Abstract
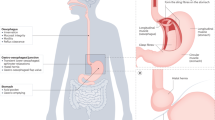
The pathogenesis of gastroparesis is complicated and poorly understood. This lack of understanding remains a major impediment to the development of effective therapies for this condition. Most of the scientific information available on the pathogenesis of gastroparesis has been derived from experimental studies of diabetes in animals. These studies suggest that the disease process can affect nerves (particularly those producing nitric oxide, but also the vagus nerve), interstitial cells of Cajal and smooth muscle. By contrast, human data are sparse, outdated and generally inadequate for the validation of data obtained from experimental models. The available data do, however, suggest that multiple cellular targets are involved. In practice, though, symptoms seldom correlate with objective measures of gastric function and there is still a lot to learn about the pathophysiology of gastroparesis. Future studies should focus on understanding the molecular pathways that lead to gastric dysfunction, in animal models and in humans, and pave the way for the development of rational therapies.
Key Points
-
The pathogenesis of gastroparesis is complex; disruption of gastric function occurs at multiple cellular levels
-
Evidence suggests that the pathogenesis of gastroparesis might involve nerves (particularly those producing nitric oxide, but also the vagus nerve), interstitial cells of Cajal and smooth muscle
-
Most research into the pathogenesis of gastroparesis has been performed in animals; human studies are limited
-
Further studies in animal models and humans are needed to increase our understanding of the molecular pathways that lead to gastric dysfunction so that viable treatment options can be developed
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Parkman HP et al. (2004) American Gastroenterological Association medical position statement: diagnosis and treatment of gastroparesis. Gastroenterology 127: 1589–1591
Maleki D et al. (2000) Gastrointestinal tract symptoms among persons with diabetes mellitus in the community. Arch Intern Med 160: 2808–2816
Soykan I et al. (1998) Demography, clinical characteristics, psychological and abuse profiles, treatment, and long-term follow-up of patients with gastroparesis. Dig Dis Sci 43: 2398–2404
Hoogerwerf WA et al. (1999) Pain: the overlooked symptom in gastroparesis. Am J Gastroenterol 94: 1029–1033
Rayner CK et al. (2001) Relationships of upper gastrointestinal motor and sensory function with glycemic control. Diabetes Care 24: 371–381
Horowitz M et al. (2002) Gastric emptying in diabetes: clinical significance and treatment. Diabet Med 19: 177–194
Horowitz M et al. (2004) Gastric function in diabetes. In Gastrointestinal Function in Diabetes Mellitus, 117 (Eds Horowitz M and Samsom M) Chichester: John Wiley & Sons
Samsom M et al. (2003) Prevalence of delayed gastric emptying in diabetic patients and relationship to dyspeptic symptoms: a prospective study in unselected diabetic patients. Diabetes Care 26: 3116–3122
Guo JP et al. (2001) Extending gastric emptying scintigraphy from two to four hours detects more patients with gastroparesis. Dig Dis Sci 46: 24–29
Lartigue S et al. (1994) Inter- and intrasubject variability of solid and liquid gastric emptying parameters. A scintigraphic study in healthy subjects and diabetic patients. Dig Dis Sci 39: 109–115
Thomforde GM et al. (1995) Evaluation of an inexpensive screening scintigraphic test of gastric emptying. J Nucl Med 36: 93–96
Jones KL et al. (2001) Predictors of delayed gastric emptying in diabetes. Diabetes Care 24: 1264–1269
Tack J et al. (1998) Role of impaired gastric accommodation to a meal in functional dyspepsia. Gastroenterology 115: 1346–1352
Kim DY et al. (2001) Noninvasive measurement of gastric accommodation in patients with idiopathic nonulcer dyspepsia. Am J Gastroenterol 96: 3099–3105
Piessevaux H et al. (2003) Intragastric distribution of a standardized meal in health and functional dyspepsia: correlation with specific symptoms. Neurogastroenterol Motil 15: 447–455
Boeckxstaens GE et al. (2002) The proximal stomach and postprandial symptoms in functional dyspeptics. Am J Gastroenterol 97: 40–48
Bredenoord AJ et al. (2003) Gastric accommodation and emptying in evaluation of patients with upper gastrointestinal symptoms. Clin Gastroenterol Hepatol 1: 264–272
Samsom M et al. (1998) Proximal gastric motor activity in response to a liquid meal in type I diabetes mellitus with autonomic neuropathy. Dig Dis Sci 43: 491–496
Frank JW et al. (1995) Mechanism of accelerated gastric emptying of liquids and hyperglycemia in patients with type II diabetes mellitus. Gastroenterology 109: 755–765
Jebbink RJ et al. (1994) Hyperglycemia induces abnormalities of gastric myoelectrical activity in patients with type I diabetes mellitus. Gastroenterology 107: 1390–1397
Chen JD et al. (1996) Abnormal gastric myoelectrical activity and delayed gastric emptying in patients with symptoms suggestive of gastroparesis. Dig Dis Sci 41: 1538–1545
Samsom M et al. (1995) Compliance of the proximal stomach and dyspeptic symptoms in patients with type I diabetes mellitus. Dig Dis Sci 40: 2037–2042
Takahashi T and Owyang C (1995) Vagal control of nitric oxide and vasoactive intestinal polypeptide release in the regulation of gastric relaxation in rat. J Physiol 484 (Part 2): 481–492
Shah V et al. (2004) Nitric oxide in gastrointestinal health and disease. Gastroenterology 126: 903–913
Mashimo H et al. (2000) Gastric stasis in neuronal nitric oxide synthase-deficient knockout mice. Gastroenterology 119: 766–773
Anvari M et al. (1998) Role of nitric oxide mechanisms in control of pyloric motility and transpyloric flow of liquids in conscious dogs. Dig Dis Sci 43: 506–512
Orihata M and Sarna SK (1994) Inhibition of nitric oxide synthase delays gastric emptying of solid meals. J Pharmacol Exp Ther 271: 660–670
Plourde V et al. (1994) Delayed gastric emptying induced by inhibitors of nitric oxide synthase in rats. Eur J Pharmacol 256: 125–129
Takahashi T et al. (1997) Impaired expression of nitric oxide synthase in the gastric myenteric plexus of spontaneously diabetic rats. Gastroenterology 113: 1535–1544
Jenkinson KM and Reid JJ (1995) Effect of diabetes on relaxations to non-adrenergic, non-cholinergic nerve stimulation in longitudinal muscle of the rat gastric fundus. Br J Pharmacol 116: 1551–1556
Wrzos HF et al. (1997) Nitric oxide synthase (NOS) expression in the myenteric plexus of streptozotocin-diabetic rats. Dig Dis Sci 42: 2106–2110
Adeghate E et al. (2003) Increase in neuronal nitric oxide synthase content of the gastroduodenal tract of diabetic rats. Cell Mol Life Sci 60: 1172–1179
Spangeus A and El-Salhy M (2001) Myenteric plexus of obese diabetic mice (an animal model of human type 2 diabetes). Histol Histopathol 16: 159–165
Spangeus A et al. (2000) Diabetic state affects the innervation of gut in an animal model of human type 1 diabetes. Histol Histopathol 15: 739–744
El-Salhy M and Spangeus A (1998) Substance P in the gastrointestinal tract of non-obese diabetic mice. Scand J Gastroenterol 33: 394–400
El-Salhy M and Spangeus A (2002) Gastric emptying in animal models of human diabetes: correlation to blood glucose level and gut neuroendocrine peptide content. Ups J Med Sci 107: 89–99
Watkins CC et al. (2000) Insulin restores neuronal nitric oxide synthase expression and function that is lost in diabetic gastropathy. J Clin Invest 106: 373–384
Guo C et al. (2004) Diabetic autonomic neuropathy: evidence for apoptosis in situ in the rat. Neurogastroenterol Motil 16: 335–345
Hall AV et al. (1994) Structural organization of the human neuronal nitric oxide synthase gene (NOS1). J Biol Chem 269: 33082–33090
Wang Y and Marsden PA (1995) Nitric oxide synthases: gene structure and regulation. Adv Pharmacol 34: 71–90
Wang Y et al. (1999) Neuronal NOS: gene structure, mRNA diversity, and functional relevance. Crit Rev Neurobiol 13: 21–43
Wang Y et al. (1999) RNA diversity has profound effects on the translation of neuronal nitric oxide synthase. Proc Natl Acad Sci USA 96: 12150–12155
Cellek S (2004) Point of NO return for nitrergic nerves in diabetes: a new insight into diabetic complications. Curr Pharm Des 10: 3683–3695
Cellek S et al. (2003) Two phases of nitrergic neuropathy in streptozotocin-induced diabetic rats. Diabetes 52: 2353–2362
Cellek S et al. (2004) Synergistic action of advanced glycation end products and endogenous nitric oxide leads to neuronal apoptosis in vitro: a new insight into selective nitrergic neuropathy in diabetes. Diabetologia 47: 331–339
Korenaga K et al. (2006) Suppression of nNOS expression in rat enteric neurones by the receptor for advanced glycation end-products. Neurogastroenterol Motil 18: 392–400
Nakamura K et al. (1998) Nicotinic receptor mediates nitric oxide synthase expression in the rat gastric myenteric plexus. J Clin Invest 101: 1479–1489
Ghosh DK et al. (1996) Domains of macrophage N(O) synthase have divergent roles in forming and stabilizing the active dimeric enzyme. Biochemistry 35: 1444–1449
Gangula PR et al. (2007) Diabetes induces sex-dependent changes in neuronal nitric oxide synthase dimerization and function in the rat gastric antrum. Am J Physiol Gastrointest Liver Physiol 292: G725–G733
Koya D and King GL (1998) Protein kinase C activation and the development of diabetic complications. Diabetes 47: 859–866
Gibson TM et al. (2003) Effects of alpha-lipoic acid on impaired gastric fundus innervation in diabetic rats. Free Radic Biol Med 35: 160–168
Dishy V et al. (2004) The effect of sildenafil on gastric emptying in patients with end-stage renal failure and symptoms of gastroparesis. Clin Pharmacol Ther 76: 281–286
Sun WM et al. (1998) Effects of nitroglycerin on liquid gastric emptying and antropyloroduodenal motility. Am J Physiol 275: G1173–1178
Ordog T et al. (2000) Remodeling of networks of interstitial cells of Cajal in a murine model of diabetic gastroparesis. Diabetes 49: 1731–1739
Horvath VJ et al. (2006) Reduced stem cell factor links smooth myopathy and loss of interstitial cells of cajal in murine diabetic gastroparesis. Gastroenterology 130: 759–770
Horvath VJ et al. (2005) Reduced insulin and IGF-I signaling, not hyperglycemia, underlies the diabetes-associated depletion of interstitial cells of Cajal in the murine stomach. Diabetes 54: 1528–1533
Choi K et al. (2005) Loss of neuronal nitric oxide synthase results in altered volume and distribution of interstitial cells of Cajal in mouse stomach [abstract]. Neurogastroenterol Motil 17: 612
Tashima K et al. (2000) Gastric acid secretion in streptozotocin-diabetic rats—different responses to various secretagogues. J Physiol Paris 94: 11–17
Tashima K et al. (2000) Acid secretory changes in streptozotocin-diabetic rats: different responses to various secretagogues. Dig Dis Sci 45: 1352–1358
Ishiguchi T et al. (2001) Gastric distension-induced pyloric relaxation: central nervous system regulation and effects of acute hyperglycaemia in the rat. J Physiol 533: 801–813
Ishiguchi T et al. (2002) Hyperglycemia impairs antro-pyloric coordination and delays gastric emptying in conscious rats. Auton Neurosci 95: 112–120
Kniel PC et al. (1986) Varied effects of experimental diabetes on the autonomic nervous system of the rat. Lab Invest 54: 523–530
Yagihashi S and Sima AA (1986) Diabetic autonomic neuropathy in BB rat. Ultrastructural and morphometric changes in parasympathetic nerves. Diabetes 35: 733–743
Schmidt RE et al. (1983) Experimental diabetic autonomic neuropathy characterization in streptozotocin-diabetic Sprague-Dawley rats. Lab Invest 49: 538–552
Tay SS and Wong WC (1994) Short- and long-term effects of streptozotocin-induced diabetes on the dorsal motor nucleus of the vagus nerve in the rat. Acta Anat (Basel) 150: 274–281
Lee PG et al. (2002) Streptozotocin-induced diabetes reduces retrograde axonal transport in the afferent and efferent vagus nerve. Brain Res 941: 127–136
Lee PG et al. (2001) Streptozotocin-induced diabetes causes metabolic changes and alterations in neurotrophin content and retrograde transport in the cervical vagus nerve. Exp Neurol 170: 149–161
Cai F and Helke CJ (2003) Abnormal PI3 kinase/Akt signal pathway in vagal afferent neurons and vagus nerve of streptozotocin-diabetic rats. Brain Res Mol Brain Res 110: 234–244
Carroll SL et al. (2004) Ganglion-specific patterns of diabetes-modulated gene expression are established in prevertebral and paravertebral sympathetic ganglia prior to the development of neuroaxonal dystrophy. J Neuropathol Exp Neurol 63: 1144–1154
Schmidt RE (2002) Neuropathology and pathogenesis of diabetic autonomic neuropathy. Int Rev Neurobiol 50: 257–292
Schmidt RE et al. (2003) Non-obese diabetic mice rapidly develop dramatic sympathetic neuritic dystrophy: a new experimental model of diabetic autonomic neuropathy. Am J Pathol 163: 2077–2091
Schmidt RE et al. (2004) Experimental rat models of types 1 and 2 diabetes differ in sympathetic neuroaxonal dystrophy. J Neuropathol Exp Neurol 63: 450–460
Schmidt RE et al. (2003) Analysis of the Zucker diabetic fatty (ZDF) type 2 diabetic rat model suggests a neurotrophic role for insulin/IGF-I in diabetic autonomic neuropathy. Am J Pathol 163: 21–28
Bansal V et al. (2006) Diabetic neuropathy. Postgrad Med J 82: 95–100
Vinik AI et al. (2003) Diabetic autonomic neuropathy. Diabetes Care 26: 1553–1579
Liao D et al. (2006) Three-dimensional geometry analysis of the stomach in type II diabetic GK rats. Diabetes Res Clin Pract 71: 1–13
Takahashi T et al. (1996) Impaired intracellular signal transduction in gastric smooth muscle of diabetic BB/W rats. Am J Physiol 270: G411–G417
Soulie ML et al. (1992) Impairment of contractile response to carbachol and muscarinic receptor coupling in gastric antral smooth muscle cells isolated from diabetic streptozotocin-treated rats and db/db mice. Mol Cell Biochem 109: 185–188
James AN et al. (2004) Regional gastric contractility alterations in a diabetic gastroparesis mouse model: effects of cholinergic and serotoninergic stimulation. Am J Physiol Gastrointest Liver Physiol 287: G612–G619
Lam WF et al. (1993) Hyperglycemia reduces gastric secretory and plasma pancreatic polypeptide responses to modified sham feeding in humans. Digestion 54: 48–53
Mearin F et al. (1986) Pyloric dysfunction in diabetics with recurrent nausea and vomiting. Gastroenterology 90: 1919–1925
Yoshida MM et al. (1988) There are no morphologic abnormalities of the gastric wall or abdominal vagus in patients with diabetic gastroparesis. Gastroenterology 94: 907–914
Guy RJ et al. (1984) Diabetic gastroparesis from autonomic neuropathy: surgical considerations and changes in vagus nerve morphology. J Neurol Neurosurg Psychiatry 47: 686–691
Ejskjaer NT et al. (1999) Novel surgical treatment and gastric pathology in diabetic gastroparesis. Diabet Med 16: 488–495
Zarate N et al. (2003) Severe idiopathic gastroparesis due to neuronal and interstitial cells of Cajal degeneration: pathological findings and management. Gut 52: 966–970
Forster J et al. (2005) Absence of the interstitial cells of Cajal in patients with gastroparesis and correlation with clinical findings. J Gastrointest Surg 9: 102–108
Iwasaki H et al. (2006) A deficiency of gastric interstitial cells of Cajal accompanied by decreased expression of neuronal nitric oxide synthase and substance P in patients with type 2 diabetes mellitus. J Gastroenterol 41: 1076–1087
Pasha SF et al. (2006) Autoimmune gastrointestinal dysmotility treated successfully with pyridostigmine. Gastroenterology 131: 1592–1596
De Giorgio R et al. (2003) Anti-HuD-induced neuronal apoptosis underlying paraneoplastic gut dysmotility. Gastroenterology 125: 70–79
Srinivasan S et al. (1998) Serum from patients with type 2 diabetes with neuropathy induces complement-independent, calcium-dependent apoptosis in cultured neuronal cells. J Clin Invest 102: 1454–1462
Pardi DS et al. (2002) Paraneoplastic dysmotility: loss of interstitial cells of Cajal. Am J Gastroenterol 97: 1828–1833
Jackson MW et al. (2004) Disruption of intestinal motility by a calcium channel-stimulating autoantibody in type 1 diabetes. Gastroenterology 126: 819–828
Sigurdsson L et al. (1997) Postviral gastroparesis: presentation, treatment, and outcome. J Pediatr 131: 751–754
Pande H et al. (2002) Inflammatory causes of gastroparesis: report of five cases. Dig Dis Sci 47: 2664–2668
De Giorgio R et al. (2000) Idiopathic myenteric ganglionitis underlying intractable vomiting in a young adult. Eur J Gastroenterol Hepatol 12: 613–616
Ward SM et al. (2004) Role of interstitial cells of Cajal in neural control of gastrointestinal smooth muscles. Neurogastroenterol Motil 16 (Suppl 1): 112–117
Strege PR et al. (2003) Sodium current in human intestinal interstitial cells of Cajal. Am J Physiol Gastrointest Liver Physiol 285: G1111–G1121
Hirst GD and Edwards FR (2004) Role of interstitial cells of Cajal in the control of gastric motility. J Pharmacol Sci 96: 1–10
Holzer P (2002) Sensory neuron responses to mucosal noxae in the upper gut: relevance to mucosal integrity and gastrointestinal pain. Neurogastroenterol Motil 14: 459–475
Berthoud HR et al. (2004) Neuroanatomy of extrinsic afferents supplying the gastrointestinal tract. Neurogastroenterol Motil 16 (Suppl 1): 28–33
Grundy D (2006) Signalling the state of the digestive tract. Auton Neurosci 125: 76–80
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Vittal, H., Farrugia, G., Gomez, G. et al. Mechanisms of Disease: the pathological basis of gastroparesis—a review of experimental and clinical studies. Nat Rev Gastroenterol Hepatol 4, 336–346 (2007). https://doi.org/10.1038/ncpgasthep0838
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1038/ncpgasthep0838
This article is cited by
-
Impairment of Nrf2- and Nitrergic-Mediated Gastrointestinal Motility in an MPTP Mouse Model of Parkinson’s Disease
Digestive Diseases and Sciences (2019)
-
Enhanced Recovery After Surgery (ERAS®) in Individuals with Diabetes: A Systematic Review
World Journal of Surgery (2017)
-
Influence of Musa sapientum L. on pharmacokinetic of metformin in diabetic gastroparesis
Chinese Journal of Integrative Medicine (2016)
-
Gastric emptying and glycaemia in health and diabetes mellitus
Nature Reviews Endocrinology (2015)
-
Diabetic Gastroparesis: Functional/Morphologic Background, Diagnosis, and Treatment Options
Current Diabetes Reports (2014)