Abstract
The cardiovascular protective role of furin has been suggested by some animal-based studies but has not been well studied in humans. Therefore, the objective of this study was to examine the prospective association between serum furin and high blood pressure in a longitudinal cohort of Chinese adults. Leveraging a longitudinal prospective cohort with blood pressure examined twice on average 4 years apart, we systemically examined the cross-sectional, longitudinal, and prospective associations of baseline serum furin with blood pressure and incident hypertension. Conventional risk factors, including age, sex, education level, cigarette smoking, alcohol consumption, BMI, fasting glucose, and lipids, were controlled. All participants included were free of cardiovascular and kidney disease at baseline. The cross-sectional analysis of 2312 participants (mean age 53 years) revealed that individuals with the lowest quartile of serum furin had average systolic, diastolic, and mean arterial blood pressures that were 2.58, 1.38, and 1.61 mmHg higher, respectively, than the corresponding pressures in individuals with the highest quartile (all P < 0.001). These negative associations remained significant after controlling for the dynamic risk profiles during follow-up in the longitudinal analysis. The prospective analysis of 1088 participants free of prevalent hypertension at baseline revealed that compared with participants with the highest quartile of serum furin, those with the lowest quartile had a 46% increased risk of incident hypertension (HR = 1.46, P = 0.003). These results indicate that lower serum furin is significantly associated with higher blood pressure and predicts an increased future risk of developing hypertension in Chinese adults. Furin may be a protective factor or marker of hypertension.
Similar content being viewed by others
Introduction
Hypertension is a polygenetic, complicated disease affecting two-thirds of the population worldwide [1]. As a leading modifiable risk factor for cardiovascular disease (CVD) [2], a better understanding of the mechanisms and risk factors of hypertension is of critical importance for the prevention and management of this debilitating disorder and CVD. Furin, a member of the subtilisin-like proprotein convertase enzyme family, plays a pivotal role in diverse physiological processes, such as proliferation and migration of vascular smooth muscle cells [3], vascular remodeling [4], maintenance of sodium-electrolyte balance [5] and activation of the prorenin receptor [6], all of which are involved in blood pressure maintenance. These findings may indicate a potential role for human furin in hypertension. Some recent findings also support this hypothesis. For example, animal studies found that haptic overexpression of profurin, a precursor of furin, can reverse atherosclerosis in mice [4]. Genetic variants of the FURIN gene have been associated with blood pressure [7,8,9], hypertension [10], coronary artery disease [11,12,13], and stroke [14] in humans. Furin is expressed in a broad range of organs and tissues related to hypertension, such as the heart, arteries, nervous system, kidney, and blood [15]. It also enters the circulation and can be measured as a potential biomarker for diseases. A recent study found that the extracellular furin concentration remains consistent with its intracellular level [16]. To date, circulating furin has been limitedly studied in humans and was previously associated with diabetes [17] and diabetic CVD [18]. Further, the existing studies were mainly conducted in populations with European ancestry that have different cardiovascular risk profiles from that of the Chinese population. To date, no study has examined the association between circulating furin and hypertension in the Chinese population or other ethnic groups. Therefore, we aimed to examine the prospective association between serum furin and hypertension in a systemic manner, leveraging a longitudinal cohort of Chinese adults in the Gusu cohort.
Methods
Study participants
The Gusu cohort is a community-based longitudinal prospective cohort study of CVD and its risk factors in middle-aged and elderly Chinese adults in eight communities residing in a traditional but economically developed district of Suzhou, China. The study design, survey methods, and laboratory techniques have been described previously [19]. In brief, the first clinical examination was conducted in 2010 (Phase I) by enrolling 2706 community members aged over 30 years. All surviving participants were re-examined in 2014 (Phase II) and are currently being followed through 2020. The protocols of the current study were approved by the Soochow University Ethics Committee. Written informed consent was obtained from all study participants.
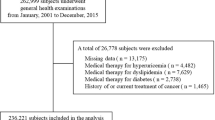
Figure 1 describes the selection of study participants included in the current analysis. Of 2706 individuals participating in the Phase I examination, 394 participants were excluded due to missing data on serum furin at baseline. A subsequent total of 2312 participants with complete data on serum furin and blood pressure measurements were included in the analysis of the cross-sectional association between serum furin and blood pressure. After further excluding 300 participants who refused to participate in the Phase II examination, 2012 participants were included in the analysis of the longitudinal association between serum furin and dynamic blood pressure during follow-up. Of these, 1088 participants free of hypertension at the Phase I examination were included in the analysis of the prospective association between baseline serum furin and incident hypertension. All participants in the Gusu cohort had not been diagnosed with CVD or chronic kidney disease in the Phase I examination.
Measurement of serum furin
Furin was measured in the stored serum samples drawn at the Phase I examination only. Serum furin measurements were performed in the Jiangsu Key Laboratory of Preventive and Translational Medicine for Geriatric Diseases at Soochow University. The staff who performed the measurements were blinded to the clinical characteristics of the study participants. We used a sandwich enzyme immunoassay (Catalog: DL-FUR-Hu; DLDEVELOP, Wuxi, China) to quantify concentrations of human furin in serums frozen at −80 °C until laboratory testing. All samples were processed in a duplicate assay. A standard curve was constructed, from which furin concentrations of unknown samples were determined. Intra- and inter-assay coefficients of variation were less than 10 and 12%, respectively.
Measurement of blood pressure and the definition of incident hypertension
In both examinations, blood pressure was measured three times by trained staff using a standard mercury sphygmomanometer and a cuff of appropriate size according to a standard protocol [20], after the participants had been resting for at least 5 min in a relaxed, sitting position. The first and fifth Korotkoff sounds were recorded as the systolic blood pressure (SBP) and diastolic blood pressure (DBP), respectively. The mean of the three measurements was used in statistical analyses. Mean arterial pressure (MAP) was approximately estimated using a formula in which the DBP is doubled and added to the SBP and that composite sum then is divided by 3. According to the Chinese guidelines for the management of hypertension, hypertension was defined as SBP ≥ 140 mmHg and/or DBP ≥ 90 mmHg or use of antihypertensive medications in the last 2 weeks [21]. Incident hypertension was defined as participants who were free of hypertension in the Phase I examination but initiated antihypertensive medications during follow-up or had an SBP of at least 140 mmHg or a DBP of at least 90 mmHg at the Phase II examination.
Assessment of conventional risk factors
Demographic data, including age, sex, and education level estimated as years of under education, were obtained by questionnaires administered by trained staff in the Phase 1 examination. Lifestyles and metabolic factors were measured at both baseline and follow-up examinations. In both examinations, cigarette smoking was classified as current smoking or not. Current smoking was defined as having smoked at least 100 cigarettes in the entire lifetime, having smoked cigarettes regularly, and smoking currently. Alcohol consumption was classified as current drinkers or not. Current drinkers were those who had consumed any alcohol during the past year. Body weight (kg) and height (cm) were measured by trained staff with the participants wearing light clothes and no shoes. BMI was calculated by dividing weight in kilograms by the square of height in meters (kg/m2). Fasting glucose, blood lipids including total cholesterol, triglycerides, high-density lipoprotein cholesterol (HDL-C), and low-density lipoprotein cholesterol (LDL-C) were measured by standard laboratory methods [19].
Statistical analysis
To carefully examine the association between serum furin and hypertension in a systemic manner, we tested the cross-sectional, longitudinal, and prospective associations of serum furin with blood pressure and incident hypertension, respectively. Log-transformation (base 10) was applied to maximize the normality of serum furin (log10-furin). A two-tailed P value of less than 0.05 was considered statistically significant. All statistical analyses were conducted using SAS statistical software (version 9.4; Cary, North Carolina, USA).
Cross-sectional association analysis
To examine whether serum furin was associated with SBP, we constructed a robust linear regression model in which SBP was the dependent variable and serum furin (log10-furin as a continuous variable or categorical furin levels in quartiles) was the independent variable, adjusting for potential confounders including age, sex, education level, current smoking, current drinking, BMI, LDL-C, HDL-C, fasting glucose, and under antihypertensive treatments (y/n). The robust regression model was used here to account for the influence of extreme values of serum furin and other covariables on model fitting. The associations of serum furin with other blood pressure components, such as DBP and MAP, were similarly examined.
Longitudinal association analysis
To further examine whether dynamic risk profiles during follow-up influence the association between serum furin and dynamic blood pressure, we constructed a linear mixed effects model in which repeated measurements of SBP were the dependent variable, serum furin (log10-furin as a continuous variable or categorical furin levels in quartiles) at baseline was the independent variable, adjusting for sex, education level, and repeated measurements of age, current smoking, current drinking, BMI, LDL-C, HDL-C, fasting glucose, and under antihypertensive treatments (y/n) at baseline and follow-up examinations, with two time-points of examinations as the random effect. The linear mixed regression model was used here to account for repeated measurements and reduce the effects of dynamic risk profiles on follow-up blood pressure. The longitudinal associations of serum furin with dynamic DBP and MAP were similarly examined.
Prospective association analysis
To examine whether baseline serum furin could predict future risk of incident hypertension, we constructed a Cox proportional hazards model in which time (in days) to incident hypertension was the dependent variable and serum furin at baseline (log_furin as a continuous variable or categorical furin levels in quartiles) was the independent variable, adjusting for baseline conventional risk factors, including age, sex, education level, current smoking, current drinking, BMI, LDL-C, HDL-C, and fasting glucose. Participants who had already been diagnosed with hypertension at baseline were excluded from this model. For incident hypertensive cases who initiated antihypertensive medications during follow-up, the initiating date was used in the Cox model. For those who were not under antihypertensive medications, we used the clinical examination date on which a new case of incident hypertension was identified as the date of diagnosis. For participants who remained free of hypertension by the end of follow-up, the time to events was censored at the end of follow-up.
Secondary analysis
To further examine whether serum furin could improve the prediction performance over conventional risk factors, such as age, sex, current smoking, current drinking, BMI, LDL-C, HDL-C, and fasting glucose, we calculated and compared the area under the receiver operating characteristic (ROC) curves for two prediction models (conventional risk factors only vs. conventional risk factors plus serum furin) using logistic regression.
Results
Baseline characteristics of study participants
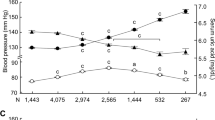
The current study included 2312 middle-aged and elderly Chinese adults (mean age 53 ± 10 years, 62% women). Of them, 1060 (45.85%) participants were diagnosed with having prevalent hypertension, including 642 individuals receiving antihypertensive medications. The baseline characteristics of the study participants according to quartiles of serum furin are shown in Table 1. Each blood pressure component, including SBP, DBP, and MAP, was significantly decreased as serum furin increased (all P < 0.001). Participants with a lower level of serum furin were more likely to be older, male, current smokers, current drinkers, under antihypertensive medications, and having a higher level of fasting glucose than those with a higher level of serum furin (all P < 0.05). No significant difference in other listed variables across quartiles of serum furin.
Cross-sectional association between serum furin and blood pressure
Table 2 shows the cross-sectional associations of serum furin with SBP, DBP, and MAP in the Phase I examination, after adjusting for age, sex, education level, current smoking, current drinking, BMI, LDL-C, HDL-C, fasting glucose, and antihypertensive treatment. Regression using log10-furin as a continuous variable showed that each 10-fold lower serum furin level was significantly associated with a 3.17 mmHg higher SBP, a 1.68 mmHg higher DBP, and a 2.03 mmHg higher MAP, respectively (all P < 0.001). The results of regression based on quartiles of serum furin also detected significant associations in the same direction. Compared with participants at the highest quartile of serum furin, those at the lowest quartile had an average of 2.58 mmHg higher SBP (P = 0.001), 1.38 mmHg higher DBP (P = 0.004), and 1.61 mmHg higher MAP (P = 0.002), respectively.
Longitudinal association between baseline serum furin and dynamic blood pressure during follow-up
Of the 2312 participants included in the cross-sectional analysis in the Phase I examination, 2012 individuals participated in the Phase II examination conducted an average of 4 years later. During follow-up, some conventional risk factors of hypertension, such as blood glucose and lipids, as expected, were dynamically changed (Supplementary Table 1). Table 3 presents the longitudinal associations of baseline serum furin with dynamic SBP, DBP, and MAP during follow-up after controlling for the dynamic risk profiles. Regression using log_furin as a continuous variable showed that the negative associations of serum furin with SBP (β = −2.12, P = 0.004), DBP (β = −0.62, P = 0.034), and MAP (β = −1.12, P = 0.020) persisted after adjusting for dynamic risk profiles including age, cigarette smoking, alcohol consumption, antihypertensive treatment, BMI, glucose, and lipids during follow-up. Regression based on quartiles of serum furin found similar results. Compared with participants with the highest level of serum furin at baseline, those with the lowest level of serum furin had an average 1.75 mmHg higher SBP (P = 0.012), 0.84 mmHg higher DBP (P = 0.037) and 0.93 mmHg higher MAP (P = 0.042).
Prospective association between baseline serum furin and incident hypertension
Of the 1088 participants free of hypertension at baseline and repeatedly participating in both examinations, 160 participants developed new hypertension during an average 4 years of follow-up. The prospective association of baseline serum furin with the risk of incident hypertension is illustrated in Fig. 2. Each 10-fold lower serum furin level at baseline was significantly associated with a 36% higher risk of developing hypertension approximately 4 years later, independent of conventional risk factors of hypertension (HR = 1.36, P < 0.001). Compared with participants with the highest level of serum furin, those with the lowest level of serum furin had a 46% increased risk of incident hypertension (HR = 1.46, P = 0.003).
Results of secondary analysis
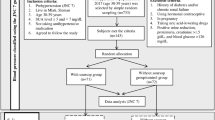
Figure 3 presents the comparisons in the ROC curves for two prediction models: conventional risk factors only and conventional risk factors plus serum furin. Adding serum furin to the prediction model slightly increased the prediction performance for hypertension compared with that of the model including conventional risk factors only, but the improvement did not reach statistical significance (area under ROC curve: 0.723 vs. 0.711, P = 0.167 for comparison).
The comparison of the ROC curves for two prediction models: conventional risk factors only vs. conventional risk factors plus serum furin. The area under the ROC curve for the prediction model of conventional risk factors only was 0.711 (95% CI: 0.669–0.752, red line). After adding serum furin, the area under the ROC curve for the prediction model became 0.723 (95% CI: 0.683–0.762, green line). The P-value for the comparison of the ROC curves for the two prediction models was 0.167
Discussion
In a longitudinal prospective cohort of middle-aged and elderly Chinese adults in the Gusu cohort, our study for the first time systemically examined the cross-sectional, longitudinal, and prospective associations between serum furin and high blood pressure. The results showed that a lower level of serum furin at baseline was not only significantly associated with higher blood pressure (SBP, DBP, MAP) but also significantly predicted a higher risk of incident hypertension during an average 4 years of follow-up. These identified associations were independent of conventional risk factors of hypertension, including smoking, drinking, obesity, blood glucose, and lipids. These results may suggest that a lower level of furin in the circulation could serve as a predictor and risk factor for the development and progression of hypertension.
In line with our study, the identified association between serum furin and high blood pressure has also been suggested by some previous studies. For example, an animal study found that mice with haptic overexpression of profurin, a precursor of furin, exhibited reduced atherosclerosis and vascular remodeling, which is the fundamental pathogenesis of hypertension [4]. In humans, the Young Finns Study, a genome-wide association study (GWAS), found that the genotype AA of rs4702 in the FURIN gene, which marked decreased furin expression, was associated with both elevated SBP and DBP [7]. The associations between FURIN gene polymorphisms and blood pressure have also been demonstrated in other GWASs, mainly in European ancestry populations [9]. In addition to hypertension per se, the FURIN gene has also been suggested as a candidate gene involved in vascular complications of hypertension, e.g., coronary artery disease [11,12,13] and stroke [14] in humans. Although no evidence to date demonstrates the association between the FURIN gene genotype and blood pressure or hypertension in the Chinese Han population, our study demonstrated a similar association between lower circulating furin and a higher risk of hypertension in this population to the genetic findings in other ethnic groups in the same direction. To the best of our knowledge, only two studies have examined furin levels in the circulation linking to disease states. One study including 4678 European adults found that baseline plasma furin predicted future risk of diabetes [17]. The other study found a significantly increased level of plasma furin in 25 diabetic patients complicated with CVD compared with that in 25 patients with diabetes alone [22]. Although the underlying reasons are unclear, these findings that conflict with ours and prior genetic studies [7, 9] suggest a complicated role of furin in the development and progression of hypertension and related conditions. Our study provided the first population evidence for the potential role of furin in the pathogenesis of hypertension and increased the possibility that furin deficiency might be a risk factor for hypertension and related cardiovascular disorders.
Although we found that serum furin could predict future risk of hypertension independently of conventional risk factors, including age, sex, education level, cigarette smoking, alcohol consumption, obesity, lipids, and glucose, serum furin just slightly (but not significantly) improved the prediction performance for hypertension over these conventional risk factors. Whether furin deserves to be an interventional target for the prevention and management of hypertension remains to be studied.
To deepen our understanding of the role of furin in the cardiovascular system, the mechanisms underlying the identified association between serum furin and hypertension needs discussion. Furin, a member of the subtilisin-like proprotein convertase enzyme, can convert many inactive protein precursors into their active forms. Of these proteins, some play vasoconstrictive roles, and others play vasodilative roles in the maintenance of blood pressure. For example, renin receptor (RR), activated by furin from its precursor [6, 23], binds renin or prorenin and consequently enhances renin activity and fully activates the biologically inactive prorenin peptide involved in the pathogenesis and progression of hypertension [24]. Overexpression of another protein activated by furin, epithelial Na + channel (ENaC) [5], has also been associated with high blood pressure. In stark contrast, transforming growth factor (TGF-β) [25, 26] is also activated by furin but contributes to lower blood pressure [27]. Another protein B-type natriuretic peptide (BNP) activated by furin [28, 29] has been associated with low blood pressure through its natriuretic/diuretic and vasodilatory actions. These inconsistent results indicate a complicated role of furin in the complex phenotype of hypertension. Despite the conflicting findings, these studies together with ours suggest an association between furin and hypertension. In addition, there may be some unknown biological activities beyond the vessel constrictive mechanisms of furin that are involved in the cardiovascular system.
To the best of our knowledge, our study is the first to examine the prospective association of serum furin with incident hypertension in Chinese adults. The strengths of this study include a longitudinal prospective study design, careful and systemic analyses of the association between serum furin and high blood pressure, and comprehensive adjustments of many conventional risk factors. However, our study also has several limitations. First, the restricted sample size may not allow us to identify a statistically significant association with a small effect size. However, we successfully found a significant prospective association between serum furin and hypertension in a small sample of 1088 adults free of prevalent hypertension at baseline. Furthermore, in a larger sample, the cross-sectional and longitudinal associations between serum furin and blood pressure persisted in the same direction as the prospective association. Such robust results indicate a biologically true association between furin and hypertension. Second, as an observational study, we cannot entirely exclude residual confounding. Although we identified a significant prospective association between baseline serum furin and future risk of hypertension, the causality between furin deficiency and hypertension is not established and requires further evidence from clinical trials. Third, we only included Chinese middle-aged and elderly adults in our study. Thus, the generalizability of our findings to other populations with different genetic backgrounds and health profiles or younger populations is questioned. Fourth, the most important use of a biomarker is its indication of the timing from the physiological to pathologic state. We only obtained blood pressure at the 4-year follow-up examination and consequently could only foresee an individual’s risk of hypertension 4 years later based on our current results. To what extent serum furin at baseline could predict a pathologic high blood pressure is unknown. Fifth, some considerable confounding factors, such as salt intake and renal function, were not obtained in our study. It is therefore uncertain whether the association between serum furin and hypertension is independent of these factors.
In summary, our study demonstrates that a lower level of serum furin was not only significantly associated with a higher SBP, DBP, and MAP but also predicted an increased risk of future hypertension in Chinese adults. These findings indicate that the circulating level of furin could serve as a predictor for the identification of individuals at high risk for hypertension during primary prevention. Furin may be a protective factor or a drug target for the prevention and management of hypertension, but more evidence is needed to establish the causality between furin level and hypertension.
References
Sarki AM, Nduka CU, Stranges S, Kandala NB, Uthman OA. Prevalence of hypertension in low and middle-income countries: a systematic review and meta-analysis. Medicine 2015;94:e1959.
Fleisher LA, Fleischmann KE, Auerbach AD, Barnason SA, Beckman JA, Bozkurt B, et al. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery. Anesth Analg 2014;58:15–26.
Urban D, Lorenz J, Meyborg H, Ghosh S, Kintscher U, Kaufmann J, et al. Proprotein convertase furin enhances survival and migration of vascular smooth muscle cells via processing of pro-nerve growth factor. J Biochem. 2013;153:197.
Lei X, Basu D, Li Z, Zhang M, Rudic RD, Jiang XC, et al. Hepatic overexpression of the prodomain of furin lessens progression of atherosclerosis and reduces vascular remodeling in response to injury. Atherosclerosis 2014;236:121–30.
Hughey RP, Bruns JB, Kinlough CL, Harkleroad KL, Tong Q, Carattino MD, et al. Epithelial sodium channels are activated by furin-dependent proteolysis. J Biol Chem. 2004;279:18111–4.
Cousin C, Bracquart D, Contrepas A, Corvol P, Muller L, Nguyen G. Soluble form of the (pro)renin receptor generated by intracellular cleavage by furin is secreted in plasma. Hypertension. 2009;53:1077–82.
Turpeinen H, Seppälä I, Lyytikäinen LP, Raitoharju E, Hutri-Kähönen N, Levula M, et al. A genome-wide expression quantitative trait loci analysis of proprotein convertase subtilisin/kexin enzymes identifies a novel regulatory gene variant for FURIN expression and blood pressure. Hum Genet 2015;134:627–36.
Wain LV, Vaez A, Jansen R, Joehanes R, Pj VDM, Erzurumluoglu AM, et al. Novel blood pressure locus and gene discovery using genome-wide association study and expression data sets from blood and the kidney. Hypertension. 2017;9:117.09438.
Ehret GB, Munroe PB, Rice KM, Bochud M, Johnson AD, Chasman DI, et al. Genetic variants in novel pathways influence blood pressure and cardiovascular disease risk. Nature 2011;478:103–9.
Li N, Luo W, Zhang J, Jin Y, Wang H, Ling Z, et al. Associations between genetic variations in the FURIN gene and hypertension. BMC Med Genet. 2010;11:124.
Deloukas P, Kanoni S, Willenborg C, Farrall M, Assimes TL, Thompson JR, et al. Large-scale association analysis identifies new risk loci for coronary artery disease. Nat Genet. 2013;45:25–33.
van der Harst P, Verweij N. Identification of 64 novel genetic loci provides an expanded view on the genetic architecture of coronary artery disease. Circ Res. 2018;122:433–43.
Nikpay M, Goel A, Won HH, Hall LM, Willenborg C, Kanoni S, et al. A comprehensive 1000 genomes-based genome-wide association meta-analysis of coronary artery disease. Nat Genet. 2015;47:1121–30.
Sun QX, Zhou HM, Du QW. Association of Rs2071410 on furin with transient ischemic attack susceptibility and prognosis in a Chinese population. Med Sci Monit Int Med J Exp Clin Res. 2016;22:3828.
Nakayama K. Furin: a mammalian subtilisin/Kex2p-like endoprotease involved in processing of a wide variety of precursor proteins. Biochem J 1997;327(Pt 3):625–35.
Ventura E, Weller M, Burghardt I. Cutting edge: ERK1 mediates the autocrine positive feedback loop of TGF-beta and furin in glioma-initiating cells. J Immunol. 2017;198:4569–74.
Fernandez C, Rysa J, Almgren P, Nilsson J, Engstrom G, Orho-Melander M, et al. Plasma levels of the proprotein convertase furin and incidence of diabetes and mortality. J Intern Med. 2018;284:377–87.
Fathy SA, Hamid FFA, Zabut BM, Jamee AF, Ali MAM, Mustafa AMA. Diagnostic utility of BNP, corin and furin as biomarkers for cardiovascular complications in type 2 diabetes mellitus patients. Biomark: Biochem Indic Expo, response, susceptibility Chem 2015;20:460–9.
Peng H, Zhang Q, Cai X, Liu Y, Ding J, Tian H, et al. Association between high serum soluble corin and hypertension: a cross-sectional study in a general population of China. Am J Hypertens 2015;28:1141–9.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr., et al. The seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. J Am Med Assoc. 2003;289:2560–72.
Liu LS. 2010 Chinese guidelines for the management of hypertension]. Zhonghua Xin Xue Guan Bing Za Zhi 2011;39:579–615.
Fathy SA, Abdel Hamid FF, Zabut BM, Jamee AF, Ali MA, Abu Mustafa AM. Diagnostic utility of BNP, corin and furin as biomarkers for cardiovascular complications in type 2 diabetes mellitus patients. Biomarkers 2015;20:460–9.
Nguyen G, Danser AH. Prorenin and (pro)renin receptor: a review of available data from in vitro studies and experimental models in rodents. Exp Physiol. 2008;93:557–63.
Gonzalez AA, Prieto MC. Renin and the (pro)renin receptor in the renal collecting duct: role in the pathogenesis of hypertension. Clin Exp Pharmacol Physiol 2015;42:14–21.
Badri KR, Yue M, Carretero OA, Aramgam SL, Cao J, Sharkady S, et al. Blood pressure homeostasis is maintained by a P311–TGF-β axis. J Clin Invest. 2013;123:4502–12.
Dubois CM, Blanchette F, Laprise MH, Leduc R, Grondin F, Seidah NG. Evidence that furin is an authentic transforming growth factor-beta1-converting enzyme. Am J Pathol 2001;158:305–16.
Li Y, Shen XZ, Li L, Zhao TV, Bernstein KE, Johnson AK, et al. Brain transforming growth factor-beta resists hypertension via regulating microglial activation. Stroke. 2017;48:2557–64.
Semenov AG, Tamm NN, Seferian KR, Postnikov AB, Karpova NS, Serebryanaya DV, et al. Processing of pro-B-type natriuretic peptide: furin and corin as candidate convertases.%A Semenov AG. Clin Chem. 2010;56:1166–76.
Nishikimi T, Nakagawa Y, Minamino N, Ikeda M, Tabei K, Fujishima A. et al. Pro-B-type natriuretic peptide is cleaved intracellularly: impact of distance between O-glycosylation and cleavage sites. Am J Physiol Regul, Integr Comp Physiol. 2015;309:R639–49.
Acknowledgements
We are deeply appreciative of the participants in this study and thank all staff members for their support and assistance. In particular, we thank the Center for Disease Prevention and Control of Gusu District for their support in the recruitment of participants.
Funding
This study was supported by the Special Financial Grant from the China Postdoctoral Science Foundation (No. 2015T80584), the General Financial Grant from the China Postdoctoral Science Foundation (No. 2014M551661), the National Natural Science Foundation of China (No. 81202271 and 81872690), the Natural Science Foundation of Jiangsu Province (No. BK20180841), the Suzhou Science and Technology Project (No. SS201853, SS0910 and SS201333), and a project of the Priority Academic Program Development of Jiangsu Higher Education Institutions, China. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
He, Y., Ren, L., Zhang, Q. et al. Serum furin as a biomarker of high blood pressure: findings from a longitudinal study in Chinese adults. Hypertens Res 42, 1808–1815 (2019). https://doi.org/10.1038/s41440-019-0295-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-019-0295-6
Keywords
This article is cited by
-
Association between high serum Nogo-B and hypertension in Chinese Han
BMC Cardiovascular Disorders (2022)
-
The association between plasma furin and cardiovascular events after acute myocardial infarction
BMC Cardiovascular Disorders (2021)