Abstract
Preeclampsia is a major cause of maternal death and morbidity. Body mass index (BMI) predicts an increased risk of developing hypertensive disorders and preeclampsia. However, waist-to-hip ratio (WHR), as a central obesity index, has not been assessed in predicting this disorder in pregnancy. We assumed that WHR might be more sensitive in predicting the risk of preeclampsia, compared with BMI. The aim of this cohort study was to investigate the relationships of BMI and WHR with preeclampsia. This was a prospective cohort study of 1200 pregnant women with singleton pregnancies. Anthropometric indices included WHR and BMI, which were measured at the first antenatal visit (⩽12 weeks of gestational age). The incidence of preeclampsia was assessed after 20 weeks of gestation. Maternal demographic data and obstetric outcomes were also recorded for each subject. All of the statistical tests were performed using SPSS software, version 16. The overall incidence of preeclampsia in the study population was 4.2%. The maternal WHR and BMI at the beginning of pregnancy were significantly associated with the occurrence of preeclampsia (P=0.006 and P=0.001, respectively). WHR⩾0.85 and BMI⩾25 kg m−2 in the first 12 weeks of pregnancy had relative risks of 2.317 (confidence interval (CI): 1.26–4.27) and 3.317 (CI: 1.6–6.86) for preeclampsia. BMI and WHR were anthropometric indicators that presented correlations with preeclampsia. Of these anthropometric indices, BMI had greater predictive value in preeclampsia.
Similar content being viewed by others
Introduction
Gestational hypertension and preeclampsia is a leading cause of maternal and perinatal mortality and morbidity, and can affect up to 10% of pregnancies.1 Preeclampsia is defined as a new onset of hypertension and proteinuria2 that complicates 3–4% of all pregnancies. Despite several decades of investigations, the underlying pathophysiology remains uncertain. Because the cause of preeclampsia is unknown, clinical interventions for treatment have also been limited.3 Currently, termination of pregnancy is a choice treatment in many conditions, so preeclampsia is one cause of pre-term birth,4 and considering the limitations in the treatment of this disorder, there is a considerable interest in determining methods to prevent preeclampsia.1
Some risk factors for preeclampsia include first pregnancy, age older than 40 years, multiple pregnancies, high body mass index (BMI), and a history of chronic hypertension. The incidence of preeclampsia has increased over the past decade, in part, due to the rise in women becoming pregnant at older ages and an increase in obesity among women.4 The prevalence of obesity during pregnancy has doubled over the past 20 years,5 and studies have shown that obesity is strongly associated with adverse gestational and perinatal outcomes, including preeclampsia and eclampsia.1, 5, 6, 7, 8 Maternal obesity is the strongest modifiable risk factor for preeclampsia, thus providing a potential means of prevention.1 Some studies have shown that obesity can increase the risk of preeclampsia, and women with low BMI were less likely to develop preeclampsia.6, 7, 8
Obesity is defined as a condition of excessive body fat, and it is usually assessed by BMI.5 Waist-to-hip ratio (WHR) is another anthropometric index that better reflects the accumulation of intra-abdominal fat compared with BMI, which is affected by the height index. WHR has been shown to be a better predictor of the risk of type 2 diabetes,9 cardiovascular risk10, 11 and hypertension12 than BMI.10 Waist circumference (WC) and WHR are now recommended as screening tools for health risks among the general public, such as cardiovascular disease, type 2 diabetes, respiratory insufficiency, low back pain and degree of physical function.13
Most studies have used BMI as a risk factor for the development of preeclampsia in the antenatal period.5, 6, 7, 8 We assumed that WHR might be more sensitive in predicting the risk of preeclampsia, compared with BMI. The aim of this cohort study was to investigate the relationships of BMI and WHR with preeclampsia.
Methods
Subjects
This was a prospective cohort study of 1200 pregnant women with singleton pregnancies attending their first routine prenatal care visits at the Health Medical Centers of Kashan University of Medical Sciences, Kashan, Central Iran, from April 2008 to May 2010. The inclusion criteria were: no medical and familial history of systemic disease, such as hypertension and diabetes mellitus; no history of preeclampsia in previous pregnancies; and gestational age ⩽12 weeks at the first antenatal visit. Women with termination of pregnancy before 24 weeks of gestation were excluded from the study. The subjects were followed prospectively until delivery.
Measurements
Gestational age was estimated from the date of the last menstrual period. Waist and hip circumference were measured at the first antenatal visit. Anthropometric measurements included waist and hip circumferences, determined by trained midwives using standard non-stretch tape with the subjects wearing light clothes. Because intermeasurer errors of the WC and hip circumference measurements were approximately 1.56 cm and 1.38 cm, respectively,14 duplicate measurements were obtained to minimize errors.
WC was measured at the midpoint, above the iliac crest and below the lowest rib margin, in the standing position with minimal expiration. Hip circumference was measured at the widest point over the buttocks.15 The WHR was obtained by dividing the values of the waist and hip circumferences, and their classification was based on a cutoff point of 0.85.12 BMI was calculated as weight in kilograms divided by the square of height in meters. The BMI cutoff point for overweight was 25 kg m−2, according to the WHO (World Health Organization).16 BMI also was categorized according to the WHO definitions of underweight (⩽18.5 kg m−2), normal (18.5–24.9 kg m−2), overweight (25.0–29.9 kg m−2) and obese (⩾30.0 kg m−2).17
Women received a diagnosis of preeclampsia if elevation of blood pressure ⩾140 mm Hg systolic or ⩾90 mm Hg diastolic was obtained on two assessments at least 6 h apart, and proteinuria was defined by a qualitative 1+ dipstick reading on two samples after 20 weeks of gestation.2, 3 Blood pressure was measured by a mercury sphygmomanometer, according to standard procedures. Maternal demographic data and obstetric outcomes were also recorded for each subject. The data on pregnancy outcomes were collected from the hospital maternity records.
Data analysis
The relationships between preeclampsia and categorical variables were analyzed by the χ2 test, and relationships of continuous variables were analyzed using Student’s t-test. The relative risk and confidence intervals (CIs) were also calculated in this study. All of the statistical tests were performed using the SPSS software v.16.0 (SPSS Inc., Chicago, IL, USA).
Ethical considerations
This study was approved by the Kashan University of Medical Sciences Ethics Committee. Informed consent was obtained from the women who agreed to participate in the study.
Results
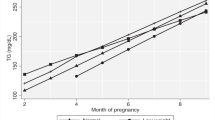
A total of 1000 women completed the study. The women’s ages ranged from 15 to 43 years, with mean and median ages of 26.39 and 25.0 years, respectively (s.d.=5.57). The mean waist and hip circumferences at recruitment were 80.12±10.3 cm and 100.65±9.1 cm, respectively, and the mean WHR was 0.79±0.61. The women had a mean BMI of 25.57±4.48 kg m−2. Of these 1000 women, 4.2% developed preeclampsia and 34 women had gestational hypertension (Table 1). Basic characteristics of the women with and without preeclampsia are presented in Table 2.
No significant relationships were found between the incidence of preeclampsia and maternal age, the number of prior gestations and gestational age at recruitment (Table 2). The anthropometric parameters of weight, height, waist and hip circumference, WHR and BMI had significant relationships with the incidence of preeclampsia. The systolic and diastolic blood pressure at the beginning of the study was significantly higher in the women who developed preeclampsia later (Table 2). The neonatal birth weight was lower in preeclamptic mothers (P=0.012). The women with preeclampsia had lower gestational ages at delivery. The rate of cesarean section was 62% in the women with preeclampsia, whereas this rate was 37.4% in the women without preeclampsia (P=0.001).
The maternal WHR and BMI at the beginning of the study were significantly associated with the occurrence of preeclampsia. WHR⩾0.85 in the first 12 weeks of pregnancy had a relative risk of 2.317 (CI: 1.26–4.27) for preeclampsia, while the relative risk with BMI⩾25 kg m−2 was 3.31 (CI: 1.6–6.86; Table 3). Among these anthropometric indices, BMI had a more predictive value in preeclampsia.
Discussion
To our knowledge, this was the first cohort study that was designed to investigate the associations of maternal WHR and BMI in early pregnancy (⩽12 weeks of gestation). We found that women who developed preeclampsia had higher BMI and WHR at gestational week ⩽12 than women who did not develop this disorder.
In the current study, the incidences of gestational hypertension and preeclampsia were 3.4 and 4.2%, respectively. The incidence has been reported as 3.1% in the United States,18 2.13% in Iran,19 and 4% in Norway.20 The incidence of preeclampsia is 2–8% in all pregnancies worldwide.21 The incidence of preeclampsia in our study was comparable to its worldwide estimation, although in one study in Brazil, the prevalence of this disorder was 13.8%.22 It seems that racial variations, age, number of previous pregnancies, socioeconomic status and other conditions might influence the occurrence of preeclampsia.4, 19, 23
The probable effects of maternal age on preeclampsia have been previously studied. Some studies have shown that with the increasing ages of pregnant women, adverse obstetric complications and preeclampsia have also been increasing.24, 25, 26 Women older than 35 years were 1.5 times more likely to develop preeclampsia, compared with younger mothers.27 In a retrospective study of 6619 singleton pregnancies, Wang et al.28 did not find a relationship between women’s ages and preeclampsia. The authors suggested that disorders such as hypertension or diabetes could influence the outcomes of pregnancies, but age alone was not a risk factor.
We did not find an association between maternal age and preeclampsia. In addition, the frequency of preeclampsia in nulliparous and multiparous pregnant women was not different. However, several previous studies have reported higher incidences of adverse obstetric complications and preeclampsia in nulliparous pregnant women.29, 30 A systematic review of controlled cohort studies indicated that the risk of preeclampsia was increased in nulliparous women.31 These differences could be explained by the characteristics of the subjects. The mean age of the mothers was 26.36 years, and the number of mothers older than 35 years (7.8%) was low in our study. Furthermore, the mean age of the mothers who were pregnant for the first time was 24.04±4.32 years, which could have caused an insignificant association between maternal age and preeclampsia. In addition, according to the inclusion criteria of this study, women with histories of previous preeclampsia were not enrolled. Therefore, the absence of subjects with risk factors for preeclampsia led to the data being diluted, and the relationship between parity and preeclampsia was not significant. However, a number of studies have confirmed that parity did not have significant associations with hypertension or preeclampsia;32, 33, 34 thus, there is a need to carefully monitor both nulliparous and multiparous pregnant women for any changes in blood pressure and for signs and symptoms of preeclampsia.
Obesity, which is increasing at an alarming rate, has been considered a risk factor for preeclampsia.21, 22 Obesity increases insulin resistance, which has been associated with endothelial dysfunction and vasoconstriction. In addition, insulin resistance increases the risks of hypertension and cardiovascular diseases.22 Central fat deposition is a reversible cause of hypertension, insulin resistance and elevated plasma lipids.13
Obesity is determined by different indices, such as BMI and WHR. BMI is an accepted anthropometric index that measures general obesity,9 and it has been reported to be closely related to the risks of hypertension disorders and preeclampsia in pregnancy.6, 7, 22, 35, 36, 37 WC or WHR are other known obesity indices that might better reflect abdominal adiposity and be better predictors of diabetes, hypertension and cardiovascular disease than BMI.5, 9 WHR has some advantages over BMI. WC is a good marker of central fat distribution. In addition, its measurement is easier, and women can easily self-measure this index.5, 11 WHR is also not influenced, like BMI, by other factors, such as height and muscle mass.9, 38 Some experts believe that WHR is the best predictor among other obesity markers.5, 11
We found that both maternal WHR and BMI could predict preeclampsia. The relative risks of WHR and BMI were 2.317 and 3.317, respectively. It seems that WHR, measured at ⩽12 weeks of gestation, can be a good predictor of preeclampsia. This index, although widely used in nonpregnant women to assess obesity and related health risks,9, 10, 11, 12 has received little attention in pregnancy. Yamamoto et al.39 also found that WHR and BMI in early pregnancy were both related to the risk of preeclampsia.
One strength of the present study was its prospective nature, which allowed us to freely collect all the data needed for the study, and causal relationships in this cohort study could be investigated. The anthropometric indices were measured before pregnancy weight gain and earlier than in other studies, which mostly measured these indices after the first trimester.13, 40
In conclusion, data from this investigation suggested that an appropriate maternal BMI (18.5–24.9) and WHR index (>0.85) at conception had substantial impacts on the overall health of pregnant women and could result in better obstetric management.
Conclusions
BMI and WHR were anthropometric indicators that presented correlations with preeclampsia. These data support the hypothesis that high BMI and WHR can be considered risk factors for preeclampsia.
References
Macdonald-Wallis C, Tilling K, Fraser A, Nelson S, Lawlor D . Gestational weight gain as a risk factor for hypertensive disorders of pregnancy. Am J Obstet Gynecol 2013; 209: 327.e1–327.e17.
Lindheimer MD, Taler SJ, Cunningham F . ASH position paper: hypertension in pregnancy. J Clin Hypertens 2009; 11: 214–225.
Robinson C, Hill E, Alanis M, Chang E, Johnson D, Almeida J . Examining the effect of maternal obesity on outcome of labor induction in patients with preeclampsia. Hypertens Pregnancy 2010; 29: 446–456.
Rosser ML, Katz NT . Preeclampsia: an obstetrician’s perspective. Adv Chronic Kidney Dis 2013; 20: 287–296.
Wendland EM, Duncan BB, Mengue SS, Nucci LB, Schmidt MI . Waist circumference in the prediction of obesity-related adverse pregnancy outcomes. Cad Saude Publica 2007; 23: 391–398.
Tsai IH, Chen CP, Sun FJ, Wu CH, Yeh SL . Associations of the pre-pregnancy body mass index and gestational weight gain with pregnancy outcomes in Taiwanese women. Asia Pac J Clin Nutr 2012; 21: 82–87.
Syngelaki A, Bredaki FE, Vaikousi E, Maiz N, Nicolaides KH . Body mass index at 11-13 weeks’ gestation and pregnancy complications. Fetal Diagn Ther 2011; 30: 250–265.
Belogolovkin V, Eddleman KA, Malone FD, Sullivan L, Ball RH, Nyberg DA, Comstock CH, Hankins GD, Carter S, Dugoff L, Craigo SD, Timor-Tritsch IE, Carr SR, Wolfe HM, D'Alton ME . The effect of low body mass index on the development of gestational hypertension and preeclampsia. J Matern Fetal Neonatal Med 2007; 20: 509–513.
Cheng C-H, Ho C-C, Yang C-F, Huang Y-C, Lai C-H, Liaw Y-P . Waist-to-hip ratio is a better anthropometric index than body mass index for predicting the risk of type 2 diabetes in Taiwanese population. Nutr Res 2010; 30: 585–593.
Oliveira M, Fagundes R, Moreira E, Trindade E, Carvalho T . Relation between anthropometric indicators and risk factors for cardiovascular disease. Arq Bras Cardiol 2010; 94: 478–485.
Winter Y, Rohrmann S, Linseisen J, Lanczik O, Ringleb PA, Hebebrand J, Back T . Contribution of obesity and abdominal fat mass to risk of stroke and transient ischemic attacks. Stroke 2008; 39: 3145–3151.
Feldstein CA, Akopian M, Olivieri AO, Kramer AP, Nasi M, Garrido D . A comparison of body mass index and waist-to-hip ratio as indicators of hypertension risk in an urban Argentine population: a hospital-based study. Nutr Metab Cardiovasc Dis 2005; 15: 310–315.
Sattar N, Clark P, Holmes A, Lean ME, Walker I, Greer IA . Antenatal waist circumference and hypertension risk. Obstet Gynecol 2001; 97: 268–271.
Waist circumference and waist–hip ratio: report of a WHO expert consultation. http://apps.who.int/iris/bitstream/10665/44583/1/9789241501491_eng.pdf December 2008.
Wang F, Wu S, Song Y, Tang X, Marshall R, Liang M, Wu Y, Qin X, Chen D, Hu Y . Waist circumference, body mass index and waist to hip ratio for prediction of the metabolic syndrome in Chinese. Nutr Metab Cardiovasc Dis 2009; 19: 542–547.
Li G, Xie F, Yan S, Hu X, Jin B, Wang J, Wu J, Yin D, Xie Q . Subhealth: definition, criteria for diagnosis and potential prevalence in the central region of China. BMC Public Health 2013; 4: 446.
Macdonald-Wallis C, Lawlor DA, Heron J, Fraser A, Nelson SM, Tilling K . Relationships of risk factors for pre-eclampsia with patterns of occurrence of isolated gestational proteinuria during normal term pregnancy. PLoS ONE 2011; 6: e22115.
Lisonkova S, Joseph KS . Incidence of preeclampsia: risk factors and outcomes associated with early- versus late-onset disease. Am J Obstet Gynecol 2013; 209: 544.e1–544.e12.
Zibaeenezhad M, Ghodsi M, Arab P, Gholzom N . The prevalence of hypertensive disorders of pregnancy in Shiraz, Southern Iran. Int Cardiovasc Res J 2010; 4: 169–172.
Nilsen RM, Bjørke-Monsen AL, Midttun O, Nygård O, Pedersen ER, Ulvik A, Magnus P, Gjessing HK, Vollset SE, Ueland PM . Maternal tryptophan and kynurenine pathway metabolites and risk of preeclampsia. Obstet Gynecol 2012; 119: 1243–1250.
Jeyabalan A . Epidemiology of preeclampsia: impact of obesity. Nutr Rev 2013; 71 (Suppl 1): 18–25.
Dantas EM, Pereira FV, Queiroz JW, Dantas DL, Monteiro GR, Duggal P, Azevedo Mde F, Jeronimo SM, Araújo AC . Preeclampsia is associated with increased maternal body weight in a northeastern Brazilian population. BMC Pregnancy Childbirth 2013; 13: 159.
Rudra Cb, Fau—Williams MA, Williams MA . Monthly variation in preeclampsia prevalence: Washington State, 1987-2001. J Matern Fetal Neonatal Med 2005; 18: 319–324.
Khalil A, Syngelaki A, Maiz N, Zinevich Y, Nicolaides KH . Maternal age and adverse pregnancy outcome: a cohort study. Ultrasound Obstet Gynecol 2013; 42: 634–643.
Yogev Y, Melamed N, Bardin R, Tenenbaum-Gavish K, Ben-Shitrit G, Ben-Haroush A . Pregnancy outcome at extremely advanced maternal age. Am J Obstet Gynecol 2010; 203: 558.e1–558.e7.
Hsieh TT, Liou JD, Hsu JJ, Lo LM, Chen SF, Hung TH . Advanced maternal age and adverse perinatal outcomes in an Asian population. Eur J Obstet Gynecol Reprod Biol 2010; 148: 21–26.
Lamminpaa R, Vehvilainen-Julkunen K, Gissler M, Heinonen S . Preeclampsia complicated by advanced maternal age: a registry-based study on primiparous women in Finland 1997-2008. BMC Pregnancy Childbirth 2012; 12: 47.
Wang Y, Tanbo T, Abyholm T, Henriksen T . The impact of advanced maternal age and parity on obstetric and perinatal outcomes in singleton gestations. Arch Gynecol Obstet 2011; 284: 31–37.
Lee CJ, Hsieh TT, Chiu TH, Chen KC, Lo LM, Hung TH . Risk factors for pre-eclampsia in an Asian population. Int J Gynaecol Obstet 2000; 70: 327–333.
Hernandez-Diaz S, Toh S, Cnattingius S . Risk of pre-eclampsia in first and subsequent pregnancies: prospective cohort study. BMJ 2009; 338: b2255.
Duckitt K, Harrington D . Risk factors for pre-eclampsia at antenatal booking: systematic review of controlled studies. BMJ 2005; 330: 565.
Ayala DE, Hermida RC . Influence of parity and age on ambulatory monitored blood pressure during pregnancy. Hypertension 2001; 38 (3 Pt 2): 753–758.
Castiglioni MT, Valsecchi L, Cavoretto P, Pirola S, Di Piazza L, Maggio L, Caretto A, Garito TS, Rosa S, Scavini M . The risk of preeclampsia beyond the first pregnancy among women with type 1 diabetes parity and preeclampsia in type 1 diabetes. Pregnancy Hypertens 2014; 4: 34–40.
Ishikuro M, Obara T, Metoki H, Ohkubo T, Yamamoto M, Akutsu K, Sakurai K, Iwama N, Katagiri M, Yagihashi K, Yaegashi N, Mori S, Suzuki M, Kuriyama S, Imai Y . Blood pressure measured in the clinic and at home during pregnancy among nulliparous and multiparous women: the BOSHI study. Am J Hypertens 2013; 26: 141–148.
Nohr EA, Timpson NJ, Andersen CS, Davey Smith G, Olsen J, Sorensen TI . Severe obesity in young women and reproductive health: the Danish National Birth Cohort. PLoS ONE 2009; 4: e8444.
Sahu MT, Agarwal A, Das V, Pandey A . Impact of maternal body mass index on obstetric outcome. J Obstet Gynaecol Res 2007; 33: 655–659.
Marshall NE, Guild C, Cheng YW, Caughey AB, Halloran DR . Maternal superobesity and perinatal outcomes. Am J Obstet Gynecol 2012; 206: 417.e1–417.e6.
Klein S, Wadden T, Sugerman HJ . AGA technical review on obesity. Gastroenterology 2002; 123: 882–932.
Yamamoto S, Douchi T, Yoshimitsu N, Nakae M, Nagata Y . Waist to hip circumference ratio as a significant predictor of preeclampsia, irrespective of overall adiposity. J Obstet Gynaecol Res 2001; 27: 27–31.
Kongubol A, Phupong V . Prepregnancy obesity and the risk of gestational diabetes mellitus. BMC Pregnancy Childbirth 2011; 11: 59.
Acknowledgements
We express our gratitude to the women who participated in this study and to the health centers' midwives who made this study possible. This study was funded and supported by Deputy of Research, Kashan University of Medical Sciences, Kashan, Iran.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Taebi, M., Sadat, Z., Saberi, F. et al. Early pregnancy waist-to-hip ratio and risk of preeclampsia: a prospective cohort study. Hypertens Res 38, 80–83 (2015). https://doi.org/10.1038/hr.2014.133
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2014.133
Keywords
This article is cited by
-
What is the “cost” of reducing adverse pregnancy outcomes in patients with gestational diabetes mellitus - risk factors for perinatal complications in a retrospective cohort of pregnant women with GDM
BMC Pregnancy and Childbirth (2022)
-
Epidemiology of hypertensive disorders in pregnancy: prevalence, risk factors, predictors and prognosis
Hypertension Research (2017)
-
Pathophysiology of preeclampsia: an angiogenic imbalance and long-lasting systemic vascular dysfunction
Hypertension Research (2017)
-
From apelin to exercise: emerging therapies for management of hypertension in pregnancy
Hypertension Research (2017)
-
Maternal, fetal and perinatal alterations associated with obesity, overweight and gestational diabetes: an observational cohort study (PREOBE)
BMC Public Health (2016)