Abstract
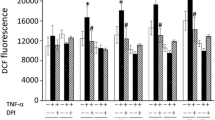
Cytokines such as tumor necrosis factor α (TNFα) and Interleukin-1α (IL1α) are known to influence energy metabolism and mitochondrial function in tumor and vascular smooth muscle cells. The aim of the present study was to investigate whether in cardiomyocytes mitochondrial function and PDH activity may also be impaired by TNFα and IL1α. Pyruvate dehydrogenase (PDH) activity and mitochondrial oxygen consumption of cultured cardiomyocytes were determined after subchronic exposure (24 h) to TNFα (1, 10, 100, 1000 I.U./ml) and IL1α (0.1, 1, 10, 100 I.U./ ml).
TNFα- and IL1α- exposure of the cardiomyocytes resulted in a concentration dependent decrease of PDH activity up to 38%. In parallel, selective oxygen consumption of the respiratory chain complexes I (NADH:ubiquinone oxidoreductase) and II (succinate:ubiquinone oxidoreductase) decreased by up to 45%. Addition of the PDH activator dichloracetate (0.01 M) resulted in complete restoration of PDH activity but not of mitochondrial function. The results suggest a primary inhibition of the mitochondrial respiratory chain by TNFα and IL1α and a subsequent down regulation of PDH activity.
Similar content being viewed by others
References
Vincent JE, Roman A, De Backer D, Kahn RJ: Oxygen uptake/supply dependency. Am Rev Res Dis 142: 2–7, 1990
Bakker J, Coffernils M, Leon M, Griss P, Vincent JL: Blood lactate levels are superior to oxygen-derived variables in predicting outcome in human septic shock. Chest 99: 956–962, 1991
Boekstegers P, Weidenhöfer S, Pilz G, Werdan K: Peripheral oxygen availability within skeletal muscle in sepsis and septic shock: Comparison to limited infection and cardiogenic shock. Infection 19: 317–323, 1991
Boekstegers P, Weidenhöfer S, Kapsner T, Werdan K: Skeletal muscle partial pressure of oxygen in patients with sepsis. Crit Care Med 22: 640–650, 1994
Hotchkiss RS, Rust RS, Dence CS, Wasserman TH, Song SK, Hwang DR, Kral IE, Welch MJ: Evaluation of the role of cellular hypoxia in sepsis by the hypoxic marker [18F] fluoromisonidazole. Am J Physiol 261: R965–972, 1991
Jepson MM, Cox M, Bates PC, Rothwell NJ, Stock MJ, Cady EB, Millward DJ: Regional blood flow and skeletal muscle energy status in endotoxemic rats. Am J Physiol 252: E581–E587, 1987
Hotchkiss RS, Karl IE: Reevaluation of the role of cellular hypoxia and bioenergetic failure in sepsis. JAMA 267: 1503–1510, 1992
Tredget EE, Yu YM, Zhong S, Burini R, Okusawa S, Gelfand JA, Dinarello CA, Young VR, Burke JF: Role of interleukin-1 and tumor necrosis factor on energy metabolism in rabbits. Am J Physiol E760–E768, 1988
Taylor DJ, Faragher EB, Evanson JM: Inflammatory cytokines stimulate glucose uptake and glycolysis but reduce glucose oxidation in human dermal fibroblasts in vitro. Circ Shock 37: 105–110, 1992
Vary TC, Siegel HJ, Nakatani T, Sato T, Aoyama H: Effects of sepsis on activity of pyruvate dehydrogenase complex in skeletal muscle and liver. Am J Physiol 250: E634–E640, 1986
Vary TC, Siegel HJ, Zechnich A, Tall BD, Morris JG, Placko R, Jawor D: Pharmacological reversal of abnormal glucose regulation, BCAA utilisation, and muscle catabolism in sepsis by dichloroacetate. J Trauma 28: 1301–1311, 1988
Vary TC, Martin LF: Potentiation of decreased pyruvate dehydro-genase activity by inflammatory stimuli in sepsis. Circ Shock 39: 299–305, 1993
Geng Y, Hansson GK, Holme E: Interferon-γand tumor necrosis factor synergize to induce nitric oxide production and inhibit mitochondrial respiration in vascular smooth muscle cells. Circ Res 71: 1268–1276, 1992
Schulze-Osthoff K, Bakker AC, Vanhaesebroeck B, Beyaert R, Jacob WA, Fiers W: Cytotoxic activity of tumor necrosis factor is mediated by early damage of mitochondrial functions. Evidence for the involvement of mitochondrial radical generation. J Biol Chem 267: 5317–5324, 1992
Boekstegers P, Kainz I, Giehrl W, Peter W, Werdan K: Subchronic exposure of cardiomyocytes to low concentrations of tumor necrosis factor αattenuates the positive inotropic response not only to catecholamines but also to cardiac glycosides and high calcium concentrations. Mol Cell Biochem 156: 135–143, 1996
Werdan K, Erdmann E: Preparation and culture of embryonic and neonatal heart muscle cells: Modification of transport activity. Meth Enzymol 173: 634–662, 1989
Granger DL, Lehninger AL: Sites of inhibition of mitochondrial electron transport in macrophage-injured neoplastic cells. J Cell Biol 95: 527–535, 1982
Stadler J, Bentz BG, Harbrecht BG, Di Silvio M, Curran RD, Billiar TR, Hoffman RA, Simmons RL: Tumor necrosis factor alpha inhibits hepatocyte mitochondrial respiration. Ann Surg 216: 539–546, 1992
Seals JR, Jarett L: Activation of pyruvate dehydrogenase by direct addition of insulin to an isolated plasma membrane/mitochondria mixture: Evidence for generation of insulin's second messenger in a subcellular system. Proc Natl Acad Sci 77: 77–81, 1980
Ferreira J: The oxygen dependence of the mitochondrial respiration rate in ascites tumor cells. Eur J Biochem 207: 857–866, 1992
Noll T, De Groot H, Wissemann P: A computer-supported oxystat system maintaining steady-state O2 partial pressures and simultaneously monitoring O 2 up-take in biological systems. Biochem J 236: 765–769, 1986
Attwood PV, Keech DB: Pyruvate carboxylase. Curr Top Cell Reg 23: 1–55, 1984
Wieland OH: The mammalian pyruvate dehydrogenase complex: Structure and regulation. Rev Physiol Biochem Pharmacol 96: 123–170, 1983
Denton RM, Halestrap AP: Regulation of pyruvate metabolism in mammalian tissues. Essays in Biochem 15: 37–77, 1979
Behal RH, Buxton DB, Robertson JG, Olson MS: Regulation of the pyruvate dehydrogenase multienzyme complex. Annu Rev Nutr 13: 497–520, 1993
Boekstegers P, Pfeifer A, Peter W, Werdan K: Contractile dysfunction of 'reperfused' neonatal rat heart cells: A model for studying 'myocardial stunning' at the cellular level. Adv Exp Med Biol 317: 573–582, 1992
Hansford RG: Studies on the effects of coenzyme A-SH: Acetyl coenzyme A, nicotinamide adenine dinucleotide, reduced nicotinamide adenine dinucleotide and adenosine diphosphate: Adenosine triphos-phate ratios on the interconversion of active and inactive pyruvate dehydrogenase in isolated rat heart mitochondria. J Biol Chem 251: 5483–5489, 1976
Reed LJ, Damuni Z, Merryfield ML: Regulation of mammalian pyruvate and branched-chain a-ketoacid dehydrogenase complexes by phos-phorylation-dephosphorylation. Curr Top Cell Reg 2741–49, 1985
Pettit FH, Pelley JW, Reed LJ: Regulation of pyruvate debydrogenase kinase and phosphatase by acetyl-CoA/CoA and NADH/NAD+ ratios. Biochem Biophys Res Commun 65: 575–581, 1975
Barron JT, Parrillo JE: Production of lactic acid and energy metabolism in vascular smooth muscle: Effect of dichloroacetate. Am J Physiol 268: H713–H719, 1995
Zentella A, Manogue K, Cerami A: Cachectin/TNF-mediated lactate production in cultured myocytes is linked to activation of a futile substrate cycle. Cytokine 5(5): 436–447, 1993
Stacpoole PW, Wright EC, Baumgartner TG, Bersin RM, Buchalter S, Curry SH, Duncan CA, Harman EM, Henderson GN, Jenkinson S, Lachin JM, Lorenz A, Schneider SH, Siegel JH, Summer WR, Thompson D, Wolfe CL, Zorovich B and the dichloroacetate lactic acidosis study group: A controlled trial of dichloroacetate for treatment of lactic acidosis in adults. N Engl J Med 327: 1564–1569, 1992
Schweizer M, Richter C: Nitric oxide potently and reversibly deenergizes mitochondria at low oxygen tension. Biochem Biophys Res Commun 204: 169–175, 1994
Werdan K, Müller-Werdan U, Reithmann C, Boekstegers P, Fuchs R, Kainz I, Stadler J: Nitric oxide dependent and independent effects of tumor necrosis factor-αon cardiomyocyte beating activity and signal transduction pathways. In: G Schlag, H Redl (eds). Shock, Sepsis and Organ Failure – Nitric Oxide. Fourth Wiggers Bernard Conference 1994. Springer Verlag, 1995
Vemuri R, Heller M, Pinson A: Studies of oxygen and volume restriction in cultured cardiac cells. II. The glucose effect. Bas Res Cardiol 80 (Suppl 2): 165–169, 1985
Schwartz P, Piper HM, Spahr R, Spieckermann PG: Ultrastructure of cultured adult myocardial cells during anoxia and reoxygenation. Am J Pathol 115: 349–361, 1984
Suffredini AF, Fromm RE, Parker MM, Brenner M, Kovacs JA, Wesley RA: The cardiovascular response of normal humans to administration of endotoxin. N Eng J Med 321: 280–287, 1989
Mitchie, HR, Manogue KR, Springs DR et al.: Detection of circulating tumor necrosis factor after endotoxin administration. N Eng J Med 318: 1481–1490, 1988
Parillo JE: Septic shock in humans: Advances in the understanding of pathogenesis, cardiovascular dysfunction, and therapy. Ann Int Med 113: 227–242, 1990
Cunnion RE, Schaer GL, Parker MM, Natanson C, Parillo JE: The coronary circulation in human septic shock. Circulation 73: 637–644, 1986
Hotchkiss RS, Song SK, Neil JJ, Chen RD, Manchester JK, Karl IE, Lowry OH, Ackerman JJ: Sepsis does not impair tricarboxylic acid cycle in the heart. Am J Physiol 260: C50–C57, 1991
Astiz ME, Rackow EC, Kaufmann B, Falk JL, Weil MH: Relationship of oxygen delivery and mixed venous oxygenation to lactic acidosis in patients with sepsis and acute myocardial infarction. Crit Care Med 16: 655–658, 1988
Padahno P, Gardinali M, Catania A, Vesconi S, Conciato L, Manfredi MG, Chiara O, Nielsen L, Nespoh A, Agostini A: Tumor necrosis factor and soluble tumor necrosis factor receptor I in multiple organ dysfunction syndrome. In: E Faist, AE Baue, FW Schildberg (eds). The Immune Consequences of Trauma, Shock and Sepsis. Mechanisms and Therapeutic Approaches. Pabst Science Publishers. Vol I, 1996, pp 368–377
Delogu G, Marandola M, Paoletti F, Marano M, Trinchieri V, De Simone C: Critically ill patients with gram-negative sepsis have increased levels of Interleukin-6 and-8 but not of interleukin-1. In: E Faist, AE Baue, FW Schildberg (eds). The Immune Consequences of Trauma, Shock and Sepsis. Mechanisms and Therapeutic Approaches. Pabst Science Publishers. Vol I, 1996, pp 378–384
Reinhart, K, Wiegand-Löhnert C, Grimminger F, Kaul M, Withington S, Treacher D, Eckart J, Willatts S, Bouza C, Krausch D, Stockenhuber F, Eiselstein J, Daum L, Kempeni J, and the MAK 195F sepsis study group: Assessment of the safety and efficacy of the monoclonal anti-tumor necrosis factor antibody-fragment, MAK 195F, in patients with sepsis and septic shock: A multicenter, randomized, placebo-controlled, dose-ranging study. Crit Care Med 24: 733–742, 1996
Boekstegers P, Weidenhöfer S, Zell R, Holler E, Kapsner T, Redl H, Schlag G, Kaul M, Kempeni J, Werdan K: Changes in skeletal muscle pO2 after administration of anti-TNFα-antibody in patients with severe sepsis: Comparison to Interleukin-6 serum levels, APACHE II, and Elebute scores. Shock 1: 246–253, 1994
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Zell, R., Geck, P., Werdan, K. et al. Tnf-α and IL-1α inhibit both pyruvate dehydrogenase activity and mitochondrial function in cardiomyocytes: Evidence for primary impairment of mitochondrial function. Mol Cell Biochem 177, 61–67 (1997). https://doi.org/10.1023/A:1006896832582
Issue Date:
DOI: https://doi.org/10.1023/A:1006896832582