Abstract
Objective
This was a pilot randomised controlled trial (RCT) to investigate the effect of post-operative face-down positioning on the outcome of macular hole surgery and to inform the design of a larger definitive study.
Methods
In all, 30 phakic eyes of 30 subjects with idiopathic full-thickness macular holes underwent vitrectomy with dye-assisted peeling of the ILM and 14% perfluoropropane gas. Subjects were randomly allocated to posture face down for 10 days (posturing group) or to avoid a face-up position only (non-posturing group). The primary outcome was anatomical hole closure.
Results
Macular holes closed in 14 of 15 eyes (93.3%; 95% confidence interval (CI) 68–100%) in the posturing group and in 9 of 15 (60%; 95% CI 32–84%) in the non-posturing group. In a subgroup analysis of outcome according to macular hole size, all holes smaller than 400 μm closed regardless of posturing (100%). In contrast, holes larger than 400 μm closed in 10 of 11 eyes (91%; 95% CI 58–99%) in the posturing group and in only 4 of 10 eyes (40%; 95% CI 12–74%) in the non-posturing group (Fisher's exact test P=0.02).
Conclusion
Post-operative face-down positioning may improve the likelihood of macular hole closure, particularly for holes larger than 400 μm. These results support the case for a RCT.
Similar content being viewed by others
Introduction
Vitrectomy with intraocular gas tamponade results in closure of full-thickness macular holes and improves vision in the majority of eyes. The surgical technique originally described in 1991 by Kelly and Wendel1 comprised three-port pars plana vitrectomy combined with meticulous removal of the posterior cortical vitreous and intraocular tamponade with a long-acting gas followed by a period of face-down positioning. Vitrectomy relieves the antero-posterior and centrifugal tangential traction responsible for induction and maintenance of foveal dehiscence. The mechanism by which gas can facilitate macular hole closure is less well understood, but gas may promote retinal reattachment the by virtue of its surface tension, and/or facilitate re-apposition of the macular hole edges by providing a surface for glial migration.2, 3 Face-down positioning might enhance the effect of the gas tamponade by ensuring that the macula is consistently in contact with the surface of the gas bubble, or enhance any effect of its buoyancy.4 However, the value of face-down positioning following surgery is unproven. Results of a number of studies question the value of posturing, demonstrating favourable outcomes with shortened durations of posturing,5, 6, 7 and with no posturing at all.8, 9, 10 Furthermore, face-down positioning is an arduous challenge and the prospect can be a significant deterrent to surgery for some people.11 It is disabling, delays rehabilitation and in some instances is wholly unfeasible even with the aid of specially designed supports. Rarely, face-down positioning has been associated with serious adverse effects, such as ulnar neuropathy12 and increased risk of thromboembolism.13 A recent review identified no significant effect of the duration of face-down posturing on the rate of macular hole closure, and concluded that well-conducted randomised control trials are needed.14 The primary purpose of the present pilot RCT of face-down positioning following surgery for macular hole was to estimate the effect size, variance, and recruitment rate to inform the design of a definitive RCT.
Materials and methods
Study population and design
We conducted a prospective interventional, comparative, and randomised clinical trial in 30 eyes of 30 subjects listed for macular hole surgery at Moorfields Eye Hospital (MEH, London, UK) or Whipps Cross Hospital (London, UK). We were able to recruit up to four subjects per month during the period from October 2007 to February 2010. The study was approved by the hospital research governance committees and by the local research ethics committee. We included individuals with stage II, III, and IV idiopathic full-thickness macular holes confirmed by optical coherence tomography (OCT)15, 16 in the eyes of subjects able and willing to posture face-down. We excluded individuals with any history of previous intraocular surgery (including cataract surgery) or ocular trauma, and those with a history of visual loss greater than 1 year suggesting macular hole duration of longer than 12 months. Pre-operatively, we recorded demographic data, the estimated duration of the macular hole and the best-corrected visual acuity (expressed as logMAR unit) for each subject. We performed a complete ocular examination including anterior segment evaluation, intraocular pressure measurement, fundus examination, and OCT of the macula (Stratus OCT III, Carl Zeiss Meditec, Dublin, CA, USA). Six radial scans were performed and the largest apical diameter was recorded for analysis using the caliper function (Figure 1).
Operative technique
The surgery was performed by consultant vitreoretinal surgeons or by fellows in subspeciality training.
All subjects underwent complete 20-gauge three-port pars plana vitrectomy with peeling of the posterior hyaloid in eyes, in which the posterior vitreous was not already detached, and peeling of the inner limiting membrane. The ILM was stained using trypan-blue 0.15% (Membrane Blue, DORC, Zuidland, The Netherlands) under fluid for 2 min. Cryo-retinopexy was applied to any peripheral breaks and a fluid-air exchange and a complete air-gas exchange was performed using perfluropropane gas (C3F8 14%). Exclusion criteria included the presence of retinal breaks for which post-operative posturing was advised, the presence of lens opacity for which cataract surgery was performed, and any pre-operative complication precluding conventional macular hole surgery and posturing.
Randomisation
At the completion of surgery subjects were randomly allocated in a 1 : 1 ratio to posturing or non-posturing groups. Randomisation was stratified according to macular hole stage and was generated using random permuted blocks of varying sizes. The randomisation schedule was held by a statistician in the Clinical Trials Unit, and clinicians contacted the statistician on the day of surgery to determine the allocation. Subjects in the posturing group were asked to maintain a face-down position for 50 min in every hour for 10 days following surgery. Subjects in the non-posturing group were asked only to avoid a face-up position with no other restriction. The investigators in the trial were masked to treatment allocation. We did not attempt to estimate compliance with instructions on positioning.
Follow-up
We reviewed all subjects 1 week after surgery and documented visual acuity and any adverse events. Furthermore, we asked the subjects if they would be willing to undergo the same treatment again if the macular hole does not close given a 50 : 50 chance of successful hole closure and an improvement in vision. After 6–8 weeks of the surgery we measured the best-corrected visual acuity and determined the final macular hole status by biomicroscopy and by OCT imaging. OCT scans were anonymised and sent to two independent retinal surgeons (ZG and DC) who graded the macular holes in a masked fashion as ’closed’, ’open and flat’ (no cuff of subretinal fluid), or ’open and elevated’.
Data analysis
As this was a pilot study, we primarily conducted a descriptive analysis. In addition, we performed a retrospective subgroup analysis of outcome according to the size of the macular hole as determined by OCT, comparing the effect of positioning on anatomical closure and visual acuity gain between the eyes with small (<400 μm) and large macular holes (≥400 μm). We used the results to calculate the sample size required to identify a significant effect of face-down positioning in a definitive randomised controlled trial, based on a power of 90% and P<0.05.
Results
In all, 30 eyes of 30 subjects were included and allocated randomly to each treatment group (Supplementary Table). There were no significant differences in the baseline parameters of subjects allocated to the posturing and the non-posturing group (see Table 1). All subjects enrolled in this trial complied with the examination schedule and completed the study; none withdrew or were lost to the follow-up.
Anatomical closure of macular holes
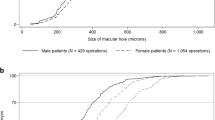
After 1 week of surgery all subjects had hand movements vision and the persistent gas fill precluded assessment of macular hole status by clinical examination or by OCT. After 6–8 weeks of the surgery, macular holes were closed in 23 of 30 (76.7%) eyes overall. Macular holes were closed in 14 of 15 eyes in the posturing group (93.3%; 95% CI 68–100% and in 9 of 15 eyes in the non-posturing group (60%; 95% CI 32–84%, Figure 2a). Of the six subjects in the non-posturing group with persistent macular holes, three were operated by consultant vitreoretinal surgeons and three by fellows in subspeciality training. The one subject in the posturing group with a persistent macular hole was operated by a consultant. In a subgroup analysis of outcome according to macular hole size, all nine of nine (100%) holes smaller than 400 μm closed regardless of posturing (four eyes in the posturing group and five eyes in the non-posturing group). Of macular holes larger than 400 μm, 10 of 11 (91%; 95% CI 58–99%) closed in the posturing group, and only 4 of 10 (40%; 95% CI 12–74%) closed in the non-posturing group (Fisher's exact test P=0.02, Figure 2b).
Visual acuity
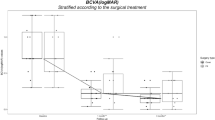
The mean final visual acuity of eyes in the posturing group improved from 0.88 (95% CI 0.79–0.97) to 0.65 logMAR unit (95% CI 0.45–0.83) and in the non-posturing group from 0.81 (95% CI 0.66–0.95) to 0.76 logMAR unit (95% CI 0.53–1.0). The mean final visual acuity improved by more than 0.2 logMAR unit in 10 of 15 eyes (66%) in the posturing group and in 6 of 15 eyes (40%) in the non-posturing group. A subgroup analysis according to the pre-operative MH size demonstrated a mean visual acuity gain of 0.16 logMAR unit (95% CI from –0.16 to 0.48) for macular holes smaller than 400 μm in the posturing group and 0.17 logMAR unit (95% CI 0.01–0.33) in the non-posturing group. In macular holes larger than 400 μm there was a mean visual acuity gain of 0.26 logMAR unit (95% CI from –0.1 to 0.55) in the posturing group and a mean visual acuity loss of 0.01 logMAR unit (95% CI 0.32–0.30) in the non-posturing group (Figure 3).
Change in visual acuity after macular hole surgery according to post-operative positioning for (a) all subjects (b–d) subgroups according to pre-operative macular hole size. (c) Each dot represents the change of VA in one individual. Dots above the green dotted line represent eyes with a significant improvement in visual acuity (≥0.2 logMAR unit). Dots below the red dotted line represent eyes with a significant deterioration in visual acuity (≥0.2 logMAR unit). The vertical black dotted line separates macular holes smaller and larger than 400 μm.
Non-closure of macular holes and complications
Macular holes remained open in 6 of 15 eyes in the non-posturing group and in 1 of 15 eyes in the posturing group at 6 weeks following surgery. In one subject of the non-posturing group the persistently open hole was associated with the development of retinal detachment with no other break. All subjects with persistently open macular holes elected to proceed with further intraocular gas tamponade and post-operative face-down posturing; anatomical closure was achieved following this second procedure in six of the seven (86%) eyes.
One subject in the posturing group developed an intraretinal macular haemorrhage resulting from iatrogenic trauma to the inner retinal trauma during the ILM peel. No other adverse effects were identified. In all, 10 out of 11 subjects in the posturing group and nine out of nine subjects in the non-posturing group stated 1 week after surgery that they would be prepared to undergo the same procedure again if the macular hole does not close given a 50 : 50 chance of successful hole closure and an improvement in vision. One patient in the posturing group stated that the prospect of posturing again would deter him from further surgery.
Discussion
Until recently, good evidence for any benefit of face-down positioning following surgery for macular holes has been lacking. Several non-randomised comparative series report high rates of anatomical closure with limited or no face-down positioning at all.7, 8, 9, 10 In 2008, however, Guillaubey et al17 reported the results of a RCT that suggested that face-down positioning for 5 days can improve the likelihood of hole closure, particularly closure of large holes. In their study, however, nearly half of the eyes underwent combined phaco-vitrectomy. Simultaneous cataract surgery may facilitate a more complete vitrectomy enabling injection of a larger volume of gas than in phakic eyes, which could reduce the need for face-down positioning in this group of subjects. This has been investigated in a companion study18 that suggests no benefit from posturing when vitrectomy is combined with cataract surgery. Furthermore, Guillaubey et al arbitrarily used a range of tamponade gases according to the size of the macular hole and acknowledged that this could also be a source of potential bias. Systematic reviews and meta-analyses of the relevant trials are limited by significant differences in the surgical techniques used, post-operative positioning regimes prescribed and outcome measures reported.14 There is a consensus that appropriately designed randomised controlled studies are required to investigate this question.19, 20 The aim of this pilot RCT was to explore the feasibility of a definitive trial to determine the value of face-down positioning following vitrectomy, ILM peeling, and C3F8 gas tamponade for full-thickness macular holes, without simultaneous phacoemulsification. In our study, we observed an anatomical closure rate of 93.3% and a mean visual acuity gain of 0.23 logMAR unit in the posturing group, a result that is consistent with previously published data.17, 21 In the non-posturing group, in contrast, we found a MH closure rate of only 60% and a mean visual acuity gain of 0.05 logMAR unit. The non-posturing group may have a worse outcome because of increased risk of cataract.11 The visual acuity outcomes in this study are less good than those in our companion study.18 This difference may reflect the effect of lens opacities in subjects in this study and the earlier assessment of outcome (6 weeks vs 6 months).
The results of this study are consistent with those of Guillaubey et al17 in suggesting that post-operative face-down positioning can improve the likelihood of macular hole closure. The possible benefit of face-down positioning appears to be relevant to macular holes of greater than 400 μm in diameter. We are not able to make firm conclusions from this trial, because the number of eyes is small.
However, we calculated that a two-group χ2-test with a 0.05 two-sided significance level will have 90% power to detect the difference between a group 1 proportion of 0.9 and a group 2 proportion of 0.6, when the sample size in each group is 42. A definitive RCT will therefore need to include a minimum of 42 eyes in each arm to be able to determine the value of face-down positioning, with confidence in eyes that undergo vitrectomy and ILM peel without simultaneous cataract surgery.

References
Kelly NE, Wendel RT . Vitreous surgery for idiopathic macular holes. Results of a pilot study. Arch Ophthalmol 1991; 109: 654–659.
Madreperla SA, Geiger GL, Funata M, de la Cruz Z, Green WR . Clinicopathologic correlation of a macular hole treated by cortical vitreous peeling and gas tamponade. Ophthalmology 1994; 101: 682–686.
Thompson JT, Smiddy WE, Glaser BM, Sjaarda RN, Flynn Jr HW . Intraocular tamponade duration and success of macular hole surgery. Retina 1996; 16: 373–382.
Berger JW, Brucker AJ . The magnitude of the bubble buoyant pressure: implications for macular hole surgery. Retina 1998; 18: 84–86.
Mulhern MG, Cullinane A, Cleary PE . Visual and anatomical success with short-term macular tamponade and autologous platelet concentrate. Graefes Arch Clin Exp Ophthalmol 2000; 238: 577–583.
Park DW, Sipperley JO, Sneed SR, Dugel PU, Jacobsen J . Macular hole surgery with internal-limiting membrane peeling and intravitreous air. Ophthalmology 1999; 106: 1392–1397.
Isomae T, Sato Y, Shimada H . Shortening the duration of prone positioning after macular hole surgery- comparison between 1-week and 1-day prone positioning. Jpn J Ophthalmol 2002; 46: 84–88.
Tornambe PE, Poliner LS, Grote K . Macular hole surgery without face-down positioning. A pilot study. Retina 1997; 17: 179–185.
Tranos PG, Peter NM, Nath R, Singh M, Dimitrakos S, Charteris D et al. Macular hole surgery without prone positioning. Eye (Lond) 2007; 21: 802–806.
Rubinstein A, Ang A, Patel CK . Vitrectomy without postoperative posturing for idiopathic macular holes. Clin Experiment Ophthalmol 2007; 35: 458–461.
Ellis JD, Baines PS . Patient perspectives on macular hole surgery. Ophthalmology 2002; 109: 622–623.
Vincent JM, Peyman GA, Ratnakaram R . Bilateral ulnar decubitus as a complication of macular hole surgery. Ophthalmic Surg Lasers Imaging 2003; 34: 485–486.
Au Eong KG, Beatty S, Thomas W, Sen V, Turner GS . Pulmonary embolism following head positioning for retinal reattachment surgery in a young patient with factor V leiden mutation. Arch Ophthalmol 2000; 118: 1300–1301.
Tatham A, Banerjee S . Face-down posturing after macular hole surgery: a meta-analysis. Br J Ophthalmol 2010; 94: 626–631.
Gass JD . Reappraisal of biomicroscopic classification of stages of development of a macular hole. Am J Ophthalmol 1995; 119: 752–759.
Gass JD . Idiopathic senile macular hole. Its early stages and pathogenesis. Arch Ophthalmol 1988; 106: 629–639.
Guillaubey A, Malvitte L, Lafontaine PO, Jay N, Hubert I, Bron A et al. Comparison of face-down and seated position after idiopathic macular hole surgery: a randomized clinical trial. Am J Ophthalmol 2008; 146: 128–134.
Yorston D, Siddiqui R, Awan A, Walker S, Bunce C, Bainbridge JW . Pilot randomised controlled trial of face-down posturing following phacovitrectomy for macular hole. Eye 2012; 26: 267–271.
Dhawahir-Scala FE, Maino A, Saha K, Mokashi AA, McLauchlan R, Charles S . To posture or not to posture after macular hole surgery. Retina 2008; 28: 60–65.
Williams GA . Macular holes: the latest in current management. Retina 2006; 26: S9–S12.
Ezra E, Gregor ZJ . Surgery for idiopathic full-thickness macular hole: two-year results of a randomized clinical trial comparing natural history, vitrectomy, and vitrectomy plus autologous serum: Morfields Macular Hole Study Group RAeport no. 1. Arch Ophthalmol 2004; 122: 224–236.
Acknowledgements
This study was supported by the NIHR Biomedical Research Centre for Ophthalmology at Moorfields and UCL Institute of Ophthalmology.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Eye website
Supplementary information
Rights and permissions
About this article
Cite this article
Lange, C., Membrey, L., Ahmad, N. et al. Pilot randomised controlled trial of face-down positioning following macular hole surgery. Eye 26, 272–277 (2012). https://doi.org/10.1038/eye.2011.221
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2011.221
Keywords
This article is cited by
-
Macular hole surgery recovery with and without face-down posturing: a meta-analysis of randomized controlled trials
BMC Ophthalmology (2019)
-
Comparison of face-down posturing with nonsupine posturing after macular hole surgery: a meta-analysis
BMC Ophthalmology (2019)
-
Adherence to face-down and non-supine positioning after macular hole surgery
BMC Ophthalmology (2018)
-
Adherence to the face-down positioning after vitrectomy and gas tamponade: a time series analysis
BMC Research Notes (2018)
-
Positioning In Macular hole Surgery (PIMS): statistical analysis plan for a randomised controlled trial
Trials (2017)