Abstract
Objective:
To describe infant mortality trends and associated factors among infants born to mothers enrolled in a prevention of mother-to-child transmission (PMTCT) program.
Study Design:
A nested case–control study of human immunodeficiency virus (HIV)-positive and -negative pregnant women enrolled from the national PMTCT program at 36 weeks of gestation attending three peri-urban clinics in Zimbabwe offering maternal and child health care. Mother–infant pairs were followed up from delivery, and at 6 weeks, 4 months and 9 months.
Results:
A total of 1045 mother and singleton infant pairs, 474 HIV-positive and 571 HIV-negative mothers, delivered 469 and 569 live infants, respectively. Differences in mortality were at 6 weeks and 4 months, RR (95% CI) 9.71 (1.22 to 77.32) and 21.84 (2.93 to 162.98), respectively. Overall, 9-month mortality rates were 150 and 47 per 1000 person-years for infants born to HIV-positive and HIV-negative mothers, respectively. Proportional hazard ratio of mortality for children born to HIV-positive mothers was 3.21 (1.91 to 5.38) when compared with that for children born to HIV-negative mothers.
Conclusion:
Maternal HIV exposure was associated with higher mortality in the first 4 months of life. Infant's HIV status was the strongest predictor of infant mortality. There is a need to screen infants for HIV from delivery and throughout breastfeeding.
Similar content being viewed by others
Introduction
Prevention of mother-to-child transmission (PMTCT) of human immunodeficiency virus (HIV) has become one of the essential elements of the control strategies for the African HIV pandemic.1, 2, 3
HIV infection has been noted to affect child mortality directly by mother-to-child transmission (MTCT) and indirectly by maternal HIV status, as a mother's death has a negative impact on the child's health.4 The epidemic among children mirrors that among women of childbearing age.5 Child mortality is a possible outcome for PMTCT interventions, as cases of pediatric HIV infection averted should also translate into deaths averted. However, the results of some trials suggest otherwise, especially in the first 2 years of life.5, 6, 7
To observe a meaningful difference in child mortality, some authors suggest a prolonged follow-up of up to 5 years, whereas others feel that it is important to establish age-specific child mortality.1, 8 Children born to HIV-infected mothers are estimated to be thrice more likely to die than those born to HIV-negative mothers and this has been observed to continue throughout the childhood years.9, 10, 11, 12 In Zimbabwe, infant mortality has been found to be 17% among infants born to HIV-infected mothers and 2% among seronegative mothers before any PMTCT interventions.3, 12, 13
In this paper, we describe age-specific mortality trends of children born to HIV-positive and -negative mothers delivered under a PMTCT program. The aim is to find the extent to which PMTCT intervention has influenced child mortality in this Zimbabwean cohort. We also describe and compare the risk factors for infant mortality by maternal HIV status in this population.
Methods
Design of the study: A nested case–control study enrolled pregnant women from the national PMTCT program.
Study sites: Three peri-urban clinics around Harare (Epworth; St Mary's and Seke North) offering maternal and child health services participated in the study.
Study population: Infants born to mothers booked at the respective Antenatal Clinics, having gone through voluntary counseling and testing under the national PMTCT program, were followed up together with their mothers from delivery up to 9 months after birth.
Inclusion criteria: Women from the national PMTCT program who were 36-week pregnant and had received pre- and post-HIV counseling were included if they intended to deliver their index infants at one of the three participating study sites. Multiple births were excluded.
Baseline assessments: A questionnaire sourcing sociodemographic, reproductive history, contraception and knowledge of STI/HIV signs and symptoms, as well as feeding practices was interview-administered to the mothers.
Intervention: HIV-positive mothers received a single 200 mg nevirapine dose at the onset of labor, and their infants received a single 1 to 2 mg nevirapine dose within 72 h of delivery. Follow-up of the infants started at delivery with a physical examination including anthropometrical measurements.
Cord blood was collected from the infant at birth and thereafter venous blood was collected at each follow-up visit; 6 weeks, 4 months and 9 months for HIV-DNA PCR test using cell pellets by prototype Roche Amplicor version 1.5 qualitative PCR assay (Roche Diagnostic Systems, Branchburg, New Jersey, USA). Infant feeding practices were also assessed at each time point. Infants were classified at birth according to maternal HIV status that was determined at approximately 36 weeks of gestation and this status was maintained for this analysis throughout the ‘9 months’ of follow-up.
At each scheduled visit, information was sourced from the mother about the health status of the infant. For this analysis, the mother and infant were considered alive if they showed up for their visit or in cases of migration home visits were conducted and their relatives confirmed that they were alive during the period under observation. They were considered dead through evidence from verbal autopsy for the infant given by either the mother or caregiver and for the mother by the next of kin. Where available and possible, clinical records were also assessed to ascertain the cause of death. The potential child mortality risk factors included were birth weight, breastfeeding, infant's HIV serostatus, mother's age, marital status and maternal HIV status.
Age-specific mortality was assessed at delivery, and at 6 weeks, 4 months and 9 months.
Ethical considerations: Both the Medical Research Council of Zimbabwe and the Ethical Review Committee in Norway approved the study.
Mothers who agreed to participate in the study gave informed written consent for themselves and their index infants to be followed up from delivery.
Statistical analysis
Data were entered and analyzed using SPSS and STATA Version 9 from StataCorp, College Station, TX, USA. Infants' anthropometrical characteristics at delivery were described according to the maternal HIV status and a description of the maternal baseline characteristics was given.
A table showing deceased infants and the proportions dying by maternal HIV status at each scheduled stipulated study visit is presented. Calculations were carried out to show the deaths, percentage of deceased infants by covariates, relative risks with their 95% confidence interval for the covariates and stratified by HIV status. Stepwise regression was used to construct models showing the most significant covariates for 9-month child mortality. Survival analysis was used to calculate 9-month mortality rates, proportional hazard ratio for death due to HIV, as well as log-rank tests for equality of survival analysis. We further analyzed the effect of infant feeding options on mortality, that is, mixed feeding, exclusive breastfeeding and not having been breastfed at all. Statistical calculations were carried out only on singleton and live born infants.
Results
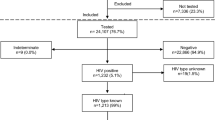
A total of 479 HIV-positive and 571 HIV-negative pregnant women were included in the study and they delivered 484 (five of which were multiple births) and 571 infants, respectively. After exclusion of 5 multiple births and 7 stillbirths, 469 HIV-positive and 569 HIV-negative mother–infant pairs were included in this analysis.
Characteristics of the mothers
HIV-positive mothers were older than the HIV-negative mothers, mean (s.d.) age in years 26.1 (4.9) and 23.5 (5.0) P<0.001. They also reported more pregnancies and had more children, mean (s.d.) pregnancy 2.5 (1.2) and parity of 1.6 (1.2) compared with 2.0 (1.1) and parity of 0.9 (1.1) for the HIV-negative mothers, respectively, P<0.001.
Infants' characteristics
Anthropometrical measurements of the infants at birth were significantly different in terms of mean weight and length between those born of HIV-positive and those of HIV-negative mothers (Table 1).
Mortality
Over the 9 months of follow-up, a total of 51 (10.9%) infants of HIV-positive mothers died compared with 20 (3.5%) born to HIV-negative mothers, P<0.001. Mortality rates of 9 months were 150 per 1000 person-years among infants born to HIV-positive and 47 per 1000 person-years among those born to HIV-negative mothers. Proportional hazard ratio for mortality over the 9-month period for children born to HIV-positive mothers was 3.21 (1.91 to 5.38) when compared with that for children born to HIV-negative mothers. The log-rank test for equality of the survival function for children born to HIV-positive mothers was significantly different from that for children born to HIV-negative mothers, P< 0.001.
Significant differences in child mortality by HIV status were observed at 6 weeks and 4 months, whereas at 9 months the differences in mortality had disappeared (see Table 2).
Among the 91 infants who tested HIV-positive over the 9-month period, 24.2% of them died compared with 5.2% of those who did not seroconvert, relative risk 4.67 (2.97 to 7.36), P<0.001.
Infant- and maternal-related risk factors
In univariate analysis among infants born to HIV-positive mothers, infant HIV positivity, having a deceased mother and low birth weight were significant risk factors for 9-month infant mortality. Infants not breastfed at all had the highest risk of dying compared with those exclusively breastfed or had mixed feeding regardless of the mother's HIV status (Table 3).
Among infants born to HIV-negative mothers, having a deceased mother was the only risk factor for mortality (see Table 4). After the stepwise multivariate analysis among infants born to HIV-positive mothers, it is the infant's HIV infection that remained as the only significant risk factor for mortality at 9 months, incidence risk rate 5.30 (2.15 to 13.05). Among infants born to HIV-negative mothers, having a deceased mother remained a significant risk factor, incidence risk rate 40.41 (19.36 to 84.38), P=0.001.
Discussion
Maternal HIV-positive status significantly predisposes the infants to higher mortality, especially in the first 4 months of life. Consistent with the previous studies even before PMTCT, maternal HIV exposure increased the risk of infant mortality. This risk is regardless of the fact that the infant would have escaped the infection itself.1, 2, 3, 4 The excess risk for mortality in our study is slightly higher than that reported by Zaba10 in the cohort of three countries.
There is need for further research with regards to maternal HIV status and intrauterine, intrapartum deaths. High infant mortality was observed among infants who tested DNA PCR-positive at birth, with about 24% of them dying in the first 9 months of life. This emphasizes the shortcomings of the single-dose antiretroviral prophylaxis, thus supporting what previous studies have observed that the majority of the deceased infants were infected in utero.9, 12
Significant differences were observed at the 6-week visit among infants of HIV-positive mothers as compared with those born to HIV-negative mothers. This difference in mortality reached a peak at 4 months where infants born of HIV-positive mothers were almost 22 times more likely to die. The peak period of this mortality is when solid foods or animal milk is introduced to the infants. Mixed feeding predisposes the infant to scarring and sores in the intestines, thereby facilitating the entry of the HIV virus. It also predisposes the infants to risk of diarrheal and respiratory infections.13 At 9 months, there was no difference in mortality among infants born to HIV-negative and HIV-positive mothers. This is in agreement with other reports observing that child mortality decreases with age.4, 5, 6, 7, 8, 11, 12 Although few studies have reported on period infant mortality, the mortality trend in our study indicates that those infants who survive the first 4 months of life have a higher chance of survival irrespective of the mother's HIV serostatus.9, 10 Overall about 8% of the infants had a low birth weight and around 14% of them died within the first 9 months of life. Although not statistically significant, infants not breastfed at all were more likely to die regardless of maternal HIV status. This is mostly attributed to the fact that these infants will succumb to other infections such as diarrhea or malnutrition itself.3 On the other hand, low birth weight infants, if not breastfed, are more likely to die especially in low-income countries, as has been reported in other studies.9 This can also be attributed to the counseling and support on feeding options, which is more focused and targeted toward the HIV-positive mothers. HIV-negative mothers who decided not to breastfeed, doubting their status, could have considered themselves at risk, but unfortunately they did not get the kind of support given to their counterparts. Feeding options and HIV remain a controversial issue with different outcomes according to different settings.3 However, in this study where over 85% of the infants were breastfed regardless of the mother's HIV status, the small number of infants who were not breastfed at all could have affected our observation.
Low birth weight was the only infant-related risk factor that was significantly associated with higher mortality for infants born to HIV-positive mothers. It was, however, confounded by other factors in the multivariate model. Maternal death was a strong predictor of infant mortality regardless of the mother's HIV status. This is consistent with reported studies whereby maternal health directly affects the infant's health.4 Risk factors for infant mortality were more pronounced among infants born to HIV-positive mothers than for the HIV-negative mothers. The HIV status of the infant itself came out as the strongest predictor of whether the child would survive or not, even after controlling for other factors. The importance of screening all HIV-exposed infants at delivery and throughout the breastfeeding period cannot be over emphasized. There should be close clinical monitoring for the HIV-seropositive infants, for CD4 counts, viral loads and commencing them on ARV drugs as and when appropriate.
This study was conducted at the time when PMTCT initiatives were being introduced in the country. This information on infant mortality while PMTCT was in its infancy will provide some insight into the impact of PMTCT on child mortality. Most of the infants in our study died from respiratory tract infections and diarrheal diseases, but we did not go further into assessing the actual morbidity leading to a particular death for this paper. This restricts the extent to which we can generalize this observation.12 However, we have managed to highlight the age-specific effect of maternal HIV exposure and the risk factors for infant mortality in the PMTCT era.
Risk factors associated with higher infant mortality were maternal mortality and for infant-related factors it was infant's HIV status and low birth weight, the former being the strongest predictor of infant survival. Infant mortality remains high in this HIV-prevalent population and more effort has to be put in establishing the actual cause of this high mortality even within PMTCT initiatives.
We conclude that maternal HIV exposure is associated with higher mortality in the first 4 months of life. Prevention of HIV among women remains a priority. There is need to strengthen current PMTCT programs, by screening pregnant women early for HIV and giving more efficacious drug regimens to HIV-positive mothers guided by their CD4 and viral load counts. Interventions to reduce both HIV transmission and infant mortality should be targeted in the first 4 months of life. All infants born to HIV-positive mothers should be screened for HIV at delivery and throughout the breastfeeding period, and ARV therapy should be initiated as and when necessary, offering continued clinical care and support.
Conflict of interest
The authors declare no conflict of interest.
References
Alioum A, Dabis F, Dequae-Merchadou L, Haverkamp G, Hudgens M, Hughes J et al. Estimating the efficacy of interventions to prevent mother to child transmission of HIV in breastfeeding populations: development of consensus methodology. Stat Med 2001; 20: 3539–3556.
Dabis F, Leroy V, Castetbon K, Spira R, Newell M, Salamon R . Preventing mother to child transmission of HIV-1 in Africa in the year 2000. AIDS 2000; 14: 1017–1026.
Iliff PJ, Piwoz EG, Tavengwa NV, Zunguza CD, Marinda ET, Nathoo KJ et al. Early exclusive breastfeeding reduces the risk of postnatal HIV-1 transmission and increases HIV-free survival. AIDS 2005; 19: 699–708.
Newell ML, Brahmbhatt H, Ghys PD . Child mortality and HIV infection in Africa: a review. AIDS 2004; 18 (2): S27–S34.
Taha TE, Kumwenda NI, Broadhead RL, Hoover DR, Graham SM, Van der hoven L et al. Mortality after the first year of life among human immunodeficiency virus type 1-infected and uninfected children. Pediatr Infec Dis J 1999; 18: 689–694.
The Petra Study Team. Efficacy of three short-course regimens of zidovudine and lamivudine in preventing early and late transmission of HIV-1 from mother to child in Tanzania, South Africa, and Uganda (Petra study): a randomized, double-blind, placebo-controlled trial. Lancet 2002; 359: 117–186.
Nduati R, John G, Mbori-Ngacha D, Richardson B, Overbaugh J, Mwatha A et al. Effect of breastfeeding and formula feeding on transmission of HIV-1: a randomized clinical trial. JAMA 2000; 283: 1167–1174.
Crampin AC, Floyd S, Glyn JR, Madise N, Nyondo A, Khondowe MM et al. The long-term impact of HIV and orphan hood on the mortality and physical well-being of children in rural Malawi. AIDS 2003; 17 (3): 389–397.
Newell ML, Coovadia H, Cortina-Boria M, Rollins N, Gaillard P, Dabis F . Mortality of infected and uninfected infants born to HIV-infected mothers in Africa: a pooled analysis. Lancet 2004; 364: 1236–1243.
Zaba B, Whitworth J, Marston M, Nakiyingi J, Ruberantwari A, Urassa M et al. HIV and mortality of mothers and children: evidence from cohort studies in Uganda, Tanzania and Malawi. Epidemiology 2005; 16 (3): 275–280.
Brahmbhatt H, Kigoz G, Wabwire-Mangen F, Serwadda D, Lutalo T, Nalugoda F et al. Mortality in HIV infected and Uninfected children of HIV-infected and uninfected mothers in rural Uganda. J Acquir Immune Defic Syndr 2006; 41: 504–508.
Zijenah L, Mbizvo MT, Kasule J, Nathoo K, Munjoma M, Mahomed K et al. Mortality in the first 2 years among infants born to human immunodeficiency virus-infected women in Harare, Zimbabwe. J Infect Dis 1998; 178: 109–113.
Nathoo K, Rusakaniko S, Zijenah LS, Kasule J, Mahomed K, Mhashu A et al. Survival pattern among infants born to human immunodeficiency virus type-1 infected mothers and uninfected mothers in Harare, Zimbabwe. Cent Afr J Med 2004; 50: 1–6.
Acknowledgements
The authors gratefully acknowledge the women and infants who participated in the study. Special mention goes to the LETTEN Foundation and Professor Letten F Saugstad herself, for funding this study. Special thanks to the local clinic authorities, study nurses, counselors and laboratory, and support staff at the College of Health Sciences, Department of Obstetrics and Gynaecology and Department of Pediatrics.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-No Derivative Works 3.0 License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Kurewa, E., Gumbo, F., Munjoma, M. et al. Effect of maternal HIV status on infant mortality: evidence from a 9-month follow-up of mothers and their infants in Zimbabwe. J Perinatol 30, 88–92 (2010). https://doi.org/10.1038/jp.2009.121
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2009.121
Keywords
This article is cited by
-
Dynamics of the infant gut microbiota in the first 18 months of life: the impact of maternal HIV infection and breastfeeding
Microbiome (2022)
-
The University of Zimbabwe College of Health Sciences (UZ-CHS) BIRTH COHORT study: rationale, design and methods
BMC Infectious Diseases (2020)
-
Predictors of mortality among HIV exposed infants at University of Gondar Comprehensive Specialized Hospital, Northwest Ethiopia
Italian Journal of Pediatrics (2019)
-
Externalities of Prevention of Mother-to-Child Transmission Programs: A Systematic Review
AIDS and Behavior (2013)
-
Preventing mother-to-child HIV transmission in Zimbabwe
Journal of Perinatology (2010)