Abstract
Patients with type 2 diabetes mellitus (DM) exhibit modification of high-density lipoprotein (HDL), which is likely to have an important role in the development of atherosclerotic cardiovascular disease (ASCVD). Excess production of aldosterone (Ald) results in hypertension as well as ASCVD. However, the biological activity of modified HDL in steroidogenesis is not clear. We measured the accumulation of thiobarbituric acid-reactive substances (TBARSs) and Nɛ-(carboxymethyl)lysine (CML) levels (markers of oxidation and glycoxidation, respectively) in isolated HDL from 41 patients with type 2 diabetes mellitus (DM group) and 41 age- and gender-matched patients in a non-DM group. We quantified angiotensin II-sensitized and -nonsensitized Ald release using a validated living adrenocortical cell assay. TBARS levels in isolated HDL were similar between patients in the DM and non-DM groups, whereas the CML content of HDL in the DM group was lower than that in the non-DM group, irrespective of higher blood glucose and hemoglobin A1c levels. There was no difference in the HDL-induced ex vivo Ald release between the groups. Although sustained hyperglycemia was not a determinant of HDL-induced Ald release, the degree of HDL glycoxidation was inversely associated with HDL-induced Ald release (r=−0.40, P<0.001). In conclusion, in vivo advanced glycoxidation of HDL had an inverse effect on HDL-induced Ald release, independent of the prevalence of type 2 DM.
Similar content being viewed by others
Introduction
Atherosclerotic cardiovascular disease is a major cause of morbidity and mortality for patients with type 2 diabetes mellitus (DM). An epidemiological study revealed that the development of atherosclerotic cardiovascular disease in diabetes is due in part to its association with atherogenic dyslipidemia, which is characterized by high low-density lipoprotein (LDL) cholesterol and triglyceride (TG) levels and low high-density lipoprotein (HDL) cholesterol.1 Therefore, HDL cholesterol levels are among the most widely measured biomarkers in clinical practice.2 However, some pharmacological clinical interventions to raise HDL cholesterol, including the cholesteryl ester transfer protein inhibitor torcetrapib, have failed to demonstrate clinical benefits.3 In addition, a Mendelian randomization study revealed that common variants that increase HDL cholesterol levels are not associated with protection against cardiovascular disease.4 These recent findings have raised the question of whether raising HDL cholesterol is a valid therapeutic target and have reinforced efforts to focus on ‘HDL quality.’
One of the most well-established anti-atherogenic mechanisms of HDL is based on its ability to promote cholesterol efflux from peripheral tissues and transport cholesterol to the liver for excretion into bile, a process known as reverse cholesterol transport.5 It is well known that HDL also has antioxidant, anti-inflammatory and vasodilatory properties.6, 7 Furthermore, it has been suggested that HDL is the preferred lipoprotein for cholesterol delivery to steroid-producing tissues.8 A recent clinical genetic study found that a variation in the SCARB1 gene, which encodes the HDL receptor scavenger type B class I (SR-BI), is associated with adrenal steroidogenesis.9 Aldosterone (Ald) is a mineralocorticoid hormone synthesized in the adrenal cortex, and increased Ald production and augmented signaling through the mineralocorticoid receptor are keys to the pathogenesis of hypertension (HTN)10 and chronic kidney disease.11, 12 Interestingly, mice lacking SR-BI exhibit adrenal insufficiency under stress and show severe atherosclerosis despite having high plasma HDL cholesterol levels.13, 14 These findings indicate a possible pathophysiological link between lipoproteins and the development of HTN, another risk factor for atherosclerotic cardiovascular disease in diabetic patients.
Modification of HDL also influences the functionality of HDL. The most common abnormal HDL composition in type 2 DM is characterized by enrichment of TG with cholesteryl ester depletion, which may reflect increased cholesteryl ester transfer protein activity and reduced hepatic lipase activity.15 Indeed, TG-enriched HDL from DM patients has been shown to have impaired antioxidative properties.16 Other qualitative abnormalities of HDL include oxidation and glycation. Persistent hyperglycemia and oxidative stress in DM are believed to be important. Several studies have investigated the biological activities of these HDL modifications, and glycated/glycoxidized HDL was generally considered dysfunctional because it was associated with decreased cholesterol efflux capacity17 and impaired anti-inflammatory and anti-apoptotic activity.18, 19 Although little is known about the functional attributes of modified HDL in steroidogenesis, Saha et al.20 recently demonstrated that native HDL increased Ald release from angiotensin II (Ang II)-sensitized human adrenocortical cells. Moreover, both oxidized HDL and glycoxidized HDL induced Ald release at levels several-fold higher than for native HDL. These findings were based on in vitro HDL modifications, and it is unclear whether HDL modified in vivo has similar functionality. Furthermore, the contribution of DM to HDL modification in patients is poorly understood.
Therefore, the purpose of this study was to investigate whether patients with type 2 DM have in vivo HDL modifications. In addition, we assessed the effects of in vivo HDL oxidation and glycoxidation on Ald release to explore the pathophysiological link between HDL modification and adrenocortical hormone release.
Methods
Study population
We enrolled 41 consecutive outpatients at Fukuoka University Hospital who had type 2 DM (DM group). In addition, 41 age- and gender-matched patients without type 2 DM were selected as a non-DM group. Type 2 DM patients either had a known history of type 2 DM with or without anti-DM therapy or met the criteria for a diagnosis of type 2 DM. The protocol in this study was approved by the ethics committee of Fukuoka University Hospital, and all patients gave their written informed consent to participate.
Evaluation of clinical parameters
In all patients, body mass index and office systolic and diastolic blood pressure were measured at the time of enrollment. The characteristics of patients with regard to history of smoking, DM, HTN, dyslipidemia and medication use were obtained from medical records.
Blood samples
Venous blood samples were drawn from all study participants at least 5 h after a meal. Concentrations of random blood glucose, hemoglobin A1c (HbA1c), total cholesterol, LDL cholesterol, HDL cholesterol, TG, creatinine, plasma aldosterone concentration and high-sensitivity C-reactive protein were measured by enzymatic methods on an autoanalyzer. The concentrations of plasma adiponectin were determined in duplicate by specific enzyme immunoassays (R&D Systems, Minneapolis, MN, USA) according to the manufacturer’s instructions.
HDL isolation by ultracentrifugation
Whole blood from each patient was collected into tubes at 4 °C containing 0.1% EDTA at pH 7.4. Plasma was separated by centrifugation and collected immediately at 4 °C. HDL (1.063<d<1.21 g ml−1) was purified by standard sequential density gradient ultracentrifugation.21 In brief, plasma was centrifuged at 150 000 g for 48 h at 4 °C using sequential densities of 1.063 and 1.21 g ml−1 to isolate HDL. The sample density was adjusted with the addition of KBr. The HDL fraction was collected by tube slicing and dialyzed against phosphate-buffered saline. The protein concentration was quantified with a bicinchoninic acid assay utilizing a commercial reagent (Pierce Chemical, Rockland, IL, USA). Next, purified HDL was filter-sterilized and stored at 4 °C before use in the experiments.
HDL biochemical characterization
Measurement of the glycoxidation of isolated HDL was performed by determining the Nɛ-(carboxymethyl)lysine (CML) levels with a specific ELISA kit (Cell Biolabs, San Diego, CA, USA). The immunoassay was used according to the manufacturer’s instructions. Briefly, isolated HDL (50 μl of 100 mg protein per l) was added to the wells with CML-bovine serum albumin (BSA) and anti-CML monoclonal antibodies for 1 h at 37 °C. After washing the wells with wash buffer, horseradish peroxidase-conjugated secondary antibody was incubated in the wells for 1 h. Finally, the optical density was read at 450 nm after adding substrate solution. The oxidative change in HDL was measured with a commercial kit to quantify the lipid peroxidation (thiobarbituric acid-reactive substance (TBARS) assay kit, Cayman Chemical, Ann Arbor, MI, USA) according to the manufacturer’s instructions. Isolated HDL (100 μl of 100 mg protein per l) was added on malondialdehyde and thiobarbituric acid; then, samples were boiled for 1 h. The supernatant absorbance was colorimetrically read at 530 nm.
Cell culture
Human adrenocortical cells (NCI-H295R, American Type Culture Collection CRL-10296) (American Type Culture Collection, Manassas, VA, USA) were cultured in DMEM-F12 medium (Wako Chemicals, Osaka, Japan) supplemented with 10% fetal bovine serum (Nu-Serum; BD Biosciences, Baltimore, MD, USA) and 1% penicillin and streptomycin in a humidified incubator with 5% CO2 at 37 °C. For the experiment, cells were counted and dispensed into 12-well culture plates at a density of 1 × 105 cells per well. Cells grown to semi-confluence were used for the following experiment.
Measurement of Ald release
The level of Ald release was determined with an enzyme immune assay and culture medium as described previously.22 Ang II-sensitized and non-sensitized H295R cells were cultured for 24 h with or without Ang II (10−7 M) (Peptide Institute Inc., Osaka, Japan), respectively. After washout of the cells, the remaining cells in DMEM-F12 were incubated with isolated HDL (100 μg protein per ml) under DMEM-F12 serum-free conditions for 24 h. Conditioned medium was collected, and Ald concentrations were measured in duplicate using an Ald ELISA assay kit (Cayman Chemical).
Statistical analysis
Statistical analysis was performed using SAS software, version 9.4 (SAS Institute, Cary, NC, USA) at Fukuoka University. Values are presented as percentages, means and s.d. Categorical and continuous variables were compared between two groups by a χ2 analysis and unpaired t-test, respectively. The correlation with Ald release was assessed using Pearson correlation coefficients. In addition, multivariate regression analysis was performed with three different models (Model 1: adjustment for age, gender and body mass index; Model 2: adjustment for Model 1 factors and HbA1c; Model 3: adjustment for Model 2 factors and total cholesterol, LDL cholesterol, HDL cholesterol, TG and TBARS of isolated HDL) to verify the independent correlation between Ald release and the CML levels in isolated HDL from patients. A P-value <0.05 was considered significant.
Results
Patient characteristics
The characteristics of the 82 patients are shown in Table 1. The mean age of all patients was 66±10 years. The mean values for the random blood glucose and HbA1c in the DM group were 134 mg dl−1 and 6.6%, respectively, and these were significantly higher than those in the non-DM group. Although both groups showed a high prevalence of HTN and dyslipidemia, most patients were well controlled, and the mean systolic blood pressure and LDL cholesterol levels were 131 mm Hg and 111 mg dl−1, respectively. There were no statistically significant differences between the groups with respect to plasma aldosterone concentration or high-sensitivity C-reactive protein. Adiponectin is the most abundant adipokine, and circulating adiponectin is known to be inversely related to body weight and insulin resistance.23 The DM patients tended to have higher body mass index and lower adiponectin levels than non-DM patients, albeit these differences were not significant (P=0.059 and 0.096, respectively). Insulin and oral hypoglycemic agents were prescribed to 17 and 60% of the diabetic patients, respectively. Approximately half of all patients were taking an angiotensin-converting enzyme inhibitor (ACE-I) or an Ang-II receptor blocker (ARB), and one-third of the patients were taking statin drugs.
Less glycoxidation occurred in HDL isolated from DM patients
To assess in vivo oxidation and glycoxidation, we measured the TBARS and CML levels in isolated HDL in the DM and non-DM groups. No statistically significant differences were observed in the TBARS levels of isolated HDL between the groups (Figure 1a). Therefore, we further compared the TBARS-HDL levels between patients with poor (HbA1c⩾7.0%) and good glycemic control (HbA1c<7.0%) (Supplementary Table 2). There was no difference in the average TBARS-HDL level between the groups (57.2±21.6 vs. 50.3±22.3 μmol per g protein; P=0.34; Supplementary Figure 2). On the other hand, although the plasma CML levels in the two groups were similar, the CML level in HDL from DM patients was significantly lower than that in non-DM patients (1.2 vs. 1.8 ng per mg protein; P=0.014; Figure 1b). It is thought that ACE-I/ARB and statin therapy can affect in vivo glycoxidation. Thus, we compared the effects of ACE-I/ARB and statin on the CML levels in isolated HDL from all subjects. Neither ACE-I/ARB use nor statin use affected the CML levels in isolated HDL (Supplementary Figure 1). To exclude the possibility that these medications work differently in the presence or absence of diabetes, we further divided the patients into two groups according to the presence of diabetes (Supplementary Table 1). Except for those who had received either an ACE-I/ARB or statin, diabetic patients tended to have low CML levels in isolated HDL, regardless of their medications.
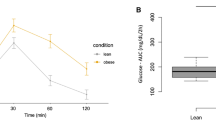
DM did not affect the rate of aldosterone release by isolated HDL in Ang II-sensitized cells
We compared Ald release with isolated HDL in Ang II (10−7 M)-sensitized NCI-H295R cells with or without DM (Figure 2). The Ang II-sensitized condition was associated with a significant increase in Ald release in both groups. The effects of isolated HDL from DM patients on Ald release in H295R cells were similar to those of HDL from the non-DM group, regardless of Ang II induction.
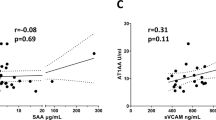
Correlation analysis for Ang II-induced Ald release by isolated HDL in all patients
We analyzed factors that influenced Ang II (10−7 M)-sensitized Ald release with isolated HDL in H295R cells for all patients. While Ald is a sodium-retaining pro-hypertensive hormone and elevated levels would typically be associated with HTN, the systolic blood pressure and plasma aldosterone concentration levels were not correlated with the aldosterone release in this study (Table 2). Remarkably, glycoxidized-HDL levels, as indicated by CML concentrations in isolated HDL, were significantly and negatively correlated with Ald release (r=−0.40, P<0.001; Figure 3). Oxidized-HDL levels, as determined by the TBARS assay for isolated HDL, did not show a significant correlation (r=0.14, P=0.234). In addition, multivariate regression analysis with three different models revealed that glycoxidized-HDL levels were independently associated with Ang II-sensitized Ald release by isolated HDL in H295R cells (Table 3).
Discussion
In the present study, we investigated whether the diabetic condition influenced HDL-induced steroidogenesis in adrenocortical cells. We found that isolated HDL from DM patients had a capacity for Ald release in a living human adrenocortical cell assay that was similar to that of HDL from non-diabetics. Although neither glucose nor HbA1c levels were correlated with the rate of ex vivo Ald release, the concentration of advanced glycation end products (AGEs) with isolated HDL was the only determinant of HDL-induced Ald release. To the best of our knowledge, this is the first report to reveal a functional relationship between in vivo HDL modification and Ald release.
AGEs are formed on proteins and lipids by non-enzymatic glycation and oxidation, and CML is one of the major antigenic structures of AGEs.24 AGEs are found in both long-lived and short-lived molecules, including apolipoproteins and lipids of lipoproteins.25 We measured the CML levels of isolated HDL from patients, and our regression analysis demonstrated that CML-HDL is negatively associated with Ang II-sensitized Ald release. A multivariate analysis revealed that, although this correlation was modest, it was stronger than those for any other variables, including other lipid parameters and markers for atherosclerotic cardiovascular disease (for example, high-sensitivity C-reactive protein and adiponectin).
SR-BI was originally identified as an HDL receptor in the liver, adrenals and ovaries.26, 27 Ohgami et al.28 demonstrated that SR-BI also serves as a receptor for AGEs. In addition, they showed that AGE-albumin inhibits both the SR-BI-mediated selective uptake of HDL cholesteryl esters and cellular cholesterol efflux to HDL, indicating that AGE proteins could modulate SR-BI-mediated cholesterol metabolism. Their observations are in line with our finding of an inverse relationship between the levels of CML-HDL and Ald release, and it is possible that AGE-HDL causes less aldosterone release as a result of inhibiting cholesterol uptake in the adrenals via the SR-BI pathway. Further studies will be needed to confirm this hypothesis.
Meanwhile, a recent report demonstrated that artificially oxidized or glycoxidized HDL augmented aldosterone release more than native HDL in a similar assay,20 which conflicts with the results of the present study. In vitro glycoxidized HDL was generally prepared by incubating isolated HDL with excessively high glucose concentrations (25–200 mM) for several days, and glycoxidized HDL is not a single defined entity but, rather, represents a spectrum of varying contents that could affect its biological activities. Thus, glycoxidized HDL might unexpectedly have nonphysiological properties.
We also compared oxidative and glycoxidative markers of HDL from patients with and without diabetes. Despite the higher random blood glucose levels and HbA1c values, the prevalence of DM did not alter TBARS levels of isolated HDL, representing HDL oxidation. Moreover, in vivo HDL glycoxidation, as indicated by CML-HDL, was decreased in the DM group of this study, and the group also had similar plasma CML levels. In fact, although it has generally been considered that sustained hyperglycemia and oxidative stress in diabetic patients facilitate AGE formation, recent large-scale prospective cohort studies did not reveal an association between plasma CML levels and the diabetic condition.29, 30 Other independent reports have shown that plasma CML levels are not related to the CML-HDL levels in diabetic patients.19, 31 Rabbani et al.25 also reported that isolated LDL from DM patients had significantly higher concentrations of arginine-derived AGEs, such as carboxymethyl-arginine, but the levels of lysine-derived AGEs, including CML, were similar to those in LDL from non-diabetics. Pentosidine, another well-characterized AGE, forms crosslinks between arginine and lysine residues during glycoxidation. Interestingly, unlike decreased CML-HDL in the DM group, pentosidine levels in isolated HDL were similar between the groups in our study (data not shown). Therefore, our observation that hyperglycemia decreased CML in HDL, but not pentosidine, indicates that lysine-derived AGEs are less susceptible to glycoxidation by hyperglycemia on HDL, in the same manner as LDL glycoxidation.
There are several limitations of this study. First, we isolated HDL from human plasma by ultracentrifugation to obtain purified HDL. However, there is some concern about utilizing ultracentrifugation for HDL isolation in high-salt media containing KBr because the salt might cause dissociation of some associated proteins from the HDL surface. Second, although our regression analysis demonstrated a significant correlation between CML-HDL and ex vivo Ald release, it is difficult to determine the clinical impact of glycoxidative modification of HDL on aldosterone release in vivo. Because we measured only the CML in isolated HDL, the other glycation products, including methylglyoxal and 3-dexoyglucosonemethyl, might have different roles in aldosterone release. Further study is needed to address this issue.
In conclusion, the current study showed that isolated HDL from diabetic patients had HDL biological activity on aldosterone release in human adrenocortical cells that was similar to that in non-DM patients. However, based on in vivo HDL glycoxidation, the CML levels of HDL were, to a lesser extent, inversely related to Ald release. Thus, pathological glycoxidation of circulating HDL might contribute to the development of atherosclerotic disease.
References
Haffner SM . Diabetes, hyperlipidemia, and coronary artery disease. Am J Cardiol 1999; 83: 17F–21F.
Lewington S, Whitlock G, Clarke R, Sherliker P, Emberson J, Halsey J, Qizilbash N, Peto R, Collins R . Blood cholesterol and vascular mortality by age, sex, and blood pressure: a meta-analysis of individual data from 61 prospective studies with 55000 vascular deaths. Lancet 2007; 370: 1829–1839.
Barter PJ, Caulfield M, Eriksson M, Grundy SM, Kastelein JJ, Komajda M, Lopez-Sendon J, Mosca L, Tardif JC, Waters DD, Shear CL, Revkin JH, Buhr KA, Fisher MR, Tall AR, Brewer B, ILLUMINATE Investigators. Effects of torcetrapib in patients at high risk for coronary events. N Engl J Med 2007; 357: 2109–2122.
Voight BF, Peloso GM, Orho-Melander M, Frikke-Schmidt R, Barbalic M, Jensen MK, Hindy G, Hólm H, Ding EL, Johnson T, Schunkert H, Samani NJ, Clarke R, Hopewell JC, Thompson JF, Li M, Thorleifsson G, Newton-Cheh C, Musunuru K, Pirruccello JP, Saleheen D, Chen L, Stewart A, Schillert A, Thorsteinsdottir U, Thorgeirsson G, Anand S, Engert JC, Morgan T, Spertus J, Stoll M, Berger K, Martinelli N, Girelli D, McKeown PP, Patterson CC, Epstein SE, Devaney J, Burnett MS, Mooser V, Ripatti S, Surakka I, Nieminen MS, Sinisalo J, Lokki ML, Perola M, Havulinna A, de Faire U, Gigante B, Ingelsson E, Zeller T, Wild P, de Bakker PI, Klungel OH, Maitland-van der Zee AH, Peters BJ, de Boer A, Grobbee DE, Kamphuisen PW, Deneer VH, Elbers CC, Onland-Moret NC, Hofker MH, Wijmenga C, Verschuren WM, Boer JM, van der Schouw YT, Rasheed A, Frossard P, Demissie S, Willer C, Do R, Ordovas JM, Abecasis GR, Boehnke M, Mohlke KL, Daly MJ, Guiducci C, Burtt NP, Surti A, Gonzalez E, Purcell S, Gabriel S, Marrugat J, Peden J, Erdmann J, Diemert P, Willenborg C, König IR, Fischer M, Hengstenberg C, Ziegler A, Buysschaert I, Lambrechts D, Van de Werf F, Fox KA, El Mokhtari NE, Rubin D, Schrezenmeir J, Schreiber S, Schäfer A, Danesh J, Blankenberg S, Roberts R, McPherson R, Watkins H, Hall AS, Overvad K, Rimm E, Boerwinkle E, Tybjaerg-Hansen A, Cupples LA, Reilly MP, Melander O, Mannucci PM, Ardissino D, Siscovick D, Elosua R, Stefansson K, O'Donnell CJ, Salomaa V, Rader DJ, Peltonen L, Schwartz SM, Altshuler D, Kathiresan S . Plasma HDL cholesterol and risk of myocardial infarction: a Mendelian randomisation study. Lancet 2012; 380: 572–580.
Fielding CJ, Fielding PE . Molecular physiology of reverse cholesterol transport. J Lipid Res 1995; 36: 211–228.
Navab M, Reddy ST, Van Lenten BJ, Fogelman AM . HDL and cardiovascular disease: atherogenic and atheroprotective mechanisms. Nat Rev Cardiol 2011; 8: 222–232.
Soran H, Hama S, Yadav R, Durrington PN . HDL functionality. Curr Opin Lipidol 2012; 23: 353–366.
Azhar S, Reaven E . Scavenger receptor class BI and selective cholesteryl ester uptake: partners in the regulation of steroidogenesis. Mol Cell Endocrinol 2002; 195: 1–26.
Vergeer M, Korporaal SJ, Franssen R, Meurs I, Out R, Hovingh GK, Hoekstra M, Sierts JA, Dallinga-Thie GM, Motazacker MM, Holleboom AG, Van Berkel TJ, Kastelein JJ, Van Eck M, Kuivenhoven JA . Genetic variant of the scavenger receptor BI in humans. N Engl J Med 2011; 364: 136–145.
Williams JS, Williams GH . 50th anniversary of aldosterone. J Clin Endocrinol Metab 2003; 88: 2364–2372.
Mulè G, Nardi E, Guarino L, Cacciatore V, Geraci G, Calcaterra I, Oddo B, Vaccaro F, Cottone S . Plasma aldosterone and its relationship with left ventricular mass in hypertensive patients with early-stage chronic kidney disease. Hypertens Res 2015; 38: 276–283.
Sato A . The necessity and effectiveness of mineralocorticoid receptor antagonist in the treatment of diabetic nephropathy. Hypertens Res 2015; 38: 367–374.
Trigatti B, Rayburn H, Viñals M, Braun A, Miettinen H, Penman M, Hertz M, Schrenzel M, Amigo L, Rigotti A, Krieger M . Influence of the high density lipoprotein receptor SR-BI on reproductive and cardiovascular pathophysiology. Proc Natl Acad Sci USA 1999; 96: 9322–9327.
Hoekstra M, Meurs I, Koenders M, Out R, Hildebrand RB, Kruijt JK, Van Eck M, Van Berkel TJ . Absence of HDL cholesteryl ester uptake in mice via SR-BI impairs an adequate adrenal glucocorticoid-mediated stress response to fasting. J Lipid Res 2008; 49: 738–745.
Lewis GF, Rader DJ . New insights into the regulation of HDL metabolism and reverse cholesterol transport. Circ Res 2005; 96: 1221–1232.
Gowri MS, Van der Westhuyzen DR, Bridges SR, Anderson JW . Decreased protection by HDL from poorly controlled type 2 diabetic subjects against LDL oxidation may Be due to the abnormal composition of HDL. Arterioscler Thromb Vasc Biol 1999; 19: 2226–2233.
Duell PB, Oram JF, Bierman EL . Nonenzymatic glycosylation of HDL and impaired HDL-receptor-mediated cholesterol efflux. Diabetes 1991; 40: 377–384.
Hoang A, Murphy AJ, Coughlan MT, Thomas MC, Forbes JM, O'Brien R, Cooper ME, Chin-Dusting JP, Sviridov D . Advanced glycation of apolipoprotein A-I impairs its anti-atherogenic properties. Diabetologia 2007; 50: 1770–1779.
Matsunaga T, Iguchi K, Nakajima T, Koyama I, Miyazaki T, Inoue I, Kawai S, Katayama S, Hirano K, Hokari S, Komoda T . Glycated high-density lipoprotein induces apoptosis of endothelial cells via a mitochondrial dysfunction. Biochem Biophys Res Commun 2001; 287: 714–720.
Saha S, Graessler J, Schwarz PE, Goettsch C, Bornstein SR, Kopprasch S . Modified high-density lipoprotein modulates aldosterone release through scavenger receptors via extra cellular signal-regulated kinase and Janus kinase-dependent pathways. Mol Cell Biochem 2012; 366: 1–10.
Havel RJ, Eder HA, Bragdon JH . The distribution and chemical composition of ultracentrifugally separated lipoprotein in human serum. J Clin Invest 2015; 34: 1345–1353.
Miura S, Nakayama A, Tomita S, Matsuo Y, Suematsu Y, Saku K . Comparison of aldosterone synthesis in adrenal cells, effect of various AT receptor blockers with or without atrial natriuretic peptide. Clin Exp Hypertens 2015; 37: 353–357.
Matsuzawa Y, Funahashi T, Kihara S, Shimomura I . Adiponectin and metabolic syndrome. Arterioscler Thromb Vasc Biol 2004; 24: 29–33.
Reddy S, Bichler J, Wells-Knecht KJ, Thorpe SR, Baynes JW . N epsilon-(carboxymethyl)lysine is a dominant advanced glycation end product (AGE) antigen in tissue proteins. Biochemistry 1995; 34: 10872–10878.
Rabbani N, Chittari MV, Bodmer CW, Zehnder D, Ceriello A, Thornalley PJ . Increased glycation and oxidative damage to apolipoprotein B100 of LDL cholesterol in patients with type 2 diabetes and effect of metformin. Diabetes 2010; 59: 1038–1045.
Glass C, Pittman RC, Weinstein DB, Steinberg D . Dissociation of tissue uptake of cholesterol ester from that of apoprotein A-I of rat plasma high density lipoprotein: selective delivery of cholesterol ester to liver, adrenal, and gonad. Proc Natl Acad Sci USA 1983; 80: 5435–5439.
Acton S, Rigotti A, Landschulz KT, Xu S, Hobbs HH, Krieger M . Identification of scavenger receptor SR-BI as a high density lipoprotein receptor. Science 1996; 271: 518–520.
Ohgami N, Nagai R, Miyazaki A, Ikemoto M, Arai H, Horiuchi S, Nakayama H . Scavenger receptor class B type I-mediated reverse cholesterol transport is inhibited by advanced glycation end products. J Biol Chem 2001; 276: 13348–13355.
Hanssen NM, Engelen L, Ferreira I, Scheijen JL, Huijberts MS, van Greevenbroek MM, van der Kallen CJ, Dekker JM, Nijpels G, Stehouwer CD, Schalkwijk CG . Plasma levels of advanced glycation endoproducts Nɛ-(carboxymethyl)lysine, Nɛ-(carboxyethyl)lysine, and pentosidine are not independently associated with cardiovascular disease in individuals with or without type 2 diabetes: the Hoorn and CODAM studies. J Clin Endocrinol Metab 2013; 98: 1369–1373.
Hanssen NM, Beulens JW, van Dieren S, Scheijen JL, van der A DL, Spijkerman AM, van der Schouw YT, Stehouwer CD, Schalkwijk CG . Plasma advanced glycation end products are associated with incident cardiovascular events in individuals with type 2 diabetes: a case-cohort study with a median follow-up of 10 years (EPIC-NL). Diabetes 2015; 64: 257–265.
Low H, Hoang A, Forbes J, Thomas M, Lyons JG, Nestel P, Bach LA, Sviridov D . Advanced glycation end-products (AGEs) and functionality of reverse cholesterol transport in patients with type 2 diabetes and in mouse models. Diabetologia 2012; 55: 2513–2521.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
KS is the Chief Director and SM is the Director of NPO Clinical and Applied Science, Fukuoka, Japan. KS has Endowed Department of Molecular Cardiovascular Therapeutics funding supported by MSD. SM belongs to the Department of Molecular Cardiovascular Therapeutics, which is supported by MSD. The remaining authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Hypertension Research website
Supplementary information
Rights and permissions
About this article
Cite this article
Kuwano, T., Miura, Si., Norimatsu, K. et al. Advanced glycation of high-density lipoprotein and the functionality of aldosterone release in type 2 diabetes. Hypertens Res 40, 271–276 (2017). https://doi.org/10.1038/hr.2016.141
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2016.141
Keywords
This article is cited by
-
Searching for optimal blood pressure targets in type 2 diabetic patients with coronary artery disease
Cardiovascular Diabetology (2019)