Abstract
A serotonin transporter gene, SLC6A4, is thought to be related to nicotine dependence and depression, one of the comorbidities of chronic obstructive pulmonary disease (COPD). To investigate the association between SLC6A4 variation and tobacco consumption, susceptibility to COPD, and depression status. In all, 247 patients with COPD and 119 control subjects were genotyped for 5 tag single-nucleotide polymorphisms (SNPs) of SLC6A4. We analyzed the correlation between these genotypes and COPD, using the results of a pulmonary function test or chest computed tomography; data on tobacco consumption (pack-years); and the depression score based on the hospital anxiety and depression scale (HADS) after adjusting for age, gender, and smoking status (and pack-years, when appropriate). The rare allele rs2020936 was significantly associated with COPD incidence in the trend model (P=0.003; odds ratio, 2.20; 95% confidence interval, 1.31–3.74). This allele was also associated with the number of pack-years (P=0.026). The major allele of another SNP of SLC6A4, namely rs3794808, correlated with the HADS depression score (P=0.016). We conclude that SLC6A4 variation affects COPD pathogenesis, and this effect depends partly on tobacco consumption. SLC6A4 variation also affects depressive symptoms. SLC6A4 could be modified to prevent COPD and treat the depressive symptoms of COPD.
Similar content being viewed by others
Introduction
Chronic obstructive pulmonary disease (COPD) is now becoming the most prevalent respiratory disease, and it is estimated that COPD will be the fifth most prevalent disease in the world in 2020.1 As only 10–20% of heavy smokers develop symptomatic COPD,2 susceptibility to COPD is thought to depend on environmental and genetic factors.
Genetic factors other than α-1-antitrypsin (A1AT) might influence the susceptibility of an individual to COPD.3 Some genes related to nicotine dependence, including nicotine receptors and those involved in the dopamine and serotonin pathways,4 are believed to be good candidates for genetic risk factors of COPD. CYP2A6 and α-nicotinic acetylcholine receptor (CHRNA 3/5) were investigated as candidate genes involved in COPD pathogenesis;5, 6 however, the association between many genes and COPD remains to be studied.
A serotonin transporter gene, solute carrier family 6, member 4 (SLC6A4) (or 5-hydroxytryptamine transporter: 5-HTT), which is involved in serotonin reuptake in the serotonin pathway, is thought to be a good candidate for a gene associated with tobacco consumption and COPD and also depression, which is one of the important comorbidities of COPD.7 SLC6A4 is thought to be closely related to nicotine dependence4 and smoking behaviour in the Japanese8and Chinese.9 SLC6A4 variation has also been reported to be related to depression.10 Depression markedly affects the quality of life, exacerbation and hospitalisation, and mortality in COPD.11, 12 As a twin study with a large population suggested that the association between smoking and depression arises largely from genetic factors,13 it could be postulated that smoking, COPD and depression are affected by the same genetic factors, including SLC6A4.
In this study, we investigated whether single-nucleotide polymorphisms (SNPs) of SLC6A4 are correlated with tobacco consumption, susceptibility to COPD and its depressive symptoms.
Materials and methods
Study subjects
The subjects were consecutive patients who initially consulted in the outpatient clinic of the Respiratory Care Clinic, Nippon Medical School, Tokyo, Japan, a secondary care specialist COPD clinic. They received ambulatory treatment without exacerbations from May 2007 to February 2009. Eligible patients fulfilled the following criteria: their clinical course, clinical symptoms and laboratory data satisfied the criteria for the clinical diagnosis of COPD, according to the COPD guidelines published by the Global Initiative for Chronic Obstructive Lung Disease,14 and they were current or ex-smokers with airflow limitation (forced expiratory volume in 1 s (FEV1)/forced vital capacity (FVC), <70%). The control subjects were current or ex-smokers (number of pack-years, >20) who had visited our clinic with some respiratory symptoms but no airflow limitation; these were considered as ‘stage 0’ subjects.15
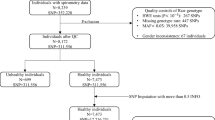
Blood samples were obtained from 367 current or ex-smokers (67.8±9.8 years old, 328 males and 39 females), comprising COPD patients (n=247) and control subjects (n=119). The basic characteristics of the subjects are shown in Table 1.
This study was approved by the ethics committee of the institute, and the subjects were enroled after appropriate informed consent was obtained.
Pulmonary function testing
Pulmonary function parameters, including the post-bronchodilator FEV1, carbon monoxide diffusing capacity (DLCO/VA), vital capacity (VC) and forced vital capacity, were measured according to the American Thoracic Society guidelines.16 using equipment for lung function testing with computer processing (CHESTAC; CHEST, Tokyo, Japan). The reference values of post-bronchodilator FEV1 and VC used were according to the standards of the Japanese Respiratory Society.17
High-resolution computed tomography (HRCT) of the chest
Emphysema severity and airway remodelling were determined on the basis of HRCT scans obtained at full inspiration, as in our previous study.18 Helical computed tomography scans were acquired with a 1.25-mm collimation, a scan time (rotation time) of 0.8 s, 120 kV and 100∼600 mA, using a Light Speed Pro16 computed tomography scanner (GE, Tokyo, Japan).
Analysis of the low-attenuation area
We calculated the percentage low-attenuation area (LAA%) on HRCT scans, using the method of Nakano et al.19 with a minor modification. Briefly, six slices were obtained of the upper, middle and lower lobes of the bilateral lungs. The upper slice was obtained at the aortic arch, the middle section was obtained at the carina and the lower section was obtained at ∼3 cm above the top of the diaphragm. The voxels within each field were categorised as emphysema based on a grey scale image that was reconstructed using Hounsfield units. A density histogram, based on the distribution of the number of voxels at each Hounsfield unit within the lung, was plotted; values <–940 Hounsfield units, which correspond to severe emphysema, were obtained. The arithmetical mean value for each case was used as the representative value, LAA%.
Analysis of airways
A cross-section of the apical bronchus of the right upper lobe (rB1) was obtained on HRCT to assess airway thickness.20 Airway dimensions were measured using the method described in previous studies21, 22 with a modification. The cross-section of the right B1 bronchus, which appeared on the HRCT film was scanned, and the images were magnified 50 times for the following measurements. Both the inner and outer perimeters of rB1 were traced. The airway wall area (WA) was calculated as the area obtained with the outer perimeter of rB1 (total airway area) subtracted from both the dark plus intermediate areas (luminal area). The percentage of the airway wall area (WA%) was calculated using the formula 100 × WA/total airway area. Major and minor axes in the inner area of rB1 were determined on the enlarged, traced images, and the ratio of the major and minor axes was calculated; this ratio was the distortion index. The WA% was obtained only for cases with a distortion index >0.75, indicating the best circular shape of the rB1 cross-section. Analyses of all images on HRCT films were performed on a Macintosh computer using the public domain NIH Image programme (developed at the US National Institutes of Health and available on the Internet at http://rsb.info.nih.gov/nih-image/).
Depression score based on the hospital anxiety and depression scale (HADS)
Depression and anxiety were assessed at baseline, using HADS.23 HADS is a validated tool for screening for the severity of symptoms of depression and anxiety in both hospitalised and primary care patients24 with chronic diseases, including COPD,11 and in the general population.24 HADS comprises seven items for depression (HAD-D) and seven items for anxiety (HAD-A). The scores range from 0 to 21 for each subscale, with a score of 0–7 denoting a non-case; 8–10, a possible case; and 11 or higher, a probable case.23 This scale was translated into Japanese and has also been validated as a screening tool in Japan.25
Methods for genotyping
SNP selection
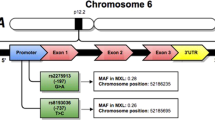
We selected SNPs of SLC6A4 based on information from Hapmap (http://www.hapmap.org) for a Japanese population, as shown in Supplementary Table 1 and Supplementary Figure 1. These SNPs were selected using a tagging algorithm in the Haploview 4.1 software (Whitehead Institute for Biomedical Research, http://www.broad.mit.edu/mpg/haploview). Haplotype blocks were defined according to Gabriel et al.,26 and tag SNPs were selected using an linkage disequilibrium threshold defined by r2⩾0.8 and a minor allele frequency ⩾0.10.
Genotyping assays
Genomic DNA was isolated from whole blood using the QIAamp DNA Blood Mini Kit, according to the manufacturer's protocol (Qiagen KK, Tokyo, Japan). The SNPs described above were genotyped using 5′ to 3′ exonuclease TaqMan assays27 with ABI TaqMan SNP Genotyping Assays (Life Technologies Japan, Tokyo, Japan).
Statistical analysis
All values are presented as means±standardized deviation (s.d.). The basic characteristics between two groups were compared using Fisher’s exact test and an unpaired t-test or a non-parametric test (Wilcoxon test). Statistical analyses were performed using JMP Genomics software, version 3.1 (SAS Institute, Cary, NC, USA). The analyses included testing Hardy–Weinberg equilibrium and the other genetic analyses that are described below.
We used multivariate logistic regression analysis to compare the COPD incidence among the genotypes tested (represented in the tables as genotype analyses) or in a trend model (an additive model in which the genotypes were coded as 0, 1 and 2 as per the number of minor alleles). The odds ratio of COPD development was also calculated according to the number of a specific risk allele in a trend model. The effect of each SNP genotype on continuous variables, including pulmonary function testing, quantitative computed tomography scan data, HADS score and pack-years, were analyzed using multivariate linear regression. Data were adjusted for age, gender and smoking status.
We implemented mediation analysis to identify the potential mediation effects of pack-years on the relation between rs2020936 and risk of COPD incidence.28 The significance of the indirect effect (mediating effect) is tested using the Sobel test, and the mediating effect is also calculated as previously described.29, 30, 31 In our study, because of the dichotomous outcome (COPD), the calculation had to be slightly modified as previously described.32, 33 Because the distribution of the pack-years was not normal, we had to apply box-cox transformation before initiating the mediation analysis.34 All regression analyses for the mediation analysis were adjusted for age and gender. The genetic variant (rs2020936) was coded assuming an additive model.
The expectation-maximisation algorithm was used to estimate the unobserved haplotype frequencies, given a multilocus sample of genetic marker genotypes under the assumption of Hardy–Weinberg equilibrium. The haplotypes for each subject were estimated. The effect of each haplotype on the formation of COPD or the continuous variables was determined via a logistic or linear regression analysis with a trend model adjusted for age, gender and smoking status.
P<0.05 was considered significant. Owing to the nature of the analysis and multiple testing of the dependent and independent variables, Bonferroni correction was applied.
Results
Tag SNP selection
We investigated the linkage disequilibrium block structure for SLC6A4 and its 5′ flanking sequence and selected 5 tag SNPs for SLC6A4. The 5 tag SNPs were considered to represent the genetic variations for the region and were used in this study (Supplementary Figure 1).
Relationship between SLC6A4 variation and tobacco consumption and COPD incidence
We found a significant correlation between COPD incidence and rs2020936 in the trend model (Table 2). rs2020936 was also associated with pack-years in the trend model before Bonferroni correction (Table 3). The number of T alleles of rs2020936 positively correlated with COPD and pack-years in a parallel manner (Figures 1 and 2), and the association between COPD and rs2020936 weakened after adjustment for pack-years (P-value adjusted for pack-years=0.006). Therefore, rs2020936 is thought to be associated with COPD, and this association is thought to depend partly on tobacco consumption. We also performed a mediation analysis to assess the mediating effect of pack-years on the relation between rs2020936 and COPD incidence. The Sobel test results showed that this mediating effect was significant (P=0.042), and that the pack-years contributed partly to the effect of the SNP on COPD (11.06%) (Supplementary Table 2). The odds ratio of the T allele for COPD was 2.20 (95% confidence interval, 1.31–3.74).
The difference in the proportion of COPD between SLC6A4 genotypes (rs2020936). Refer to Table 2 for the results of statistical analyses.
Comparison between the pack-years and the rs2020936 genotypes. The mean and s.d. values are represented in the bar graphs as error bars. The number of T alleles of rs2020936 showed a positive correlation with the number of pack-years (P=0.026). Refer to Table 3 for the results of statistical analyses.
There were significant differences in FEV1%predicted and %WA values between the rs2020936 genotypes (Table 3). These differences were also observed after the data were adjusted for pack-years (P=0.014 and 0.000, respectively). Further, five C-homozygotes for this SNP have significantly higher FEV1%predicted and lower %WA values than subjects with other genotypes (data not shown).
SLC6A4 variation and depressive symptoms
Another SNP of SLC6A4, rs3794808, significantly correlated with the depression score of HADS in a trend model of a whole population (Table 3) and also COPD subjects (P=0.022 for the trend model after adjustment) (Figure 3). This correlation was significant even after adjusting for FEV1% predicted values (P=0.019). The association between this SNP and the depression score was not significant after applying Bonferroni correction.
Comparison between the HADS depression score and the rs3794808 genotypes. The mean and s.d. values are shown in the bar graphs as error bars. All genotypes of rs3794808 significantly correlated with the HADS depression score in the trend model of the whole population (P=0.016) and also with the COPD incidence (P=0.022). Refer to Table 3 for the results of statistical analyses.
Relationship between SLC6A4 haplotypes and tobacco consumption, COPD or depressive symptoms
The haplotype rs3794808 G/rs140701 G/rs140700 G/rs2020939 C/rs2020936 T was correlated with the HADS depression score, and there were no haplotypes that correlated with COPD, pack-years and depression scores simultaneously, as shown in Supplementary Table 3.
Discussion
In this study, the SNP rs2020936 of SLC6A4 significantly correlated with COPD, and this SNP was also associated with pack-years. Another SNP of SLC6A4, rs3794808, significantly correlated with the HADS depression score. These results indicate that SLC6A4 variation affects COPD pathogenesis, and this effect depends partly on tobacco consumption. Further, SLC6A4 variation might also contribute to the depressive symptoms in COPD.
An association between SLC6A4 variation and smoking behaviour has been reported. However, this is the first report on an association between SLC6A4 SNPs and COPD. SLC6A4 is thought to be closely related to nicotine dependence4 and has been reported to be associated with smoking behaviour in the Japanese8 and Chinese.9 CYP2A6 and CHRNA 3/5 are believed to be candidate genes involved in COPD pathogenesis,5, 6 there are no reports on an association between SLC6A4 and COPD. In addition, we also showed the mediation effect of pack-years on the relationship between genetic variation of SLC6A4 and COPD, and to the best of our knowledge, this finding has been reported for the first time in the literature.
Since an SLC6A4 SNP also correlated with %WA after adjusting for pack-years, SLC6A4 is possibly associated with an aspect of airway disease in COPD. Although serotonin does not constrict the human airway smooth muscle in vitro, it increases acetylcholine release from airway nerves via 5HT3 and 5HT4 receptors.35 The activation of the serotoninergic receptors on human airway epithelial cells regulates the release of IL-6 and IL-8.36 SLC6A4 could play a role in the inflammatory responses of human airway epithelial cells in COPD subjects by changing the concentration of serotonin in the peripheral lungs.
We also observed an association between another SNP of SLC6A4 and depressive symptoms, which is consistent with previous reports. There are many reports on the association between depression and SLC6A4 variation,37 especially variation in the polymorphic region (LPR) and the 17-bp variable number of tandem repeats (VNTR) in the second intron. Although reports on the association between 5-HTTLPR and depression are inconsistent, LPR or VNTR could be the only ‘tags’ of the causal SNPs and could be responsible for the inconsistency. Since we found this correlation after adjusting for COPD severity (FEV1% predicted), SLC6A4 variation is believed to be associated with depressive symptoms, regardless of COPD severity.
Since genetic variations of SLC6A4 were associated with depressive symptoms and COPD, there is a possibility that modification of this enzyme could be an option for preventing COPD and treating its depressive symptoms. Selective serotonin reuptake inhibitors (SSRI) and nortriptyline, inhibitors or modifiers of SLC6A4, are now used as standard therapy for depression and the depressive symptoms in COPD.38 These drugs are also candidates for smoking cessation treatments.39 Thus, via their role smoking cessation, some types of SSRIs might be effective for treating both depressive symptoms and COPD.
This study had some limitations. First, the associations between the different variables, particularly the association between the SNPs and pack-years, were relatively weak, as revealed by the P-values obtained. This weak association might possibly be because of the relatively small sample size (247 COPD cases versus 119 controls). In future studies, we aim to determine this association using a larger population of other races. Second, the tag SNPs in our study were located in the intron. Fine mapping of the SNPs of SLC6A4 is needed to investigate the association between all the SNPs and phenotypes. Functional analyses (for example, mRNA expression study) of the causal SNPs should also be performed after they have been identified.
We conclude that SLC6A4 variation affects COPD pathogenesis, and this effect depends partly on tobacco consumption. SLC6A4 variation also affects depressive symptoms in COPD. Therapy for COPD in the future could be optimised to include treatments for smoking cessation and depression by taking SLC6A4 variation into consideration.
References
Murray, C. J. & Lopez, A. D. Evidence-based health policy—lessons from the global burden of disease study. Science 274, 740–743 (1996).
Fletcher, C. & Peto, R. The natural history of chronic airflow obstruction. Br. Med. J. 1, 1645–1648 (1977).
Silverman, E. K., Spira, A. & Pare, P. D. Genetics and genomics of chronic obstructive pulmonary disease. Proc. Am. Thorac. Soc. 6, 539–542 (2009).
Quaak, M., van Schayck, C. P., Knaapen, A. M. & van Schooten, F. J. Genetic variation as a predictor of smoking cessation success. A promising preventive and intervention tool for chronic respiratory diseases? Eur. Respir. J. 33, 468–480 (2009).
Minematsu, N., Nakamura, H., Iwata, M., Tateno, H., Nakajima, T., Takahashi, S. et al. Association of CYP2A6 deletion polymorphism with smoking habit and development of pulmonary emphysema. Thorax 58, 623–628 (2003).
Pillai, S. G., Ge, D., Zhu, G., Kong, X., Shianna, K. V., Need, A. C. et al. A genome-wide association study in chronic obstructive pulmonary disease (COPD): identification of two major susceptibility loci. PLoS. Genet. 5, e1000421 (2009).
Barnes, P. J. & Celli, B. R. Systemic manifestations and comorbidities of COPD. Eur. Respir. J. 33, 1165–1185 (2009).
Ishikawa, H., Ohtsuki, T., Ishiguro, H., Yamakawa-Kobayashi, K., Endo, K., Lin, Y. L. et al. Association between serotonin transporter gene polymorphism and smoking among Japanese males. Cancer Epidemiol. Biomarkers Prev. 8, 831–833 (1999).
Chu, S. L., Xiao, D., Wang., C. & Jing, H. Association between 5-hydroxytryptamine transporter gene-linked polymorphic region and smoking behavior in Chinese males. Chin. Med. J. (Engl) 122, 1365–1368 (2009).
Caspi, A., Sugden, K., Moffitt, T. E., Taylor, A., Craig, I. W., Harrington, H. et al. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science 301, 386–389 (2003).
Ng, T. P., Niti, M., Tan, W. C., Cao, Z., Ong, K. C. & Eng, P. Depressive symptoms and chronic obstructive pulmonary disease: Effect on mortality, hospital readmission, symptom burden, functional status, and quality of life. Arch. Intern. Med. 167, 60–67 (2007).
Xu, W., Collet, J. P., Shapiro, S., Lin, Y., Yang, T., Platt, R. W. et al. Independent effect of depression and anxiety on chronic obstructive pulmonary disease exacerbations and hospitalizations. Am. J. Respir. Crit. Care Med. 178, 913–920 (2008).
Kendler, K. S., Neale, M. C., MacLean, C. J., Heath, A. C., Eaves, L. J. & Kessler, R. C. Smoking and major depression. A causal analysis. Arch. Gen. Psychiatry 50, 36–43 (1993).
Global strategy for diagnosis, management, and prevention of COPD, http://www.goldcopd.com/ (accessed 13 April 2009).
Vestbo, J. & Lange, P. Can GOLD Stage 0 provide information of prognostic value in chronic obstructive pulmonary disease? Am. J. Respir. Crit. Care Med. 166, 329–332 (2002).
Standardization of spirometry, 1994 update. American Thoracic Society. Am. J. Respir. Crit. Care Med. 152, 1107–1136 (1995).
Japanese Respiratory Society. The predicted values of spirometry and arterial blood gas analysis in Japanese. J. Jap. Resp. Soc. 39, Appendix (2001) (in Japanese).
Motohashi, N., Kimura, K., Ishii, T., Wakabayashi, R., Kurosaki, H., Motegi, T. et al. Emphysema on imaging is associated with quality of life in elderly patients with chronic obstructive pulmonary disease. Geriatr. Gerontol. Int. 10, 17–24 (2010).
Nakano, Y., Muro, S., Sakai, H., Hirai, T., Chin, K., Tsukino, M. et al. Computed tomographic measurements of airway dimensions and emphysema in smokers. Correlation with lung function. Am. J. Respir. Crit. Care Med. 162, 1102–1108 (2000).
Nakano, Y., Muller, N. L., King, G. G., Niimi, A., Kalloger, S. E., Mishima, M. et al. Quantitative assessment of airway remodeling using high-resolution ct. Chest 122, 271S–275S (2002).
Okazawa, M., Muller, N., McNamara, A. E., Child, S., Verburgt, L. & Pare, P. D. Human airway narrowing measured using high resolution computed tomography. Am. J. Respir. Crit. Care Med. 154, 1557–1562 (1996).
Orlandi, I., Moroni, C., Camiciottoli, G., Bartolucci, M., Pistolesi, M., Villari, N. et al. Chronic obstructive pulmonary disease: thin-section ct measurement of airway wall thickness and lung attenuation. Radiology 234, 604–610 (2005).
Zigmond, A. S. & Snaith, R. P. The hospital anxiety and depression scale. Acta. Psychiatr. Scand. 67, 361–370 (1983).
Bjelland, I., Dahl, A. A., Haug, T. T. & Neckelmann, D. The validity of the hospital anxiety and depression scale. An updated literature review. J. Psychosom. Res. 52, 69–77 (2002).
Higashi, A., Yashiro, H., Kiyota, K., Inokuchi, H., Hatta, H., Fujita, K. et al. Validation of the hospital anxiety and depression scale in a gastro-intestinal clinic. Nippon Shokakibyo Gakkai Zasshi 93, 884–892 (1996).
Gabriel, S. B., Schaffner, S. F., Nguyen, H., Moore, J. M., Roy, J., Blumenstiel, B. et al. The structure of haplotype blocks in the human genome. Science 296, 2225–2229 (2002).
Holland, P. M., Abramson, R. D., Watson, R. & Gelfand, D. H. Detection of specific polymerase chain reaction product by utilizing the 5′–3′ exonuclease activity of thermus aquaticus DNA polymerase. Proc. Natl. Acad. Sci. USA 88, 7276–7280 (1991).
Baron, R.M. & Kenny, D.A. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol. 51, 1173–1182 (1986).
Kenny, D.A. Mediation. Available at: http://davidakenny.net/cm/mediate.htm (Accessed September 8, 2010).
Sobel, M.E. Asymptotic confidence intervals for indirect effects in structural equation models. in Sociological Methodology (ed, Leinhart S). Vol. 13, 290–312 (Jossey-Bass, San Francisco, 1982).
Preacher,, K. J. Calculation for the Sobel test. Available at: http://www.people.ku.edu/~preacher/sobel/sobel.htm (Accessed September 8, 2010).
Herr, N. R. Mediation with dichotomous outcomes Available at: http://nrherr.bol.ucla.edu/Mediation/logmed.html (Accessed September 8, 2010).
MacKinnon, D. P. & Dwyer, J. H. Estimating mediated effects in prevention studies. Evaluation Rev. 17, 144–158 (1993).
Wang, J., Spitz, M. R., Christopher, I., Amos, C.I., Wilkinson, A. V., Wu, X . et al. Mediating effects of smoking and chronic obstructive pulmonary disease on the relation between the CHRNA5-A3 genetic locus and lung cancer risk. Cancer 116, 3458–3462 (2010).
Barnes, P. J. Histamine and serotonin. Pulm. Pharmacol. Ther. 14, 329–339 (2001).
Bayer, H., Muller, T., Myrtek, D., Sorichter, S., Ziegenhagen, M., Norgauer, J. et al. Serotoninergic receptors on human airway epithelial cells. Am. J. Respir. Cell Mol. Biol. 36, 85–93 (2007).
Risch, N., Herrell, R., Lehner, T., Liang, K. Y., Eaves, L., Hoh, J. et al. Interaction between the serotonin transporter gene (5-httlpr), stressful life events, and risk of depression: A meta-analysis. JAMA 301, 2462–2471 (2009).
Hill, K., Geist, R., Goldstein, R. S. & Lacasse, Y. Anxiety and depression in end-stage COPD. Eur. Respir. J. 31, 667–677 (2008).
Hughes, J. R., Stead, L. F. & Lancaster, T. Antidepressants for smoking cessation. Cochrane Database Syst. Rev. 1, CD000031 (2007).
Acknowledgements
We sincerely thank Ms Fujishiro for her help in our research. We also acknowledge the help provided by Dr Motohashi N, Dr Morii K, Dr Hattori K, Dr Yamada K and Dr Motegi T in sample collection. This study was partly supported by a grant from the Grant-in-Aid for Young Scientists (B) from the Ministry of Education, Science, Sports and Culture, Japan.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supplementary Information accompanies the paper on Journal of Human Genetics website
Rights and permissions
About this article
Cite this article
Ishii, T., Wakabayashi, R., Kurosaki, H. et al. Association of serotonin transporter gene variation with smoking, chronic obstructive pulmonary disease, and its depressive symptoms. J Hum Genet 56, 41–46 (2011). https://doi.org/10.1038/jhg.2010.133
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhg.2010.133
Keywords
This article is cited by
-
Cigarette Smoking and Psychiatric Illness Among Individuals with COPD: a Systematic Review
Current Addiction Reports (2024)
-
Circulating serotonin levels in COPD patients: a pilot study
BMC Pulmonary Medicine (2018)
-
Genetic scores of smoking behaviour in a Chinese population
Scientific Reports (2016)
-
SLC6A4STin2 VNTR genetic polymorphism is associated with tobacco use disorder, but not with successful smoking cessation or smoking characteristics: a case control study
BMC Genetics (2014)
-
PDE4: A Novel Target in the Treatment of Chronic Obstructive Pulmonary Disease
Clinical Pharmacology & Therapeutics (2012)