Key Points
-
Any type of trauma or disease causing damage to the CNS and/or the peripheral nerves in, and around the pelvic floor can cause anejaculation
-
Penile vibratory stimulation (PVS) constitutes the cheapest and least invasive method of inducing ejaculation
-
In patients in whom PVS fails, electroejaculation has proved almost universally successful
-
Surgical sperm retrieval should be reserved strictly for patients in whom assisted ejaculation fails
-
The method of assisted reproductive technique should be chosen primarily based on the total motile sperm count
-
In selected cases, home insemination by the infertile couple themselves is feasible, by means of PVS and intravaginal self-insemination
Abstract
Normal fertility is dependent on intravaginal delivery of semen through ejaculation. This process is highly dependent on an intact ejaculatory reflex arc, which can be disrupted through any type of trauma or disease causing damage to the CNS and/or peripheral nerves. Neurogenic anejaculation is most commonly associated with spinal cord injury. This aetiology is especially relevant because most men with spinal cord injuries are injured at reproductive age. Assisted ejaculation in the form of penile vibratory stimulation is the first choice for sperm retrieval in such patients because it is noninvasive and inexpensive. In patients in whom vibratory stimulation fails, electroejaculation is almost always successful. When both methods of assisted ejaculation are unsuccessful, sperm retrieval by aspiration from either the vas deferens or the epididymis, or by testicular biopsy or surgery are reasonable options. In such cases the most inexpensive and least invasive methods should be considered first. The obtained semen can be used for intravaginal or intrauterine insemination or in vitro fertilization with or without intracytoplasmic sperm injection.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Fode, M. et al. Male sexual dysfunction and infertility associated with neurological disorders. Asian J. Androl. 14, 61–68 (2012).
O'Connor, P. Incidence and patterns of spinal cord injury in Australia. Accid. Anal. Prev. 34, 405–415 (2002).
Rathore, M. F., Hanif, S., Farooq, F., Ahmad, N. & Mansoor, S. N. Traumatic spinal cord injuries at a tertiary care rehabilitation institute in Pakistan. J. Pak. Med. Assoc. 58, 53–57 (2008).
Kuptniratsaikul, V. Epidemiology of spinal cord injuries: a study in the Spinal Unit, Siriraj Hospital, Thailand, 1997–2000. J. Med. Assoc. Thai. 86, 1116–1121 (2003).
Exner, G. & Meinecke, F. W. Trends in the treatment of patients with spinal cord lesions seen within a period of 20 years in German centers. Spinal Cord 35, 415–419 (1997).
Kafetsoulis, A., Brackett, N. L., Ibrahim, E., Attia, G. R. & Lynne, C. M. Current trends in the treatment of infertility in men with spinal cord injury. Fertil. Steril. 86, 781–789 (2006).
Giuliano, F. & Clement, P. Neuroanatomy and physiology of ejaculation. Annu. Rev. Sex Res. 16, 190–216 (2005).
Coolen, L. M., Allard, J., Truitt, W. A. & McKenna, K. E. Central regulation of ejaculation. Physiol Behav. 83, 203–215 (2004).
Thomas, A. J. Jr. Ejaculatory dysfunction. Fertil. Steril. 39, 445–454 (1983).
Turek, P. J. Male Reproductive Physiology in Campbell Walsh Urology Vol. 1 (eds Wein, A. J., Kavoussi, L. R., Novick, A., Partin, A. & Peters, C.) 591–615 (Elsevier Saunders, 2012).
Bohlen, D., Hugonnet, C. L., Mills, R. D., Weise, E. S. & Schmid, H. P. Five meters of H(2)O: the pressure at the urinary bladder neck during human ejaculation. Prostate 44, 339–341 (2000).
Colpi, G. et al. EAU guidelines on ejaculatory dysfunction. Eur. Urol. 46, 555–558 (2004).
Yavetz, H. et al. Retrograde ejaculation. Hum. Reprod. 9, 381–386 (1994).
Ohl, D. A., Quallich, S. A., Sonksen, J., Brackett, N. L. & Lynne, C. M. Anejaculation and retrograde ejaculation. Urol. Clin. North Am. 35, 211–220 (2008).
Kamischke, A. & Nieschlag, E. Update on medical treatment of ejaculatory disorders. Int. J. Androl. 25, 333–344 (2002).
Gilja, I., Parazajder, J., Radej, M., Cvitkovic, P. & Kovacic, M. Retrograde ejaculation and loss of emission: possibilities of conservative treatment. Eur. Urol. 25, 226–228 (1994).
Crich, J. P. & Jequier, A. M. Infertility in men with retrograde ejaculation: the action of urine on sperm motility, and a simple method for achieving antegrade ejaculation. Fertil. Steril. 30, 572–576 (1978).
Brackett, N. L., Ibrahim, E., Iremashvili, V., Aballa, T. C. & Lynne, C. M. Treatment for ejaculatory dysfunction in men with spinal cord injury: an 18-year single center experience. J. Urol. 183, 2304–2308 (2010).
Decter, R. M. et al. Reproductive understanding, sexual functioning and testosterone levels in men with spina bifida. J. Urol. 157, 1466–1468 (1997).
Frohman, E. M. & Wingerchuk, D. M. Clinical practice. Transverse myelitis. N. Engl. J. Med. 363, 564–572 (2010).
Haensch, C. A. & Jorg, J. Autonomic dysfunction in multiple sclerosis. J. Neurol. 253 (Suppl. 1), I3–I9 (2006).
Weinstein, M. H. & Machleder, H. I. Sexual function after aorto-lliac surgery. Ann. Surg. 181, 787–790 (1975).
Kedia, K. R., Markland, C. & Fraley, E. E. Sexual function after high retroperitoneal lymphadenectomy. Urol. Clin. North Am. 4, 523–528 (1977).
Pearce, S., Steinberg, Z. & Eggener, S. Critical evaluation of modified templates and current trends in retroperitoneal lymph node dissection. Curr. Urol. Rep. 14, 511–517 (2013).
Genuth, S. Insights from the diabetes control and complications trial/epidemiology of diabetes interventions and complications study on the use of intensive glycemic treatment to reduce the risk of complications of type 1 diabetes. Endocr. Pract. 12 (Suppl. 1), 34–41 (2006).
Dunsmuir, W. D. & Holmes, S. A. The aetiology and management of erectile, ejaculatory, and fertility problems in men with diabetes mellitus. Diabet. Med. 13, 700–708 (1996).
Sexton, W. J. & Jarow, J. P. Effect of diabetes mellitus upon male reproductive function. Urology 49, 508–513 (1997).
Brindley, G. S. Reflex ejaculation under vibratory stimulation in paraplegic men. Paraplegia 19, 299–302 (1981).
Brackett, N. L. Semen retrieval by penile vibratory stimulation in men with spinal cord injury. Hum. Reprod. Update 5, 216–222 (1999).
Sonksen, J. & Ohl, D. A. Penile vibratory stimulation and electroejaculation in the treatment of ejaculatory dysfunction. Int. J. Androl. 25, 324–332 (2002).
Sonksen, J., Biering-Sorensen, F. & Kristensen, J. K. Ejaculation induced by penile vibratory stimulation in men with spinal cord injuries. The importance of the vibratory amplitude. Paraplegia 32, 651–660 (1994).
Brackett, N. L. et al. An analysis of 653 trials of penile vibratory stimulation in men with spinal cord injury. J. Urol. 159, 1931–1934 (1998).
Brackett, N. L., Kafetsoulis, A., Ibrahim, E., Aballa, T. C. & Lynne, C. M. Application of 2 vibrators salvages ejaculatory failures to 1 vibrator during penile vibratory stimulation in men with spinal cord injuries. J. Urol. 177, 660–663 (2007).
Kafetsoulis, A. et al. Abdominal electrical stimulation rescues failures to penile vibratory stimulation in men with spinal cord injury: a report of two cases. Urology 68, 204–211 (2006).
Giuliano, F. et al. Vardenafil improves ejaculation success rates and self-confidence in men with erectile dysfunction due to spinal cord injury. Spine (Phila Pa 1976) 33, 709–715 (2008).
Courtois, F. J. et al. Blood pressure changes during sexual stimulation, ejaculation and midodrine treatment in men with spinal cord injury. BJU Int. 101, 331–337 (2008).
Leduc, B. E. et al. Midodrine in patients with spinal cord injury and anejaculation: A double-blind randomized placebo-controlled pilot study. J. Spinal Cord Med. 38, 57–62 (2015).
Sonksen, J. Assisted ejaculation and semen characteristics in spinal cord injured males. Scand. J. Urol. Nephrol. Suppl. 2003, 1–31 (2003).
Wieder, J. A., Brackett, N. L., Lynne, C. M., Green, J. T. & Aballa, T. C. Anesthetic block of the dorsal penile nerve inhibits vibratory-induced ejaculation in men with spinal cord injuries. Urology 55, 915–917 (2000).
Ekland, M. B., Krassioukov, A. V., McBride, K. E. & Elliott, S. L. Incidence of autonomic dysreflexia and silent autonomic dysreflexia in men with spinal cord injury undergoing sperm retrieval: implications for clinical practice. J. Spinal Cord. Med. 31, 33–39 (2008).
Wan, D. & Krassioukov, A. V. Life-threatening outcomes associated with autonomic dysreflexia: a clinical review. J. Spinal Cord. Med. 37, 2–10 (2014).
Elliott, S. & Krassioukov, A. Malignant autonomic dysreflexia in spinal cord injured men. Spinal Cord 44, 386–392 (2006).
Sheel, A. W., Krassioukov, A. V., Inglis, J. T. & Elliott, S. L. Autonomic dysreflexia during sperm retrieval in spinal cord injury: influence of lesion level and sildenafil citrate. J. Appl. Physiol. 99, 53–58 (2005).
Steinberger, R. E., Ohl, D. A., Bennett, C. J., McCabe, M. & Wang, S. C. Nifedipine pretreatment for autonomic dysreflexia during electroejaculation. Urology 36, 228–231 (1990).
Castle, S. M. et al. Safety and efficacy of a new device for inducing ejaculation in men with spinal cord injuries. Spinal Cord 52 (Suppl. 2), S27–S29 (2014).
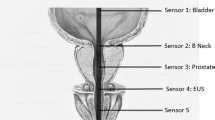
Sonksen, J., Ohl, D. A. & Wedemeyer, G. Sphincteric events during penile vibratory ejaculation and electroejaculation in men with spinal cord injuries. J. Urol. 165, 426–429 (2001).
Suominen, J. J., Kilkku, P. P., Taina, E. J. & Puntala, P. V. Successful treatment of infertility due to retrograde ejaculation by instillation of serum-containing medium into the bladder. A case report. Int. J. Androl. 14, 87–90 (1991).
Perkash, I., Martin, D. E., Warner, H., Blank, M. S. & Collins, D. C. Reproductive biology of paraplegics: results of semen collection, testicular biopsy and serum hormone evaluation. J. Urol. 134, 284–288 (1985).
Sarkarati, M., Rossier, A. B. & Fam, B. A. Experience in vibratory and electro-ejaculation techniques in spinal cord injury patients: a preliminary report. J. Urol. 138, 59–62 (1987).
Braude, P. R., Ross, L. D., Bolton, V. N. & Ockenden, K. Retrograde ejaculation: a systematic approach to non-invasive recovery of spermatozoa from post-ejaculatory urine for artificial insemination. Br. J. Obstet. Gynaecol. 94, 76–83 (1987).
Shangold, G. A., Cantor, B. & Schreiber, J. R. Treatment of infertility due to retrograde ejaculation: a simple, cost-effective method. Fertil. Steril. 54, 175–177 (1990).
Okada, H., Goda, K., Koshida, M. & Kamidono, S. Pregnancy by insemination of cryopreserved spermatozoa from a man with retrograde ejaculation: a case report. J. Reprod. Med. 49, 389–391 (2004).
Hsiao, W., Deveci, S. & Mulhall, J. P. Outcomes of the management of post-chemotherapy retroperitoneal lymph node dissection-associated anejaculation. BJU Int. 110, 1196–1200 (2012).
Kathiresan, A. S. et al. Anejaculatory infertility due to multiple sclerosis. Andrologia 44 (Suppl. 1), 833–835 (2012).
Hultling, C., Levi, R., Amark, S. P. & Sjoblom, P. Semen retrieval and analysis in men with myelomeningocele. Dev. Med. Child Neurol. 42, 681–684 (2000).
Ohl, D. A., Sonksen, J., Menge, A. C., McCabe, M. & Keller, L. M. Electroejaculation versus vibratory stimulation in spinal cord injured men: sperm quality and patient preference. J. Urol. 157, 2147–2149 (1997).
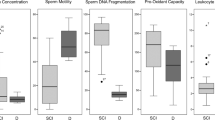
Iremashvili, V. V., Brackett, N. L., Ibrahim, E., Aballa, T. C. & Lynne, C. M. A minority of men with spinal cord injury have normal semen qualitycan we learn from them? A case-control study. Urology 76, 347–351 (2010).
Denil, J., Ohl, D. A., Menge, A. C., Keller, L. M. & McCabe, M. Functional characteristics of sperm obtained by electroejaculation. J. Urol. 147, 69–72 (1992).
Siosteen, A., Forssman, L., Steen, Y., Sullivan, L. & Wickstrom, I. Quality of semen after repeated ejaculation treatment in spinal cord injury men. Paraplegia 28, 96–104 (1990).
Hamid, R., Patki, P., Bywater, H., Shah, P. J. & Craggs, M. D. Effects of repeated ejaculations on semen characteristics following spinal cord injury. Spinal Cord 44, 369–373 (2006).
Das, S. et al. Does repeated electro-ejaculation improve sperm quality in spinal cord injured men? Spinal Cord 44, 753–756 (2006).
Brackett, N. L., Lynne, C. M., Weizman, M. S., Bloch, W. E. & Padron, O. F. Scrotal and oral temperatures are not related to semen quality of serum gonadotropin levels in spinal cord-injured men. J. Androl. 15, 614–619 (1994).
Ohl, D. A. et al. Fertility of spinal cord injured males: effect of genitourinary infection and bladder management on results of electroejaculation. J. Am. Paraplegia Soc. 15, 53–59 (1992).
Brackett, N. L., Lynne, C. M., Weizman, M. S., Bloch, W. E. & Abae, M. Endocrine profiles and semen quality of spinal cord injured men. J. Urol. 151, 114–119 (1994).
Basu, S. et al. Cytofluorographic identification of activated T-cell subpopulations in the semen of men with spinal cord injuries. J. Androl. 23, 551–556 (2002).
Aird, I. A., Vince, G. S., Bates, M. D., Johnson, P. M. & Lewis-Jones, I. D. Leukocytes in semen from men with spinal cord injuries. Fertil. Steril. 72, 97–103 (1999).
Trabulsi, E. J., Shupp-Byrne, D., Sedor, J. & Hirsch, I. H. Leukocyte subtypes in electroejaculates of spinal cord injured men. Arch. Phys. Med. Rehabil. 83, 31–34 (2002).
Basu, S., Aballa, T. C., Ferrell, S. M., Lynne, C. M. & Brackett, N. L. Inflammatory cytokine concentrations are elevated in seminal plasma of men with spinal cord injuries. J. Androl. 25, 250–254 (2004).
Cohen, D. R. et al. Sperm motility in men with spinal cord injuries is enhanced by inactivating cytokines in the seminal plasma. J. Androl. 25, 922–925 (2004).
Brackett, N. L., Cohen, D. R., Ibrahim, E., Aballa, T. C. & Lynne, C. M. Neutralization of cytokine activity at the receptor level improves sperm motility in men with spinal cord injuries. J. Androl. 28, 717–721 (2007).
Ohl, D. A., Menge, A. C. & Jarow, J. P. Seminal vesicle aspiration in spinal cord injured men: insight into poor sperm quality. J. Urol. 162, 2048–2051 (1999).
Brackett, N. L., Davi, R. C., Padron, O. F. & Lynne, C. M. Seminal plasma of spinal cord injured men inhibits sperm motility of normal men. J. Urol. 155, 1632–1635 (1996).
Brackett, N. L., Lynne, C. M., Aballa, T. C. & Ferrell, S. M. Sperm motility from the vas deferens of spinal cord injured men is higher than from the ejaculate. J. Urol. 164, 712–715 (2000).
Qiu, Y., Wang, L. G., Zhang, L. H., Zhang, A. D. & Wang, Z. Y. Quality of sperm obtained by penile vibratory stimulation and percutaneous vasal sperm aspiration in men with spinal cord injury. J. Androl. 33, 1036–1046 (2012).
Iremashvili, V., Brackett, N. L., Ibrahim, E., Aballa, T. C. & Lynne, C. M. The choice of assisted ejaculation method is relevant for the diagnosis of azoospermia in men with spinal cord injuries. Spinal Cord 49, 55–59 (2011).
Bartak, V., Josifko, M. & Horackova, M. Juvenile diabetes and human sperm quality. Int. J. Fertil. 20, 30–32 (1975).
Padron, R. S., Dambay, A., Suarez, R. & Mas, J. Semen analyses in adolescent diabetic patients. Acta Diabetol. Lat. 21, 115–121 (1984).
Ali, S. T., Shaikh, R. N., Siddiqi, N. A. & Siddiqi, P. Q. Semen analysis in insulin-dependent/non-insulin-dependent diabetic men with/without neuropathy. Arch. Androl. 30, 47–54 (1993).
Delfino, M., Imbrogno, N., Elia, J., Capogreco, F. & Mazzilli, F. Prevalence of diabetes mellitus in male partners of infertile couples. Minerva Urol. Nefrol. 59, 131–135 (2007).
Agbaje, I. M. et al. Insulin dependant diabetes mellitus: implications for male reproductive function. Hum. Reprod. 22, 1871–1877 (2007).
Safarinejad, M. R. Evaluation of endocrine profile, hypothalamic-pituitary-testis axis and semen quality in multiple sclerosis. J. Neuroendocrinol. 20, 1368–1375 (2008).
La Vignera. S., Condorelli, R., Vicari, E., D'Agata, R. & Calogero, A. E. Diabetes mellitus and sperm parameters. J. Androl. 33, 145–53 (2012).
Shin, D. H. & Turek, P. J. Sperm retrieval techniques. Nat. Rev. Urol. 10, 723–730 (2013).
Goldstein, M. & Tanrikut, C. Microsurgical management of male infertility. Nat. Clin. Pract. Urol. 3, 381–391 (2006).
Wosnitzer, M. S. & Goldstein, M. Obstructive azoospermia. Urol. Clin. North Am. 41, 83–95 (2014).
Practice Committee of American Society for Reproductive Medicine. Sperm retrieval for obstructive azoospermia. Fertil. Steril. 90, S213–S218 (2008).
Dieckmann, K. P., Heinemann, V., Frey, U. & Pichlmeier, U. How harmful is contralateral testicular biopsy?—an analysis of serial imaging studies and a prospective evaluation of surgical complications. Eur. Urol. 48, 662–672 (2005).
Donoso, P., Tournaye, H. & Devroey, P. Which is the best sperm retrieval technique for non-obstructive azoospermia? A systematic review. Hum. Reprod. Update 13, 539–549 (2007).
Boomsma, C. M., Heineman, M. J., Cohlen, B. J. & Farquhar, C. Semen preparation techniques for intrauterine insemination. Cochrane Database of Systematic Reviews, Issue 4. Art. No.: CD004507. http://dx.doi.org/10.1002/14651858.CD00450.pub2.
Duran, E. H., Morshedi, M., Taylor, S. & Oehninger, S. Sperm DNA quality predicts intrauterine insemination outcome: a prospective cohort study. Hum. Reprod. 17, 3122–3128 (2002).
Cantineau, A. E., Cohlen, B. J. & Heineman, M. J. Ovarian stimulation protocols (anti-oestrogens, gonadotrophins with and without GnRH agonists/antagonists) for intrauterine insemination (IUI) in women with subfertility. Cochrane Database of Systematic Reviews, Issue 2. Art. No.: CD005356. http://dx.doi.org/10.1002/14651858.CD005356.pub2.
Bensdorp, A. J., Cohlen, B. J., Heineman, M. J. & Vandekerckhove, P. Intra-uterine insemination for male subfertility. Cochrane. Database. Syst. Rev. Issue: 4. Art No.: CD000360. http://dx.doi.org/10.1002/14651858.CD000360.pub4.
Goverde, A. J. et al. Ovarian response to standard gonadotrophin stimulation for IVF is decreased not only in older but also in younger women in couples with idiopathic and male subfertility. Hum. Reprod. 20, 1573–1577 (2005).
Yeh, J., Leipzig, S., Friedman, E. A. & Seibel, M. M. Results of in vitro fertilization pregnancies: experience at Boston's Beth Israel Hospital. Int. J. Fertil. 35, 116–119 (1990).
Navot, D., Bergh, P. A. & Laufer, N. Ovarian hyperstimulation syndrome in novel reproductive technologies: prevention and treatment. Fertil. Steril. 58, 249–261 (1992).
[No authors listed]. Assisted reproductive technology in the United States: 1996 results generated from the American Society for Reproductive Medicine/Society for Assisted Reproductive Technology Registry. Fertil. Steril. 71, 798–807 (1999).
Schenker, J. G. & Ezra, Y. Complications of assisted reproductive techniques. Fertil. Steril. 61, 411–422 (1994).
Fauser, B. C., Devroey, P. & Macklon, N. S. Multiple birth resulting from ovarian stimulation for subfertility treatment. Lancet 365, 1807–1816 (2005).
della Ragione, T. et al. Developmental stage on day-5 and fragmentation rate on day-3 can influence the implantation potential of top-quality blastocysts in IVF cycles with single embryo transfer. Reprod. Biol. Endocrinol. 5, 2 (2007).
Palermo, G., Joris, H., Devroey, P. & Van Steirteghem, A. C. Pregnancies after intracytoplasmic injection of single spermatozoon into an oocyte. Lancet 340, 17–18 (1992).
Kupker, W. et al. Use of frozen-thawed testicular sperm for intracytoplasmic sperm injection. Fertil. Steril. 73, 453–458 (2000).
Cohen, J. et al. Cryopreservation of single human spermatozoa. Hum. Reprod. 12, 994–1001 (1997).
Van Voorhis, B. J. et al. Effect of the total motile sperm count on the efficacy and cost-effectiveness of intrauterine insemination and in vitro fertilization. Fertil. Steril. 75, 661–668 (2001).
Ohl, D. A. et al. Electroejaculation and assisted reproductive technologies in the treatment of anejaculatory infertility. Fertil. Steril. 76, 1249–1255 (2001).
Sonksen, J. et al. Pregnancy after assisted ejaculation procedures in men with spinal cord injury. Arch. Phys. Med. Rehabil. 78, 1059–1061 (1997).
Lochner-Ernst, D., Mandalka, B., Kramer, G. & Stohrer, M. Conservative and surgical semen retrieval in patients with spinal cord injury. Spinal Cord 35, 463–468 (1997).
Nehra, A., Werner, M. A., Bastuba, M., Title, C. & Oates, R. D. Vibratory stimulation and rectal probe electroejaculation as therapy for patients with spinal cord injury: semen parameters and pregnancy rates. J. Urol. 155, 554–559 (1996).
Dahlberg, A., Ruutu, M. & Hovatta, O. Pregnancy results from a vibrator application, electroejaculation, and a vas aspiration programme in spinal-cord injured men. Hum. Reprod. 10, 2305–2307 (1995).
Rutkowski, S. B. et al. A comprehensive approach to the management of male infertility following spinal cord injury. Spinal Cord 37, 508–514 (1999).
Kathiresan, A. S. et al. Pregnancy outcomes by intravaginal and intrauterine insemination in 82 couples with male factor infertility due to spinal cord injuries. Fertil. Steril. 96, 328–331 (2011).
Leduc, B. E. Treatment of infertility in 31 men with spinal cord injury. Can. J. Urol. 19, 6432–6436 (2012).
Sonksen, J., Fode, M., Lochner-Ernst, D. & Ohl, D. A. Vibratory ejaculation in 140 spinal cord injured men and home insemination of their partners. Spinal Cord 50, 63–66 (2012).
Hultling, C. et al. Assisted ejaculation and in-vitro fertilization in the treatment of infertile spinal cord-injured men: the role of intracytoplasmic sperm injection. Hum. Reprod. 12, 499–502 (1997).
Heruti, R. J. et al. Treatment of male infertility due to spinal cord injury using rectal probe electroejaculation: the Israeli experience. Spinal Cord 39, 168–175 (2001).
Shieh, J. Y. et al. A protocol of electroejaculation and systematic assisted reproductive technology achieved high efficiency and efficacy for pregnancy for anejaculatory men with spinal cord injury. Arch. Phys. Med. Rehabil. 84, 535–540 (2003).
Kathiresan, A. S. et al. Comparison of in vitro fertilization/intracytoplasmic sperm injection outcomes in male factor infertility patients with and without spinal cord injuries. Fertil. Steril. 96, 562–566 (2011).
Raviv, G., Madgar, I., Elizur, S., Zeilig, G. & Levron, J. Testicular sperm retrieval and intra cytoplasmic sperm injection provide favorable outcome in spinal cord injury patients, failing conservative reproductive treatment. Spinal Cord 51, 642–644 (2013).
Author information
Authors and Affiliations
Contributions
M.F. researched data for and wrote the article. All authors made substantial contributions to discussion of content and reviewed/edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
M.F. declares that he has acted as a consultant and speaker for Astellas, Eli Lilly and Menarini. D.A.O. has acted as a consultant for Pfizer and a speaker for Eli Lilly. J.S. has acted as a consultant and speaker for Coloplast, Eli Lilly and Menarini and as a speaker for Astellas, and board member and shareholder in Multicept, Denmark.
Rights and permissions
About this article
Cite this article
Fode, M., Ohl, D. & Sønksen, J. A step-wise approach to sperm retrieval in men with neurogenic anejaculation. Nat Rev Urol 12, 607–616 (2015). https://doi.org/10.1038/nrurol.2015.241
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrurol.2015.241
This article is cited by
-
A rare cause of anejaculation: mitochondrial neurogastrointestinal encephalomyopathy (MNGIE) syndrome: case report
International Journal of Impotence Research (2023)
-
Assisted Reproductive Techniques in Multiple Sclerosis: Recommendations from an Expert Panel
Neurology and Therapy (2023)
-
Clinical use and implications of sexual devices and sexually explicit media
Nature Reviews Urology (2021)
-
Treatment of Delayed Ejaculation
Current Sexual Health Reports (2020)
-
Sexual Dysfunction After Spinal Cord Injury
Current Sexual Health Reports (2020)