foster City, CA), according to the manufacturer’s instructions.
RNA Isolation and Analysis
Total RNA was isolated from cells using the TRIzol method (Invitrogen); it was then subjected to reverse transcription real-time quantitative PCR (RT-qPCR) analysis, as previously described50. Primers were as follows: β2ADR-forward: 5′-TTCCTTCCTACACCCTTGGA-3′; β2ADR-reverse: 5′-AGACTTTGCTCGGGAAAACA-3′; NR4A1-forward: 5′GTTCTCTGGAGGTCATCCGCA-3′; NR4A1-reverse: 5′-GACGGGACCTTGAGAAGGCCA-3′; NR4A2-forward: 5′-TATTCCAGGTTCCAGGCGAA-3′; NR4A2-reverse: 5′-GCTAATCGAAGGACAAACAG-3′; NR4A3-forward: 5′-CCAAGCCTTAGCCTGCCTGTC-3′; NR4A3-reverse: 5′-AGCCTGTCCCTTACTCTGGTGG-3′; 18S-forward: 5′-CGCCGCTAGAGGTGAAATTC-3′; 18S-reverse: 5′-TTGGCAAATGCTTTCGCT-3′. The specificity of each gene amplification was verified at the end of qPCR reactions through analysis of dissociation curves of the qPCR products. Amplification curves were analyzed with ABI Prism 7000 SDS software using the comparative cycle threshold method. Relative quantification of the steady-state target mRNA levels was calculated after normalization of the total amount of tested cDNA to an 18S RNA endogenous reference.
mRNA Half-life Determination
We have measured mRNA half-life using a method blocking cellular transcription with actinomycin D51. After 1 h of treatment by EN or B(a)P, actinomycin D (5 µg/ml) was added to culture medium to inhibit de novo mRNA synthesis; then treatments were stopped after 0, 30, 60, 90 or 150 min, and mRNA levels analyzed after extraction, by real time-PCR. The half-life of mRNA was calculated, after linear regression, from the slope of a semilogarithmic plot of mRNA level.
Immunolocalization
Cells were fixed with cold solution of paraformaldehyde (4% in PBS) for 30 min (on ice). After removal of paraformaldehyde, cells were washed with PBS and incubated in PBS containing 2% BSA for 1 h at room temperature. The medium was aspirated and replaced with blocking medium containing primary antibody (isotype control or antibody against β2ADR). After 2 h of incubation at room temperature and three washes with cold PBS, the primary antibody was detected with goat fluorescein-labeled IgG (FITC). Nuclei were stained by 4′,6-diamidino-2-phenylindole (DAPI), for 5 min at room temperature. Images were then acquired with a fluorescence microscope adapted to a high resolution AxioCam camera (Carl Zeiss, Canada).
Immunoblotting Analysis
Immunoblotting was performed on total cellular extracts as previously described52. Briefly, protein samples (40 µg) were subjected to electrophoresis in a 10% acrylamide gel and electrophoretically transferred to a nitrocellulose membrane (Bio-Rad). After blocking with Tris-buffered saline containing 4% bovine serum albumin and 0.1% Tween 20 at room temperature, membranes were incubated with specific primary antibody overnight at 4 °C and, subsequently, with appropriate horseradish peroxidase-conjugated secondary antibody for 1 h. Immunolabeled proteins were finally visualized by chemiluminescence using the LAS-3000 analyzer (Fujifilm). Image processing was performed using Multi Gauge software (Fujifilm).
Statistical Analysis
Results are presented as means ± S.D. They were statistically analyzed with student’s t test. p < 0.05 was considered statistically significant.
References
Ifegwu, O. C. & Anyakora, C. Polycyclic Aromatic Hydrocarbons: Part I. Exposure. Adv. Clin. Chem 72, 277–304, doi:10.1016/bs.acc.2015.08.001 (2015).
Skupińska, K., Misiewicz, I. & Kasprzycka-Guttman, T. Polycyclic aromatic hydrocarbons: physicochemical properties, environmental appearance and impact on living organisms. Acta Pol. Pharm. 61, 233–240 (2004).
Clark, J. D. et al. Exposure to polycyclic aromatic hydrocarbons and serum inflammatory markers of cardiovascular disease. Environ. Res. 117, 132–137, doi:10.1016/j.envres.2012.04.012 (2012).
Karimi, P., Peters, K. O., Bidad, K. & Strickland, P. T. Polycyclic aromatic hydrocarbons and childhood asthma. Eur. J. Epidemiol. 30, 91–101, doi:10.1007/s10654-015-9988-6 (2015).
Yan, J., Wang, L., Fu, P. P. & Yu, H. Photomutagenicity of 16 polycyclic aromatic hydrocarbons from the US EPA priority pollutant list. Mutat. Res. 557, 99–108, doi:10.1016/j.mrgentox.2003.10.004 (2004).
N’Diaye, M. et al. Aryl hydrocarbon receptor- and calcium-dependent induction of the chemokine CCL1 by the environmental contaminant benzo[a]pyrene. J. Biol. Chem. 281, 19906–19915, doi:10.1074/jbc.M601192200 (2006).
Mayati, A., Le Ferrec, E., Lagadic-Gossmann, D. & Fardel, O. Aryl hydrocarbon receptor-independent up-regulation of intracellular calcium concentration by environmental polycyclic aromatic hydrocarbons in human endothelial HMEC-1 cells. Environ. Toxicol. 27, 556–562, doi:10.1002/tox.v27.9 (2012).
Ovrevik, J. et al. Differential effects of nitro-PAHs and amino-PAHs on cytokine and chemokine responses in human bronchial epithelial BEAS-2B cells. Toxicol. Appl. Pharmacol. 242, 270–280, doi:10.1016/j.taap.2009.10.017 (2010).
Øvrevik, J., Refsnes, M., Holme, J. A., Schwarze, P. E. & Låg, M. Mechanisms of chemokine responses by polycyclic aromatic hydrocarbons in bronchial epithelial cells: sensitization through toll-like receptor-3 priming. Toxicol. Lett. 219, 125–132, doi:10.1016/j.toxlet.2013.02.014 (2013).
Mayati, A. et al. Induction of intracellular calcium concentration by environmental benzo(a)pyrene involves a β2-adrenergic receptor/adenylyl cyclase/Epac-1/inositol 1,4,5-trisphosphate pathway in endothelial cells. J. Biol. Chem. 287, 4041–4052, doi:10.1074/jbc.M111.319970 (2012).
Mayati, A. et al. Calcium signaling and β2-adrenergic receptors regulate 1-nitropyrene induced CXCL8 responses in BEAS-2B cells. Toxicol. Vitro Int. J. Publ. Assoc. BIBRA 28, 1153–1157, doi:10.1016/j.tiv.2014.05.012 (2014).
Najafi, A., Sequeira, V., Kuster, D. W. D. & van der Velden, J. β-adrenergic receptor signalling and its functional consequences in the diseased heart. Eur. J. Clin. Invest. 46, 362–374, doi:10.1111/eci.2016.46.issue-4 (2016).
Taira, C. A. et al. Therapeutic implications of beta-adrenergic receptor pharmacodynamic properties. Curr. Clin. Pharmacol 3, 174–184, doi:10.2174/157488408785747719 (2008).
Parnell, E., Smith, B. O. & Yarwood, S. J. The cAMP sensors, EPAC1 and EPAC2, display distinct subcellular distributions despite sharing a common nuclear pore localisation signal. Cell. Signal. 27, 989–996, doi:10.1016/j.cellsig.2015.02.009 (2015).
Danner, S., Frank, M. & Lohse, M. J. Agonist regulation of human beta2-adrenergic receptor mRNA stability occurs via a specific AU-rich element. J. Biol. Chem. 273, 3223–3229, doi:10.1074/jbc.273.6.3223 (1998).
Factor, P. et al. Polycyclic aromatic hydrocarbons impair function of β2-adrenergic receptors in airway epithelial and smooth muscle cells. Am. J. Respir. Cell Mol. Biol. 45, 1045–1049, doi:10.1165/rcmb.2010-0499OC (2011).
Canga, L., Levi, R. & Rifkind, A. B. Heart as a target organ in 2,3,7,8-tetrachlorodibenzo-p-dioxin toxicity: decreased beta-adrenergic responsiveness and evidence of increased intracellular calcium. Proc. Natl. Acad. Sci. USA 85, 905–909, doi:10.1073/pnas.85.3.905 (1988).
Myers, S. A., Eriksson, N., Burow, R., Wang, S.-C. M. & Muscat, G. E. O. Beta-adrenergic signaling regulates NR4A nuclear receptor and metabolic gene expression in multiple tissues. Mol. Cell. Endocrinol. 309, 101–108, doi:10.1016/j.mce.2009.05.006 (2009).
Pearen, M. A. et al. The orphan nuclear receptor, NOR-1, is a target of beta-adrenergic signaling in skeletal muscle. Endocrinology 147, 5217–5227, doi:10.1210/en.2006-0447 (2006).
Kawasaki, H. et al. A family of cAMP-binding proteins that directly activate Rap1. Science 282, 2275–2279, doi:10.1126/science.282.5397.2275 (1998).
de Rooij, J. et al. Epac is a Rap1 guanine-nucleotide-exchange factor directly activated by cyclic AMP. Nature 396, 474–477, doi:10.1038/24884 (1998).
Taylor, S. S., Zhang, P., Steichen, J. M., Keshwani, M. M. & Kornev, A. P. PKA: lessons learned after twenty years. Biochim. Biophys. Acta 1834, 1271–1278, doi:10.1016/j.bbapap.2013.03.007 (2013).
Ferguson, S. S. et al. Role of beta-arrestin in mediating agonist-promoted G protein-coupled receptor internalization. Science 271, 363–366, doi:10.1126/science.271.5247.363 (1996).
January, B. et al. beta2-adrenergic receptor desensitization, internalization, and phosphorylation in response to full and partial agonists. J. Biol. Chem. 272, 23871–23879, doi:10.1074/jbc.272.38.23871 (1997).
Collins, S., Bouvier, M., Bolanowski, M. A., Caron, M. G. & Lefkowitz, R. J. cAMP stimulates transcription of the beta 2-adrenergic receptor gene in response to short-term agonist exposure. Proc. Natl. Acad. Sci. USA 86, 4853–4857, doi:10.1073/pnas.86.13.4853 (1989).
Collins, S. et al. Mechanisms involved in adrenergic receptor desensitization. Biochem. Soc. Trans. 18, 541–544, doi:10.1042/bst0180541 (1990).
Chu, S. et al. Prenatal and postnatal polycyclic aromatic hydrocarbon exposure, airway hyperreactivity, and Beta-2 adrenergic receptor function in sensitized mouse offspring. J. Toxicol. 2013, 603581, doi:10.1155/2013/603581 (2013).
Neal, M. S., Zhu, J. & Foster, W. G. Quantification of benzo[a]pyrene and other PAHs in the serum and follicular fluid of smokers versus non-smokers. Reprod. Toxicol. Elmsford N 25, 100–106, doi:10.1016/j.reprotox.2007.10.012 (2008).
Wang, W., Li, X. & Xu, J. Exposure to cigarette smoke downregulates β2-adrenergic receptor expression and upregulates inflammation in alveolar macrophages. Inhal. Toxicol. 27, 488–494, doi:10.3109/08958378.2015.1075628 (2015).
Gagnon, A. W., Kallal, L. & Benovic, J. L. Role of clathrin-mediated endocytosis in agonist-induced down-regulation of the beta2-adrenergic receptor. J. Biol. Chem 273, 6976–6981, doi:10.1074/jbc.273.12.6976 (1998).
Hadcock, J. R. & Malbon, C. C. Down-regulation of beta-adrenergic receptors: agonist-induced reduction in receptor mRNA levels. Proc. Natl. Acad. Sci. USA 85, 5021–5025, doi:10.1073/pnas.85.14.5021 (1988).
Pende, A. et al. Regulation of the mRNA-binding protein AUF1 by activation of the beta-adrenergic receptor signal transduction pathway. J. Biol. Chem. 271, 8493–8501, doi:10.1074/jbc.271.14.8493 (1996).
Bouvier, M. et al. Two distinct pathways for cAMP-mediated down-regulation of the beta 2-adrenergic receptor. Phosphorylation of the receptor and regulation of its mRNA level. J. Biol. Chem. 264, 16786–16792 (1989).
Fan, G., Shumay, E., Malbon, C. C. & Wang, H. c-Src tyrosine kinase binds the beta 2-adrenergic receptor via phospho-Tyr-350, phosphorylates G-protein-linked receptor kinase 2, and mediates agonist-induced receptor desensitization. J. Biol. Chem. 276, 13240–13247, doi:10.1074/jbc.M011578200 (2001).
Ahn, S., Maudsley, S., Luttrell, L. M., Lefkowitz, R. J. & Daaka, Y. Src-mediated tyrosine phosphorylation of dynamin is required for beta2-adrenergic receptor internalization and mitogen-activated protein kinase signaling. J. Biol. Chem. 274, 1185–1188, doi:10.1074/jbc.274.3.1185 (1999).
Shukla, A. K., Xiao, K. & Lefkowitz, R. J. Emerging paradigms of β-arrestin-dependent seven transmembrane receptor signaling. Trends Biochem. Sci. 36, 457–469, doi:10.1016/j.tibs.2011.06.003 (2011).
Bourquard, T. et al. Unraveling the molecular architecture of a G protein-coupled receptor/β-arrestin/Erk module complex. Sci. Rep. 5, 10760, doi:10.1038/srep10760 (2015).
Tomkiewicz, C. et al. The aryl hydrocarbon receptor regulates focal adhesion sites through a non-genomic FAK/Src pathway. Oncogene 32, 1811–1820, doi:10.1038/onc.2012.197 (2013).
Vogel, C. F. A. et al. Dioxin increases C/EBPbeta transcription by activating cAMP/protein kinase A. J. Biol. Chem. 279, 8886–8894, doi:10.1074/jbc.M310190200 (2004).
Oesch-Bartlomowicz, B. & Oesch, F. Role of cAMP in mediating AHR signaling. Biochem. Pharmacol. 77, 627–641, doi:10.1016/j.bcp.2008.10.017 (2009).
Monteiro, P. et al. Dioxin-mediated up-regulation of aryl hydrocarbon receptor target genes is dependent on the calcium/calmodulin/CaMKIalpha pathway. Mol. Pharmacol. 73, 769–777, doi:10.1124/mol.107.043125 (2008).
Oakley, R. H., Revollo, J. & Cidlowski, J. A. Glucocorticoids regulate arrestin gene expression and redirect the signaling profile of G protein-coupled receptors. Proc. Natl. Acad. Sci. USA 109, 17591–17596, doi:10.1073/pnas.1209411109 (2012).
Schmidt, P., Holsboer, F. & Spengler, D. Beta(2)-adrenergic receptors potentiate glucocorticoid receptor transactivation via G protein beta gamma-subunits and the phosphoinositide 3-kinase pathway. Mol. Endocrinol. Baltim. Md 15, 553–564, doi:10.1210/mend.15.4.0613 (2001).
Paolillo, S. et al. Role of alveolar β2-adrenergic receptors on lung fluid clearance and exercise ventilation in healthy humans. PloS One 8, e61877, doi:10.1371/journal.pone.0061877 (2013).
Snyder, E. M., Johnson, B. D. & Joyner, M. J. Genetics of beta2-adrenergic receptors and the cardiopulmonary response to exercise. Exerc. Sport Sci. Rev. 36, 98–105, doi:10.1097/JES.0b013e318168f276 (2008).
Yin, Q. et al. Downregulation of β-Adrenoceptors in Isoproterenol-Induced Cardiac Remodeling through HuR. PloS One 11, e0152005, doi:10.1371/journal.pone.0152005 (2016).
Croen, L. A. et al. Prenatal exposure to β2-adrenergic receptor agonists and risk of autism spectrum disorders. J. Neurodev. Disord. 3, 307–315, doi:10.1007/s11689-011-9093-4 (2011).
Pitzer, M., Schmidt, M. H., Esser, G. & Laucht, M. Child development after maternal tocolysis with beta-sympathomimetic drugs. Child Psychiatry Hum. Dev. 31, 165–182, doi:10.1023/A:1026419720410 (2001).
Witter, F. R., Zimmerman, A. W., Reichmann, J. P. & Connors, S. L. In utero beta 2 adrenergic agonist exposure and adverse neurophysiologic and behavioral outcomes. Am. J. Obstet. Gynecol. 201, 553–559, doi:10.1016/j.ajog.2009.07.010 (2009).
Sparfel, L. et al. Transcriptional signature of human macrophages exposed to the environmental contaminant benzo(a)pyrene. Toxicol. Sci. Off. J. Soc. Toxicol. 114, 247–259, doi:10.1093/toxsci/kfq007 (2010).
Chen, C.-Y. A., Ezzeddine, N. & Shyu, A.-B. Messenger RNA half-life measurements in mammalian cells. Methods Enzymol. 448, 335–357, doi:10.1016/S0076-6879(08)02617-7 (2008).
Lecureur, V. et al. ERK-dependent induction of TNFalpha expression by the environmental contaminant benzo(a)pyrene in primary human macrophages. FEBS Lett. 579, 1904–1910, doi:10.1016/j.febslet.2005.01.081 (2005).
Acknowledgements
We wish to thank the MRic facilities (SFR Biosit) for microscopy experiments and the Ligue Contre le Cancer (Comité 35) for financial support to our work.
Author information
Authors and Affiliations
Contributions
E.L.F., A.M., O.F., and M.R. conceived the study and designed the experiments; E.L.F., A.M., N.P. and M.R., performed the experiments; E.L.F., A.M., M.R., N.P., D.L.G., O.F. and L.S. analyzed the data; E.L.F. and A.M., wrote the manuscript in close collaboration with all other authors. All authors reviewed the manuscript. All authors finally approved this version to be published.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mayati, A., Podechard, N., Rineau, M. et al. Benzo(a)pyrene triggers desensitization of β2-adrenergic pathway. Sci Rep 7, 3262 (2017). https://doi.org/10.1038/s41598-017-03646-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-03646-4
This article is cited by
-
Benzo[a]pyrene disrupts LH/hCG-dependent mouse Leydig cell steroidogenesis through receptor/Gαs protein targeting
Scientific Reports (2024)
-
Potential role of polycyclic aromatic hydrocarbons in air pollution-induced non-malignant respiratory diseases
Respiratory Research (2020)
-
Potential role of polycyclic aromatic hydrocarbons as mediators of cardiovascular effects from combustion particles
Environmental Health (2019)
-
Combustion Particle-Induced Changes in Calcium Homeostasis: A Contributing Factor to Vascular Disease?
Cardiovascular Toxicology (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.