Abstract
We have identified a novel function for a member of the transient receptor potential (TRP) protein super-family, TRPM2, in prostate cancer cell proliferation. TRPM2 encodes a non-selective cation-permeable ion channel. We found that selectively knocking down TRPM2 with the small interfering RNA technique inhibited the growth of prostate cancer cells but not of non-cancerous cells. The subcellular localization of this protein is also remarkably different between cancerous and non-cancerous cells. In BPH-1 (benign), TRPM2 protein is homogenously located near the plasma membrane and in the cytoplasm, whereas in the cancerous cells (PC-3 and DU-145), a significant amount of the TRPM2 protein is located in the nuclei in a clustered pattern. Furthermore, we have found that TRPM2 inhibited nuclear ADP-ribosylation in prostate cancer cells. However, TRPM2 knockdown-induced inhibition of proliferation is independent of the activity of poly(ADP-ribose) polymerases. We conclude that TRPM2 is essential for prostate cancer cell proliferation and may be a potential target for the selective treatment of prostate cancer.
Similar content being viewed by others
Introduction
Prostate cancer is the second most prevalent cancer among men over 50 years of age, with nearly 30 000 men dying from the disease each year in the United States. Although many theories have been proposed and investigated, the exact mechanism leading to development and progression of prostate cancer remains unknown. However, recent reports suggest that transient receptor potential (TRPs) ion channel super-families have a significant role in regulating calcium homeostasis during prostate carcinogenesis.1 The function of TRPM2 in cancer cells has recently been investigated.2, 3 Using a cDNA array technique, significantly increased TRPM2 mRNA expression has been observed in prostate cancer tissues and cell lines in comparison with normal prostate tissues (http://www.ncbi.nlm.nih.gov/projects/geo/gds).
TRPM2 is a member of the TRP protein super-family of ion channels4, 5 that can be activated by ADP-ribose,6 β-NAD,7 TNFα,8 or H2O2,9 which results in an increase in intracellular free calcium concentration ([Ca2+]i).10 ADP-ribose is a breakdown product of NAD+, CD38, cADP-ribose, and protein de-acetylation.4, 11 As a bifunctional protein, TRPM2 protein contains a Nudix box in its C-terminus,12 which is a common motif of enzymes that degrade nucleotide diphosphates in addition to serving as a binding site for ADP-ribose.13 This study is designed to closely evaluate the role of TRPM2 in cell proliferation of prostate cancer cells.
Materials and methods
Prostate cancer tissue sections
Small blocks of fresh prostate cancer tissue were obtained during radial prostatectomy of prostate cancer patients (mean age of 61 and Gleason score range of 6–8) at Tulane Hospital and Clinics and the VA Hospital in New Orleans, LA, USA (consent was approved by institution review board for such studies). Tissues were snap-frozen in liquid nitrogen after being carefully embedded in Tissue-Tek OCT Compound (Jed Pella Inc., Redding, CA, USA). Samples were microtomed into 6–7 μm thick sections, mounted onto clean uncoated glass slides, and stored at −80 °C until further processing.
Laser capture microdissection and RNA preparation
The sections were thawed at room temperature for 10 s, followed by normal hemotoxylin and eosin staining, air dried, and subjected to laser capture microdissection (LCM) using a PixCell II instrument and CapSure LCM Caps (Arcturus Engineering, Mountain View, CA, USA). Matched tumor cells and benign prostate epithelium from LCM procured prostate from the same patient were captured separately after identification, confirmation, staging, and grading of the tissue area by a certified pathologist. Laser captured cells from multiple serial sections (roughly 2000–3000 pulses at spot diameter of 30 μm and 25–35 mW laser power) were pooled into a 500 μl nuclease-free Eppendorf tube containing 400 μl of TRI Reagent (Molecular Research Centre Inc., Cincinnati, OH, USA) mixed with RNA carrier, 1 μl of 10 μg μl−1 of GenEluteTM Linear PolyAcrylamide (Sigma, St Louis, MO, USA). After recovery of the RNA pellet, a DNase treatment step was performed for 2 h at 37 °C using 2 unit of RQ1 RNase-free Dnase (Promega Corp., Madison, WI, USA), followed by re-extraction and precipitation. The RNA yield and integrity was determined using Agilent 2100 bioanalyzer (Agilent Technologies, Palo Alto, CA, USA) with RNA LabChip (Ambion Inc., Austin, TX, USA). Only RNA samples with distinguished bands of 28S and 18S and without multiple RNA degradation bands were subjected to further analysis.
Cell culture
The human prostate epithelial cell line BPH-1 was a gift from Dr Stuart W Hayward and Dr R Dahia of the University of San Francisco. Other prostate cell lines, including RWPE-1, PC-3, DU-145, and LNCaP were purchased from ATCC (Manassas, VA, USA). For comparison purposes, human cavernosal smooth muscle cells routinely grown as primary culture in our laboratory and maintained in DMEM media containing 10% heat inactivated fetal bovine serum were used as controls for these studies. BPH-1, PC-3, DU-145, and LNCaP cells were grown in RPMI-1640 medium containing 5% fetal bovine serum. Normal epithelial RWPE-1 cells were grown in kerationcyte-SFM medium containing 5 ng ml−1 epidermal growth factor and 50 μg ml−1 bovine pituitary extract (Invitrogen Corp., Carlsbad, CA, USA). All cells were cultured in a humidified incubator with 5% CO2 and 95% air at 37 °C.
Cell proliferation analysis
Proliferation was assessed using a WST-8 assay according to manufacturer's instructions. Briefly, 10 μl of 2-(2-methoxy-4-nitrophenyl)-3-(4-nitrophenyl)-5-(2,4-disul-phonyl)-2H-etrazolium (WST-8) was added to each well at the end of treatment and incubated for one additional hour. Optical density values were read by an ELISA plate reader at wavelengths of 450 and 650 nm. Results were calculated as percentage of control. For the PARP activity experiment, PC-3 cells were seeded in a 96-well plate at a density of approximately 103 cells per well, in triplicate. The following day, the cells were treated with the PARP inhibitor NU1025 at concentrations ranging from 0.2 to 2 mM for 24 and 72 h.
Quantitative real-time PCR and RT–PCR
For quantitative real-time PCR, the primers of TRPM2 were forward: 5′-CCATCCGTGACCTTCTCATT-3′ and reverse: 5′-CTCTGAGCCCAGATGATTCC-3′ (reverse). The primers of β-actin used for real-time PCR were forward: 5′-GGCACCCAGCACAATGAAG-3′ and reverse: 5′-GCCGATCCACACGGAGTACT 3′ (reverse). SYBR Green PCR master mix (Applied Biosystems, Warrington, UK) was used to develop the real-time PCR in a thermal cycler (GeneAmp 5700, Applied Biosystems). A validation experiment was carried out to check whether the efficiencies of all target and reference primers were approximately equal.
For RT–PCR, RNA was extracted from prostate epithelial cell lines and cancer cell lines using TRI-REAGENT (Molecular Research Center Inc.). A 2 μg sample of total RNA from each cell line was incubated with 1 unit of RNase-free DNase for 10 min at 37 °C and then at 65 °C for another 10 min. Random primers (1 μg) were then added and the tube was kept at 70 °C for 5 min. Subsequently, 5 μl of Moloney murine leukemia virus reverse transcriptase reaction buffer (5 × ), 1 μl of 10 mM PCR nucleotide mix, 25 units of rRNasin ribonuclease inhibitor, and 200 units of Moloney murine leukemia virus reverse transcriptase were added to the tube and incubated at 37 °C for 1 h. All reagents were purchased from Promega Co. The cDNA product (2 μl) was mixed with 1.5 units TaKaRa Taq, 2.5 μl 10 × PCR buffer, 2 μl 2.5 mM dNTP mixture (TaKaRa Shuzo Co., Otsu, Japan), and 100 pM of each primer, with DEPC water added for a final volume of 25 μl. The primers for TRPM2 were forward: 5′-ATGCTACCTCGGAAGCTGAA-3′ and reverse: 5′-TTCTGGAGGAGGGTCTTGTG-3′; for TRPC3—forward: 5′-CAAGTACCCTCCAACCCTCA-3′ and reverse: 5′-CTGGCTGCTAGATCCCAGAA-3′; for TRPV5—forward: 5′-CGCTGTTGTGAACCAGAATG-3′ and reverse: 5′-GCTGGAGGATGAGgatgtgt-3′; for GAPDH—forward: 5′-TCAACGGATTTGGTCGTATTGGG-3′ and reverse: 5′-TGATTTTGGAGGGATCTCGC-3′. The amplification protocol for PCR was set as follows: 94 °C for 4 min, followed by 30 cycles of amplification steps (94 °C for 2 min, 60 °C for 30 s, 72 °C for 40 s), and the final extension at 72 °C for 8 min. PCR products were analyzed using agarose gel (1.5%) electrophoresis and visualized under UV light after staining with ethidium bromide (1 μg ml−1).
Western blot analysis
For nuclear protein extraction, nuclei were isolated from both prostate cancer cell lines (PC-3 and DU-145) and non-cancerous cell lines (BPH and RWPE-1) using CelLytic NucLEAR Extraction kit (Sigma-Aldrich Inc.). The nuclei were lysed and extracted by centrifugation at 13 000 g for 5 min. The supernatant was collected and protein concentrations were determined using BCA reagent (PIERCE Chemical Co., Rockford, IL, USA). For western blot analysis, an equal amount of protein (50 μg) from each cell extract was separated in SDS–PAGE gels (Bio-Rad Laboratories, Hercules, CA, USA). The proteins were transferred electrophoretically to a 0.2 μm nitrocellulose membrane. Non-fat dry milk (5%) in PBS containing 0.1% Tween 20 (PBS-T) was used as a blocking agent for 1 h at room temperature. The membrane was then treated with 1:300 dilution of TRPM2 primary antibody (Bethyl Laboratories Inc., Montgomery, TX, USA) at 4 °C overnight, rinsed briefly with PBS-T twice, and incubated with HRP-conjugated secondary antibody (dilution 1:2000 in PBS-T) for 1 h at room temperature with constant agitation. The film was developed with the ECL western blot detection reagent kit (Amersham Pharmacia Biotech, Piscataway, NJ, USA).
Immunofluorescent confocal microscopy
Cells were placed on chamber slides for 1 day to allow for attachment. Cells were then subsequently washed three times with PBS, fixed with methanol at −20 °C for 10 min, and permeabilized in 0.5% Triton X-100 in PBS for 5 min. After treatment with 20% goat serum for 10 min, cells were incubated with primary antibody (rabbit anti-TRPM2, 1:50, Bethyl Laboratories Inc.) for 60 min at room temperature, which was followed by secondary antibody (goat anti-rabbit IgG FITC conjugated, 1:200, Bethyl Laboratories Inc.) for 30 min in darkness. Propidium iodide (Abcam Inc., Cambridge, MA, USA) was used for nuclear staining. Confocal microscopy was performed using a Leica TCS SP2 confocal microscope equipped with five lasers, including Argon 488 nm and HeNe 543 nm (Leica Microsystems, Exton, PA, USA).
Small interfering RNA assay
Cells were cultured on 96-well microplates until ∼30% confluence and then transfected with 40 nM of either small interfering RNA (siRNA) specific to TRPM2 (5′-AUAGAUCAGGAACUCCGUCUC-3′) or scrambled siRNA (Integrated DNA Technology, Coralville, IA, USA) using Lipofectamine 2000 transfection reagent (Invitrogen) according to the manufacturer's instructions. Cell growth was monitored by a WST-8 cell counting kit (Alexis Biochemicals Corp., San Diego, CA, USA).
Statistical analysis
All data are expressed as mean±standard deviation. For statistical analysis, Student's t-test was used to compare the differences between control and treatment groups. A probability value of P<0.05 is considered statistically significant and denoted by asterisk marks in the figures.
Results
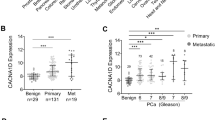
TRPM2 mRNA expression in cancerous vs benign tissue
The expression of TRPM2 mRNA was examined using real-time PCR in cells isolated by laser capture microdissection from tumor tissues isolated from prostate cancer patients as compared with that from cells of the benign tissues of the same subjects. Our qRT–PCR analysis demonstrated selective high expression of TRPM2 transcripts in 75% of LCM-procured malignant cells in comparison to matched microdissected benign cells of surgical specimens (Table 1). It is noteworthy that TRPM2 expression does not correlate with age or Gleason score. However, our results further emphasize the need to confirm these observations in a large cohort of prostate cancer patients.
TRPM2 mRNA expression in prostate cancer cell lines
RT–PCR analysis was performed to evaluate TRPM2 mRNA expression in prostate cancer cell lines (DU-145, LNCaP, and PC-3). As shown in Figure 1, all three types of cells yielded a clear PCR product band (293 bp) of TRPM2. These data suggest that these cell lines are appropriate models for studying the mechanism of TRPM2 underlying cancer progression.
Subcellular expression of TRPM2 in prostate cells
We examined the sub-cellular distribution of TRPM2 in prostate cancer and non-cancerous prostate cell lines using immunofluorescent confocal microscopy. As shown in Figure 2a, TRPM2 proteins are located at the plasma membrane and cytoplasm in BPH-1 cells. However, in the prostate cancer cell lines (PC-3 and DU-145), TRPM2 is also highly expressed in the nuclear region in a clustered pattern. The expression of TRPM2 in RWPE-1 cells is very low in our experiment. To confirm the predominant expression of TRPM2 in the nuclei of prostate cancer cells, nuclear proteins from PC-3 and DU-145 cells were extracted and analyzed using western blot analysis. Equal amounts of protein extracts (50 μg) from the different cell lines were used for western blot analysis. As shown in Figure 2b, expression of TRPM2 protein was detected in the nuclei of prostate cancer cells (PC-3 and DU-145). In contrast, TRPM2 was absent in the nuclei of benign (BPH-1) or normal prostate epithelium cells (RWPE-1). These data confirm that TRPM2 is expressed in the nuclei of prostate cancer cells. Our western blot analysis also detected TRPM2 expression in the cytoplasm preparations in PC-3, DU-145, and BPH-1 cells, but not in RWPE-1 cells. This is consistent with the data in Figure 2a.
(a) Confocal microscopy showing the subcellular expression of TPRM2 protein in prostate cancer cell Lines (PC-3, DU-145), benign cells (BPH-1), and normal prostate epithelial cell line (RWPE-1). DU-145 is the 15th section of the z-series images (30 series). PC-3, BPH-1, and RWPE-1 are the 10th section of the z-series images (30 series). Red is propidium iodide (PI) label of nuclei and green is FITC fluorescence conjugated secondary antibody against TRPM2 antibody. Single arrows indicate the nuclear location of TRPM2 in cancer cells. Double arrow indicates plasma membrane expression of TRPM2 in BPH-1 cells. All images are the overlays of FITC and PI fluorescence. (b) Expression of TPRM2 proteins in both the nuclei and the remainders (whole cell preparation excluding nuclei) of prostate cancer cell lines (PC-3 and DU-145) and non-cancerous prostate epithelium cell lines (BPH and RWPE-1).
Involvement of TRPM2 in prostate cancer cell proliferation
To examine the role of TRPM2 in prostate cancer cell proliferation, we conducted experiments to selectively block the expression of TRPM2 mRNA by transfecting siRNA specifically targeting TRPM2 (siRNA-TRPM2) into prostate cancer cells and non-cancerous prostate cells and examining the effect of the siRNA on the proliferation of these cells. As shown in Figure 3a, a significant inhibitory effect on prostate cancer cell proliferation was observed in siRNA-TRPM2-treated cells as compared with control cells that were not transfected with siRNA or cells treated with scrambled siRNA (P<0.05). In contrast, siRNA-TRPM2 had no inhibitory effect on RWPE-1 or BPH-1 cell proliferation. These data suggest that knockdown of TRPM2 does not inhibit cell growth in non-cancerous prostate epithelial cells, but specifically inhibits growth of prostate cancer cells.
Selective inhibitory effect of siRNA-TRPM2 on prostate cancer cell proliferation. (a) Cell proliferation monitored in cell lines PC-3, DU-145, BPH-1, and RWPE-1 with WST-8 assay. The open square represents the data from untreated cells (control). The open triangle represents data from cells treated with 40 nM scrambled siRNA. The open circle represents the data from cells treated with 40 nM siRNA-TRPM2. N=3 for all groups. Error bar represents the standard deviation. *Indicates P<0.05 between siRNA-TRPM2 treatment and the two other groups. (b) RT–PCR showed that TRPM2 mRNA expression is inhibited by the siRNA-TRPM2 treatment in DU-145 and PC-3 2 days after the siRNA transfection. The sizes of PCR products are 293 bp and 234 bp for TRPM2 and GAPDH, respectively. (c) Western blot shows that TRPM2 protein expression is inhibited in PC-3 by 40 nM siRNA-TRPM2 treatment for 72 h. Repeated three times. siTRPM2: siRNA-TRPM2.
The efficiency of the siRNA-TRPM2 in suppressing TRPM2 expression was examined with the RT–PCR method. Figure 3b shows that siRNA-TRPM2 successfully blocked the expression of TRPM2 mRNA in both PC-3 and DU-145 cells. The expression of TRPM2 protein was also inhibited by siRNA-TRPM2 treatment, as shown in Figure 3c. Western blot analysis shows the expression of TRPM2 protein was significantly reduced in PC-3 cells treated with siRNA-TRPM2 when compared with scrambled siRNA treatments. Pretreating the primary antibody with a specific blocking peptide completely prevented binding of the antibody to the TRPM2 protein.
Effect of knockdown of TRPM2 on ADP-ribosylation in prostate cancer cells
On the basis of the finding that TRPM2 is relocated in the nucleus of prostate cancer cells and the fact that TRPM2 has ADP-ribose pyrophosphatase activity,6, 12 we hypothesized that TRPM2 may decrease the level of poly ADP-ribose in the nucleus of cancer cells by catalyzing ADP-ribose to ribose 5-phosphate and AMP.14 To test this hypothesis, we transfected (Lipofectamine, Invitrogen) siRNA-TRPM2 (40 nM) into PC-3 and BPH-1 cells for 72 h to knock down the expression of TRPM2 specifically. We then measured level of ADP-ribosylation in the cells with fluorescent microscopy and ELISA.
As shown in Figure 4a, control PC-3 cells and PC-3 cells treated with scrambled siRNA presented low levels of ADP-ribosylation, as indicated by only a few cells being stained with the red fluorescent dye (anti-ADP-ribose conjugated with Texas Red). Conversely, substantial increases in the occurrence and intensity of red fluorescence in stained PC-3 cells were observed in siRNA-TRPM2-treated cells, suggesting that an increase in ADP-ribosylation occurred even though the total number of living cells was reduced significantly under this condition. In Figure 4a, total cell number was less after the treatment with siRNA-TRPM2 than the control or scrambled siRNA; this is consistent with the experimental result shown in Figure 3a.
Effect of siRNA-TRPM2 on ADP-ribosylation in PC-3 cells. (a) Immunofluorescence indicating ADP-ribosylation in PC-3 cells transfected with no siRNA (control), scrambled siRNA, or siRNA-TRPM2. The magnification for all of the images is × 10. (b) ELISA measurement of ADP-ribosylation in PC-3 and BPH-1 cells. *Indicates P<0.01 of Student's t-test between the siRNA-TRPM2 treated and the control groups. (c) Dose-dependent toxic effect of UN1025 on PC-3 cells. (d) PC-3 cell proliferation of under the conditions of 40 nM siRNA-TRPM2 treatment and co-treatment with siRNA-TRPM2 and 100 μM UN1025. #Indicates P<0.05 of Student's t-test between the siRNA-TRPM2 or UN1025+siRNA-TRPM2 treated and the control groups.
An ELISA assay was used to evaluate the level of ADP-ribosylation in PC-3 and BPH-1 cells (Figure 4b). In general, the ADP-ribosylation was higher in PC-3 cells than that in BPH-1 cells. After treatment with siRNA-TRPM2 for 72 h, an approximately threefold increase in the ADP-ribosylation was measured in PC-3 cells, whereas no observable difference was seen in BPH-1 cells. These data are consistent with our previous observation that showed specific TRPM2 protein expression in the nuclei of prostate cancer cells and no such expression in the nuclei of BPH-1 cells.
PARP-independent inhibition of ADP-ribosylation by TRPM2 in prostate cancer cells
Poly ADP-ribosylation is a transient posttranslational modification of nuclear proteins, mainly catalyzed by poly ADP-ribose polymerases (PARPs). ADP-ribose in the nucleus is converted into poly ADP-ribose by PARPs, a process that has an important function in DNA repair15 and cell replication.16 Poly ADP-ribosylation also has a role in G0–G1 transition during cell cycle progression.17 Over-activation of PARP can cause cell necrosis because of the depletion of cytoplasmic ATP.18, 19 To examine the potential role of PARPs in TRPM2-mediated proliferation of prostate cancer cells, we used the PARP-1 inhibitor NU1025 (8-hydroxy-2-methylquinazoline-4-(3H)one) to inhibit the activity of the major subtype of PARPs, PARP-1,20 in cells treated with siRNA-TRPM2. Dose-dependent toxicity of NU1025 on PC-3 cell proliferation starts at 200 μM (Figure 4c). PC-3 cells were seeded in a 96-well plate at ∼1000 cells per well in triplicate. Then, cells were treated with 100 μM of NU1025 together with siRNA-TRPM2 or scrambled siRNA for 4 days. NU1025 treatment did not affect cell proliferation when it was applied alone; NU1025 co-treatment did not rescue TRPM2-siRNA-mediated inhibition of cell proliferation (Figure 4d). These results suggest that TRPM2 knockdown-induced inhibition of proliferation is independent of the activity of poly(ADP-ribose) polymerases.
Discussion
Previous studies have shown that TRPM2 channels are expressed primarily in the plasma membrane and have a key role in oxidative stress-induced cell death.12 Our results show a unique and previously unreported role for the TRPM2 protein, facilitating or promoting cell proliferation in cancer cells. The observation of a Ca2+ channel plays a non-Ca2+ transport function is surprising, but not completely new. It has been reported that an L-type voltage-gated Ca2+ channel is proteolytically cleaved to form a C-terminal fragment, which is translocated into the nucleus and alters the endogenous transcription of a wide variety of genes.21 However, the molecular mechanisms that mediate this change in functionality in the TRPM2 protein between cancerous and non-cancerous tissues remain elusive. The difference in the subcellular locations of TRPM2 between cancerous and non-cancerous prostate cells may explain the switching of these two roles. In non-cancerous cells, TRPM2 proteins are mainly located at the plasma membrane where they mediate sodium and calcium influx on oxidative stimulation. As a result, these cation influxes may lead to membrane depolarization and changes in calcium homeostasis that can lead to programed cell death. In cancer cells, the role of TRPM2 as a plasma membrane ion channel is less important because of the internalization and nuclear localization of TRPM2. Abundant TRPM2 proteins are translocated into the nucleus (Figure 2) where they may have an important enzymatic function relating to cancer cell proliferation. We anticipate this TRPM2 nuclear translocation is a more general phenomenon as we also have observed it in other types of cancer cells (data not shown).
It has been reported that two fragments (sense and antisense transcriptions) of TRPM2 are specifically expressed in cancer cells,3 as our PCR and antibody targeted the C-terminus (exons 30–32, exon 25, respectively) it will be very interesting to see if the nuclear expressed TRPM2 represent or include the TRPM2 fragment of the sense transcription. If so, the cancer-specific transcription will create two functionally important fragment proteins—the antisense fragments inhibit the normal Ca2+ transport function of TRPM2 and the sense fragment conducts enzymatic function in the nucleus simultaneously.
Zhang et al.22 have suggested that TRPM2 activation resulted in PARP cleavage and inactivation in hematopoietic cells through a mechanism involving [Ca2+]i elevation. Our data show that knocking down TRPM2 increased PARP activity in prostate cancer cells through a unresolved mechanism and also that direct blockade of PARP-1 activity by NU1025 did not prevent siRNA-TRPM2-induced inhibition of prostate cancer cell proliferation (Figure 4d). These data suggest the activity of PARP-1 may not have a crucial role in siRNA-TRPM2-induced inhibition of cancer cell growth. Therefore, TRPM2 may have an important function in cell proliferation independent of the activity of PARPs in prostate cancer cells.
Dual localization in the plasma membrane and endoplasmic reticulum has been observed for TRPM8 ion channel in prostate cancer cells. TRPM8 is closely related to TRPM2, with 42% homology.23 TRPM8 is highly expressed in endoplasmic reticulum membrane as an ion channel in prostate cancer cells and has an essential role in prostate cancer cell survival.24, 25 However, nuclear expression of this channel has not been seen in prostate cancer cells as we have observed for TRPM2. Whether TRPM2 also functions as an endoplasmic reticulum calcium channel in prostate cancer cells is currently unknown. Our data strongly suggest that TRPM2 has a major function in the nuclei of prostate cancer cells.
Intracellular [Ca2+] regulation has a crucial role in tumorigenesis, including cell replication and apoptosis.26 Nuclear expression of TRPM2 may also influence nuclear Ca2+ concentration [Ca2+]n. The nuclear envelope comprises an inner membrane that abuts the nucleoplasm and an outer membrane that is continuous with the endoplasmic reticulum. Anchored within this envelope are the nuclear pore complexes and several intracellular calcium store-regulating molecules that have been reported to have a role in the regulation of [Ca2+]n. For example, inositol 1,4,5-trisphosphate (IP3) and inositol 1,3,4,5-tetrakisphosphate (IP4) binding sites have been identified in the inner membrane of the nuclear envelope.27, 28, 29 IP3 and IP4 serve as signal molecules for either Ca2+ release (IP3) or sequestration (IP4) in the nucleus.30 Another example is, cADP-ribose, an endogenous regulator of type 2 ryanodine receptors that induces Ca2+ release from nuclear stores.31 More detailed information concerning the nuclear location of TRPM2 will be useful in advancing our knowledge of this aspect of prostate cancer proliferation.
The mechanism of TRPM2 transmigration into the nucleus is currently unknown. TRPM2 itself does not contain a nuclear localization signaling sequence; therefore, a chaperone may be involved in TRPM2 transportation. A similar mechanism could also be present for TRPM2 considering evidence that inositol 1,4,5-trisphosphate receptors (IP3R) can migrate into the nucleus and IP3R directly binds to TRPC channels.32, 33
TRPM2 is expressed in many non-cancerous cells, such as brain and peripheral blood cells.7, 8, 34 Considering the function of TRPM2 in these cells is to serve as a mediator of oxidative-stress-induced calcium influx (i.e., the channel is at plasma membrane) and thus apoptosis in those tissues, inhibition of TRPM2 may be beneficial in terms of continued survival.35 Selectively suppressing the expression of TRPM2 or blocking the transmigration of these proteins into the nucleus may not harm non-cancerous cells, but may selectively inhibit prostate cancer growth. Therefore, TRPM2 may be a potential target for the selective control of prostate cancer growth and cell proliferation.
References
Pervarskaya N, Flourakis M, Bidaux G, Thebault S, Skryma R . Differential role of TRP channels in prostate cancer. Biochem Soc Trans 2007; 35: 133–135.
Ishii M, Oyama A, Hagiwara T, Miyazaki A, Mori Y, Kiuchi Y et al. Facilitation of H2O2-induced A172 human glioblastoma cell death by insertion of oxidative stress-sensitive TRPM2 channels. Anticancer Res 2007; 27: 3987–3992.
Orfanelli U, Wenke A-K, Doglioni C, Russo V, Bosserhoff AK, Lavorgna G . Identification of novel sense and antisense transcription at the TRPM2 locus in cancer. Cell Res 2008; 18: 1128–1140.
Clapham DE . TRP channels as cellular sensors. Nature 2003; 426: 517–524.
Perraud AL, Schmitz C, Scharenberg AM . TRPM2 Ca2+ permeable cation channels: from gene to biological function. Cell Calcium 2003; 33: 519–531.
Perraud AL, Fleig A, Dunn CA, Bagley LA, Launay P, Schmitz C et al. ADP-ribose gating of the calcium-permeable LTRPC2 channel revealed by Nudix motif homology. Nature 2001; 411: 595–599.
Sano Y, Inamura K, Miyake A, Mochizuki S, Yokoi H, Matsushime H et al. Immunocyte Ca2+ influx system mediated by LTRPC2. Science 2001; 293: 1327–1330.
Hara Y, Wakamori M, Ishii M, Maeno E, Nishida M, Yoshida T et al. LTRPC2 Ca2+-permeable channel activated by changes in redox status confers susceptibility to cell death. Mol Cell 2002; 9: 163–173.
Wehage E, Eisfeld J, Heiner I, Jungling E, Zitt C, Luckhoff A . Activation of the cation channel long transient receptor potential channel 2 (LTRPC2) by hydrogen peroxide. A splice variant reveals a mode of activation independent of ADP-ribose. J Biol Chem 2002; 277: 23150–23156.
Kraft R, Grimm C, Grosse K, Hoffmann A, Sauerbruch S, Kettenmann H et al. Hydrogen peroxide and ADP-ribose induce TRPM2-mediated calcium influx and cation currents in microglia. Am J Physiol 2004; 286: C129–C137.
Rafty LA, Schmidt MT, Perraud AL, Scharenberg AM, Denu JM . Analysis of O-acetyl-ribose as a target for Nudix ADP-ribose hydrolases. J Biol Chem 2002; 277: 47114–47122.
Zhang W, Chu X, Tong Q, Cheung JY, Conrad K, Masker K et al. A novel TRPM2 isoform inhibits calcium influx and susceptibility to cell death. J Biol Chem 2003; 278: 16222–16229.
Bessman MJ, Frick DN, O’Handley SF . The MutT proteins or ‘Nudix’ hydrolases, a family of versatile, widely distributed, ‘housecleaning’ enzymes. J Biol Chem 1996; 271: 25059–25062.
Naziroglu M . New molecular mechanism on the activation of TRPM2 channels by oxidative stress and ADP-ribose. Neurochem Res 2007; 32: 1990–2001.
Shell S, de Murcia G . Poly(ADP-ribose) polymerase-1: what have we learned from the deficient mouse model? Mutat Res 2000; 460: 1–15.
Virag L, Szabo C . The therapeutic potential of poly(ADP-ribose) polymerase inhibitors. Pharmacol Rev 2002; 54: 375–429.
Carbone M, Rossi MN, Cavaldesi M, Notari A, Amati P, Maione R . Poly(ADP-ribosyl)ation is implicated in the G0-G1 transition of resting cells. Oncogene 2008; 27: 6083–6092.
Schreiber V, Hunting D, Trucco C, Gowans B, Grunwald D, de Murcia G et al. A dominant negative mutant of human poly(ADP-ribose) polymerase affect cell recovery, apoptosis and sister chromatid exchange following DNA damage. Proc Natl Acad Sci USA 1995; 92: 4753–4757.
Kleczkowska HE, Althaus FR . The role of poly(ADP-ribosyl)lation in the adaptive response. Mutat Res 1996; 35: 215–221.
Bowman KJ, White A, Golding BT, Griffin RJ, Curtin NJ . Potentiation of anti-cancer agent cytotoxicity by the potent poly(ADP-ribose) polymerase inhibitors NU1025 and NU1064. Br J Cancer 1998; 78: 1269–1277.
Gomez-Ospina N, Tsuruta F, Barreto-Chang O, Hu L, Dolmetsch R . The C-terminus of the L-type voltage-gated calcium channel Ca(V)1.2 encodes a transcription factor. Cell 2006; 127: 591–606.
Zhang W, Hirschler-Laszkiewicz I, Tong Q, Conrad K, Sun S-C, Penn L et al. TRPM2 is an ion channel that modulates hematopoietic cell death through activation of caspases and PARP cleavage. Am J Physiol Cell Physiol 2005; 290: 1146–1159.
Tsavaler L, Shapero MH, Morkowski S, Laus R . Trp-p8, a novel prostate-specific gene, is up-regulated in prostate cancer and other malignancies and shares high homology with transient receptor potential calcium channel proteins. Cancer Res 2001; 61: 3760–3769.
Zhang L, Barritt GJ . Evidence that TRPM8 is an androgen-dependent Ca2+ channel required for the survival of prostate cancer cells. Cancer Res 2004; 64: 8365–8373.
Thebault S, Lemonnier L, Bidaux G, Flourakis M, Bavencoffe A, Gordienko D et al. Novel role of cold/menthol-sensitive transient receptor potential melastatine family member 8 (TRPM8) in the activation of store-operated channels in LNCap Human prostate cancer epithelial cells. J Biol Chem 2005; 280: 39423–39435.
Monteith GR, McAndrew D, Faddy HM, Roberts-Thomson SJ . Calcium and cancer: targeting Ca2+ transport. Nature Rev 2007; 7: 519–530.
Maeda N, Niinobe M, Mikoshiba K . A cerebellar Pukinje cell marker P400 protein is an inositol 1,4,5-trisphosphate (InsP3) receptor protein. Purificaation and characterization of InsP3 receptor complex. EMBO J 1990; 9: 61–67.
Malviya AN, Rogue P, Vincendon G . Sterospecific inositol 1,4,5-[32]trisphosphate binding to isolated rat liver nuclei: evidence for inositol trisphosphate receptor-mediated calcium release form the nucleus. Proc Natl Acad Sci USA 1990; 87: 9270–9274.
Matter N, Ritz MF, Freyermuth S, Rogue P, Malviya AN . Stimulation of nuclear protein kinase C leads to phosphorylation of nuclear inositol 1,4,5 trisphosphate receptor and accelerated calcium releases by inositol 1,4,5-trisphosphate form isolated rat liver nuclei. J Biol Chem 1993; 268: 732–736.
MacDonald JR . Nuclear calcium: transfer to and from the cytosol. Biol Signals Recept 1998; 7: 137–147.
Gerasimenko OK, Gerasimenko JV, Tepikin AV, Petersen OH . ATP-dependent accumulation and inositol trsphosphate- or cyclic ADP-ribose-mediated release of Ca2+ from the nuclear envelope. Cell 1995; 80: 439–444.
Boulay G, Brown DM, Qin N, Jiang M, Dietrich A, Zhu MX et al. Modulation of Ca(2+) entry by polypeptides of the inositol 1,4, 5-trisphosphate receptor (IP3R) that bind transient receptor potential (TRP): evidence for roles of TRP and IP3R in store depletion-activated Ca(2+) entry. Proc Natl Acad Sci USA 1999; 96: 14955–14960.
Zhu MX, Tang J . TRPC channel interactions with calmodulin and IP3 receptors. Novartis Found Symp 2004; 258: 44–58.
Nagamine K, Kudoh J, Minoshima S, Kawasaki K, Asakawa S, Ito F et al. Molecular cloning of a novel putative Ca2+ channel protein (TRPC7) highly expressed in brain. Genomics 1998; 54: 124–131.
Fonfria E, Marshall IC, Benham CD, Boyfield I, Brown JD, Hill K et al. TRPM2 channel opening in response to oxidative stress is dependent on activation of poly(ADP-ribose) polymerase. Br J Pharmacol 2004; 143: 186–192.
Acknowledgements
We thank Dr B Miller (Pennsylvania State University) for constructive comments. Supported by ADA research award (ML) and DOD PA031119 (ABA).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-No Derivative Works 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Zeng, X., Sikka, S., Huang, L. et al. Novel role for the transient receptor potential channel TRPM2 in prostate cancer cell proliferation. Prostate Cancer Prostatic Dis 13, 195–201 (2010). https://doi.org/10.1038/pcan.2009.55
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pcan.2009.55
Keywords
This article is cited by
-
TRPM2-mediated Ca2+ signaling as a potential therapeutic target in cancer treatment: an updated review of its role in survival and proliferation of cancer cells
Cell Communication and Signaling (2023)
-
Calcium signalling pathways in prostate cancer initiation and progression
Nature Reviews Urology (2023)
-
The Role οf Ion Channels in the Development and Progression of Prostate Cancer
Molecular Diagnosis & Therapy (2023)
-
The Janus-faced role of TRPM2-S in retroperitoneal liposarcoma via increasing ROS levels
Cell Communication and Signaling (2022)
-
The human ion channel TRPM2 modulates migration and invasion in neuroblastoma through regulation of integrin expression
Scientific Reports (2022)