Abstract
An understanding of the role of the prefrontal cortex in normal cognitive processes has advanced our comprehension of the pathophysiology underlying the cognitive deficits in schizophrenia. Studies of single-neuron activity in monkeys during performance of delayed-response tasks have confirmed the involvement of the prefrontal cortex in working memory. The “memory fields” of prefrontal neurons are analogous to the receptive fields of visual neurons and the cellular expression of a working memory process that allows mnemonic information to guide behavior. D1-dopamine antagonists produce a dose-dependent effect (U-shaped) on the firing rate of cells with memory fields during delayed-response tasks. Disordered cognitive processes in schizophrenia can be attributed to impairment of function in the prefrontal cortex, as evidenced by hypometabolic activity in the prefrontal cortex and selective impairment in working memory tasks. Advances in our understanding of the role of D1 receptors in the cognitive deficits observed in schizophrenia should provide us with a rational basis for developing alternative antipsychotic treatments and may provide insight into the cellular basis of the disorder.
Similar content being viewed by others
THE ROLE OF THE PREFRONTAL CORTEX IN SCHIZOPHRENIA
A number of the characteristic symptoms of schizophrenia, including the disorganization in thought and behavior, may be explained by a deficiency in working memory (Goldman-Rakic 1991; Goldman-Rakic and Selemon 1997). The role of the cortex in establishing internal representations of the outside world is well known, and the use of a computational workspace to recall and manipulate information is integral to storage and processing functions of the brain. The working memory dysfunction, or disruption in “on line” thought processing, that is evident in cognitive disturbances of schizophrenia has been ascribed to cellular mechanisms intrinsic to the prefrontal cortex (Goldman-Rakic 1995).
The importance of the prefrontal cortex in cognition and the cognitive deficits observed in schizophrenia is supported by neuropsychological and neurophysiological studies (Goldberg et al. 1993; Levin 1984; Merriam et al. 1990; Morihisa et al. 1983; Weinberger et al. 1986, 1988; Wolkin et al. 1988). Schizophrenic patients perform poorly on prefrontal cortex-mediated tasks that involve working memory (Park and Holzman 1992; Wexler et al. 1999). These tasks require that the subject retains knowledge of the information provided by an environmental cue in order to perform the appropriate behavioral response some time after the cue has been removed (Goldman-Rakic 1987). In monkeys, the spatial delayed-response task is used to study working memory. In this task, the monkey is required to hold in working memory the spatial location of an environmental cue during a delay period following removal of the cue. Performance of spatial delayed-response tasks involves the dorsolateral prefrontal cortex in humans (Freedman and Oscar-Berman 1986; Verin et al. 1993) and nonhuman primates (Friedman and Goldman-Rakic 1994; Goldman et al. 1971; Funahashi et al. 1989; Fuster and Alexander 1971; Verin et al. 1993).
Studies of single-neuron activity in monkeys during performance of delayed-response tasks have confirmed the involvement of the prefrontal cortex in working memory (Batuev et al. 1981, 1985; Funahashi et al. 1986; Fuster 1973; Fuster and Alexander 1971; Fuster et al. 1982; Joseph and Barone 1987; Kojima and Goldman-Rakic 1982, 1984; Niki and Watanabe 1976). Neurons that serve an important function in working memory typically display an increase in discharge rate after cue presentation and sustained activity during the delay period until the response is executed (Batuev et al. 1985; Funahashi et al. 1986; Fuster and Alexander 1971; Niki and Watanabe 1976). When errors occur in a task that is dependent on working memory function, they are associated with a failure of the corresponding neurons to maintain delay period activity. Delay period activity of prefrontal neurons codes the spatial coordinates of visual cues during a delayed-response task and provides a mnemonic code for direction over the full perimeter of visual space. These neuronal “memory fields” are analogous to the receptive fields of visual neurons and the cellular expression of a working memory process that allows mnemonic information to guide behavior (Funahashi et al. 1989).
The involvement of the prefrontal cortex in schizophrenia is supported by studies designed to probe morphologic differences between schizophrenic and normal brains. The activities of the prefrontal cortex necessarily involve interactions within a complex array of related areas (Goldman-Rakic 1988a, 1988b; Goldman-Rakic et al. 1993; Selemon and Goldman-Rakic 1988). Early attempts to identify neuropathologic features of the brains of schizophrenic patients did not lead to the identification of one specific neural abnormality (Andreasen 1988). However, quantitative neuroanatomical studies during the past two decades, using computerized positron emission tomography (PET), magnetic resonance imaging (MRI), and other modern techniques, have begun to converge on subtle abnormalities in a variety of key areas in the schizophrenic brain. Brain regions reported to be abnormal in schizophrenics include the hippocampus (Suddath et al. 1990), amygdala (Rossi et al. 1994; Shenton et al. 1992), entorhinal cortex (Arnold et al. 1991; Honer et al. 1996), cingulate cortex (Benes et al. 1992), planum temporale (Petty et al. 1995), mediodorsal thalamic nucleus (Andreasen et al. 1994; Pakkenberg 1990), and nucleus accumbens (Pakkenberg 1990). Enlarged ventricular spaces and smaller cortical volumes also have been observed (Cannon and Marco 1994; Weinberger et al. 1983). Many of the brain regions identified as structurally abnormal in schizophrenics have connections with either the prefrontal cortex or the nucleus accumbens, or both (O'Donnell and Grace 1998).
The importance of the prefrontal cortex in schizophrenia is supported by PET and dynamic single-photon emission computed tomography (D-SPECT) studies that have assessed the metabolic characteristics and/or blood perfusion of the prefrontal cortex in schizophrenic patients during performance of behavioral tasks (Ariel et al. 1983; Berman et al. 1986; Buchsbaum et al. 1984; Farkas et al. 1984; Kurachi et al. 1985; Liddle et al. 1992; Paulman et al. 1990; Volkow et al. 1987; Weinberger et al. 1986, 1988; Wolkin et al. 1988). In 1986, Weinberger et al. observed that schizophrenic patients failed to show an increase in regional cerebral blood flow (rCBF) in the dorsolateral prefrontal cortex while performing the Wisconsin Card Sorting Test (WCST), a measure of frontal lobe neuropsychological function (Weinberger et al. 1986). In a more recent study by Paulman et al. (1990), D-SPECT was conducted to assess regional and hemispheric rCBF in 40 chronic male schizophrenics (20 medicated and 20 unmedicated) and 31 gender- and age-matched healthy controls during performance of the WCST and the Luria–Nebraska Battery. Consistent with Weinberger et al. (1986), the results confirmed a deficit in bilateral frontal rCBF in male schizophrenic patients at rest and during the WCST; frontal flow deficits were most prominent in paranoid patients, and right temporal deficits were most prominent in nonparanoid patients. This study also extended previous findings by showing that reduced left frontal rCBF was associated with neuropsychological impairment on the WCST and the Luria–Nebraska Battery. In addition, increased hemispheric CBF was correlated with the presence of positive schizophrenic symptoms (Paulman et al. 1990). In summary, the evidence for compromised metabolism and blood flow in schizophrenia now seems incontrovertible.
Cell counting and planimetric analyses have now also identified regions of cell loss and cortical volume changes in schizophrenic patients (Benes 1993; Bogerts 1993; Heckers 1997; Shapiro 1993), although definitive evidence for cell loss has been presented only in a limited number of studies (Selemon and Goldman-Rakic 1999). The schizophrenic cortex is normal in appearance, and lesions such as those found in classic neurodegenerative disorders (e.g., Huntington's disease) are not present. Recent morphometric studies of the dorsolateral prefrontal cortex, however, reveal a pathologic condition in the schizophrenic brain that is characterized by an impoverished neuronal connectivity (Rajkowska et al. 1998; Selemon et al. 1995, 1998). With the application of a direct three-dimensional (3-D) counting technique (Williams and Rakic 1988), neuronal densities in prefrontal area 9 and visual cortical area 17 were calculated to be 17% and 10% higher in brains from schizophrenic patients as compared with healthy controls (Selemon et al. 1995). When measurements were made in prefrontal area 46, a 21% increase in density was measured in schizophrenic brains (Selemon et al. 1998). Based on a model in which the distance between neurons is diminished without a change in the number of neurons, we proposed the “reduced neuropil hypothesis” to relate prefrontal cognitive disturbances to atrophy of neuronal processes, without actual neuronal loss (Selemon and Goldman-Rakic 1999). Collectively, the results of these studies suggest that a reduced neuropil form of pathology may occur over widespread regions in the schizophrenic cortex (Selemon et al. 1995, 1998).
THE DOPAMINE HYPOTHESIS OF SCHIZOPHRENIA AND DOPAMINE SYSTEMS
Dopamine (DA)-responsive systems have been implicated in schizophrenia, tardive dyskinesia, Parkinson's disease, Tourette's syndrome, hyperprolactinemia, and possibly Huntington's disease (Gingrich and Caron 1993). There are two major dopaminergic systems in the brain, the mesolimbic and the nigrostriatal. The mesolimbic dopamine system is involved in cognition and modulation of reward and consists of projections from the ventral tegmental area (VTA) to the nucleus accumbens (mesolimbic) and to the cortex (mesocortical). The nigrostriatal dopamine system is primarily involved in modulation of motor behaviors and consists of ascending projections from the substantia nigra (SN) to the striatum (caudate nucleus and putamen) (Role and Kelly 1991). As originally formulated, the DA hypothesis of schizophrenia postulated that increased DA activity (possibly in the mesolimbic system) was the cause of symptoms (Matthysse 1973; Meltzer and Stahl 1976). However, the negative symptoms of schizophrenia, including flattening of affect, anhedonia, anergia or psychomotor retardation, and cognitive deficits, are associated with hypoactivity in the prefrontal cortex DA system. In fact, improvements in negative symptoms have been noted in some patients treated with DA agonists (Angrist et al. 1980, 1982; Sanfilipo et al. 1996), and modifications of the hypothesis have been necessary to address the pathophysiology of negative symptoms (MacKay 1980; Meltzer 1979).
Knowledge of the structure and function of dopamine receptors has increased substantially in recent years with the application of techniques from molecular biology (Gingrich and Caron 1993). Cloning of the 5 mammalian DA-receptor subtypes and development of subtype-specific ligands has facilitated the investigation of the role of DA in cognitive processes and schizophrenia. These five receptor subtypes can be broadly classified into the D1 and D2 families; the D1 family includes the D1 and D5 subtypes, and the D2 family includes the D2, D3, and D4 subtypes (Seeman and Van Tol 1994).
In general, D1, D2, and D3 receptors are prominent in subcortical regions, D4 receptors are distributed in both limbic and cortical regions, and D1 and D5 receptors are relatively more prominent in striatum and cortex than in brain stem nuclei (Meador-Woodruff et al. 1996). The distribution of D2 receptors is clinically significant, because the antipsychotic efficacy of classic neuroleptics has been correlated with their degree of activity at D2 receptors (Creese et al. 1976; Seeman et al. 1976). D2-receptor subtype distribution has been examined in an autoradiographic study of postmortem human brain tissue using the specific D2 agonist [3H]CV 205-502 and the antagonist [3H]spiroperidol (Camps et al. 1989). High densities of both ligands were observed in the caudate nucleus and putamen (striatum), nucleus accumbens, olfactory tubercle, and the substantia nigra pars compacta. Lower densities were observed in the globus pallidus and hippocampus. Negligible amounts of binding were observed in the olfactory bulb, diencephalon, brainstem, cerebellum, and neocortex. A strong correlation was observed between the anatomical distribution of D2 receptors and reported regional endogenous dopamine concentrations (Camps et al. 1989). Receptor-binding assays with the selective D2 antagonist [3H]-raclopride (Lidow et al. 1989) have shown similar results, with lower concentrations of D2-receptor binding sites observed in the cortex as compared to the striatum.
D1 receptors recently have been proposed to play an important role in the pathophysiology of schizophrenia (Lynch 1992). Recent studies using antagonists and agonists selective for the D1 receptor have shown differences in the distribution of D1 receptors in schizophrenic patients as compared with healthy controls (the reader is referred to Sedvall et al. in this issue for a review of PET and audioradiography localization studies in schizophrenic patients). For example, decreased D1-receptor binding has been observed in the prefrontal cortex of drug-naive schizophrenic patients, with the reduction in prefrontal D1 receptors correlated with the severity of negative symptoms and cognitive disturbances (Okubo et al. 1997).
D1 RECEPTORS IN PREFRONTAL CORTEX
Dopaminergic innervation of the cerebral cortex is well-documented (Berger et al. 1986; Brown et al. 1979; Kehr et al. 1976). Radiolabeled ligands have been used to determine the distributions of the D1- and D2-receptor subtypes within the prefrontal cortex in studies of in vitro receptor binding (Camps et al. 1989; Cortés et al. 1989; Goldman-Rakic et al. 1990; Hall et al. 1988; Lidow et al. 1989; Richfield et al. 1989) and in vivo PET (Farde et al. 1987, 1988). In studies using the D1-receptor antagonist [3H]SCH 23390 and the D2-receptor antagonist [3H]raclopride, or [3H]SCH 23390 and [3H]spiperone in the presence of mianserin (to block labeling of 5-HT2A and 5-HT2C sites), a low density of [3H]raclopride (D2 receptors) binding was observed in all layers of the cortical areas studied. The highest densities of [3H]-raclopride binding were observed in layer V of frontal, parietal, and occipital lobes. The density of binding for D1 receptors with [3H]SCH 23390 was 10 to 20 times higher than D2-receptor density in all cortical areas, including the prefrontal cortex (Figure 1 ). Both [3H]SCH 23390 and [3H]raclopride binding sites display a rostral-caudal gradient, with the highest concentrations observed in the prefrontal cortex and the lowest concentrations in the occipital cortex (Lidow et al. 1989, 1991).
Histogram comparing layer-by-layer distribution of D1-specific [3H]SCH 22390 binding sites to D2-specific [3H]raclopride binding sites in area 46 of prefrontal cortex in the rhesus monkey (From data shown in Goldman-Rakic et al. 1990)
Ligands specific for various subtypes of dopaminergic, adrenergic, and serotonergic receptors have allowed us to observe distinctive laminar-specific distributions for monoamine receptors in the cerebral cortex. Although there is overlap among the dopaminergic, adrenergic, and serotonergic receptors, subtypes within the same receptor class tend to have complementary laminar profiles and even different localizations where cellular compartments (Goldman-Rakic et al. 1996; (Goldman-Rakic et al. 1990). Similar studies using [3H]SCH 23390 in post-mortem human brain tissue have confirmed a laminar cortical distribution of D1 receptors (Cortés et al. 1989). Interestingly, multivariate analysis demonstrated that advancing age is correlated with a marked decrease in the density of D1 receptors in human brains (Cortés et al. 1989).
D1 receptor-specific antibodies have been used in immunohistochemical studies to characterize the distribution of the D1 receptors in the primate prefrontal cortex at the resolution of light and electron microscopy (Smiley et al. 1994). D1-immunoreactive neurons are observed in all cortical layers, but are particularly visible in layers II, III, and V (Bergson et al. 1995). In addition, D1 receptors are associated with pyramidal neurons, often in cell dendrites and spines (Figure 2 ) (Smiley et al. 1994). Similar to the distribution of D1-binding sites observed in autoradiographic studies, a bilaminar distribution (layers 1b-II and V-VI) of neurophil labeling is also observed. Electron microscopic analysis reveals that D1 receptors are frequently located postsynaptically in the prefrontal cortex, although presynaptic sites are also observed. When localized presynaptically, D1 receptors are often observed in axon terminals that form asymmetric synaptic specializations. Double-label localization experiments demonstrate coexpression of D1 and D5 receptors within neurons of both the neocortex and the hippocampus. Ultrastructurally, D1-antibody staining is prominent in spines; whereas, D5-antibody staining is dominant in dendritic shafts (Bergson et al. 1995).
Diagrammatic representation of a cortical pyramidal cell indicating the relative location of D1 receptors on the shafts and spines at distal portions of the basilar and apical dendritic tree. The photomicrograph shows an unidentified axon (Ax) of the asymmetric (excitatory) type terminating on a D1-containing spine (Sp) as revealed by the dark label in the spine produced by immunocytochemical response to a D1-specific antibody (photomicrograph courtesy of E. Christopher Muly and P.S. Goldman-Rakic)
Three possible cellular mechanisms of DA modulation of working memory function seem to operate in the prefrontal cortex (Goldman-Rakic 1998). One mechanism is direct nonsynaptic modulation of pyramidal neurons. The second mechanism is indirect synaptic modulation of pyramidal neurons via feedforward inhibition from GABAergic interneurons. The third possible mechanism is direct synaptic modulation of receptors on the distal dendrites and spines of pyramidal neurons. Synaptic triad complexes have been observed in the prefrontal cortex in which the spines of a pyramidal neuron receive input from both a dopamine terminal and a glutamate terminal. This triad suggests dopamine modulation of excitatory input on pyramidal neurons that project to the thalamus, the striatum, and to other areas of the cortex (Goldman-Rakic 1998). Although the receptors involved in these triads have not been identified, electrophysiological studies from our laboratory (discussed in detail below) indicate that the D1 receptor may be involved in regulating excitatory neurotransmission in the prefrontal cortex (Williams and Goldman-Rakic 1995).
THE INVOLVEMENT OF D1 RECEPTORS IN MEMORY AND COGNITION
Although the normally low concentrations of D2 receptors and high concentrations of D1 receptors present in the prefrontal cortex suggest the involvement of the D1 receptor in mnemonic processes, additional evidence to support this hypothesis comes from experiments with the potent D1 antagonists SCH 23390 and SCH 39166 (Chipkin et al. 1988). In these experiments, SCH 23390 and SCH39166 were injected into several areas of the prefrontal cortex of rhesus monkeys and an oculomotor delayed-response (ODR) task was used to monitor their effects on working memory (Sawaguchi and Goldman-Rakic 1991). The D1 antagonists induced errors and increased the latency of response during the performance of the ODR task, which required memory-guided saccades; these deficits were dose-dependent and delay period sensitive. Performance on a control task requiring visually guided saccades showed that the D1 antagonists had no effects on sensory or motor functions. These results suggest that activation of D1 receptors is critical for memory processes mediated by the prefrontal cortex, although the specific types of neurons affected by the D1 antagonists were not determined.
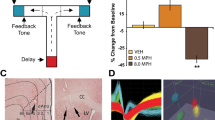
Iontophoresis of drugs onto neurons in conjunction with single-cell recording of neural activity during behavior is now possible (Funahashi et al. 1989, 1990; Williams and Goldman-Rakic 1995). Using this technology, the involvement of D1 receptors in mnemonic processes of the prefrontal cortex has been tested. Williams and Goldman-Rakic (1995) examined the effects of SCH 39166 on cell firing in the dorsolateral prefrontal cortex of monkeys while they performed an ODR task (Williams and Goldman-Rakic 1995). Consistent with previous findings, spatially tuned memory fields were observed in prefrontal neurons; that is, neurons responded maximally during the delay period for targets in one or a few adjacent target locations. However, in contrast to our previous finding that D1 antagonists were detrimental to working memory (Sawaguchi and Goldman-Rakic 1991), iontophoresis of SCH 39166 enhanced the neuronal memory fields in 11 of 12 neurons. Similar results were obtained with the less selective D1 antagonists, SCH 23390, NNC 010756, and A 60924 (Williams and Goldman-Rakic 1995). The neuronal memory field activation caused by D1-receptor blockade could be reversed by iontophoresis of the partial D1 agonist, SKF 38393. The D2-receptor antagonist, raclopride, caused a generalized inhibition of firing without the selective effects on neuronal memory fields observed with D1-specific agents. In this study, an increased activation of memory fields of prefrontal neurons was achieved only through D1-receptor activation, suggesting a memory-enhancing action at the doses used (Williams and Goldman-Rakic 1995).
Another important observation in this study was the dose dependence of D1-antagonist effects. At high doses, D1 antagonists caused a nonspecific inhibition of cell firing, affecting not only the memory field of the cells but neuronal activity during all phases of the ODR task and at all target locations. The dose-related effects observed at the cellular level are consistent with the results of other physiological and behavioral studies (Arnsten et al. 1994; Cai and Arnsten 1997; Hu and Wang 1988; Murphy et al. 1996). The dependence of working memory on D1-receptor activation is a “U-shaped” function, where the optimal range of dopamine concentrations and cortical receptor activation characterizes the state of normal cognitive performance. Currently available antipsychotic agents consistently are not effective in treating the negative symptoms and cognitive deficits of schizophrenia (Angrist et al. 1980; Meltzer et al. 1994). The results of the Williams and Goldman-Rakic (1995) study raise the possibility that antipsychotic medications may have unforeseen effects on D1- and D2-receptor levels, causing the D1-receptor levels to fall outside of the optimal range. Additional studies of the effects of D1-specific agonists and antagonists on working memory function are in progress.
D1 Receptors and Antipsychotics
Long-term exposure (≥6 months) to typical antipsychotic drugs (D2 antagonists) increases the level of D2 receptors and produces a downregulation of D1 receptors in primate cerebral cortex (Figure 3 ) (Lidow and Goldman-Rakic 1994, 1997; Lidow et al. 1997; Nordström et al. 1992; Wolkin et al. 1989). The level of D2 receptors rises relatively quickly after the beginning of exposure (Nordström et al. 1992; Wolkin et al. 1989); whereas, effects on cortical D1 receptors are slower to appear. D1 and D5 receptors are both subject to this downregulation (Lidow et al. 1997), which occurs at a detectable level only after months of exposure to antipsychotic drugs. The mechanism by which D2 antagonists reduce cortical D1- and D5-receptor levels is not known (Lidow et al. 1998).
Bar graphs representing changes in the levels of D2-long (L), D2-short (S)2, D1 and D5 mRNAs in response to 6 months of daily treatment with nine pharmacologically distinct drugs but common D2 antagonist properties. The bar graphs represent mean dopamine receptor mRNA expressed per β-actin mRNA ± (standard error of the mean) with the mean ratio for the drug-free control group designated as one and the remainder of the data normalized accordingly (adapted from Lidow and Goldman-Rakic 1997; Lidow et al. 1998)
We are currently studying the effects of a D1-receptor agonist (ABT-431, Abbott) on working memory (ODR task) in primates that have had long-term neuroleptic treatment. To date, the results are encouraging. Whether or not D1 or D2 receptors are involved in the primary pathophysiology of schizophrenia is still unknown (Goldman-Rakic and Selemon 1997). To the extent that maintaining receptor occupancy at a certain level is important to normal cognitive function, the use of appropriate doses of D1-receptor antagonists or agonists in a clinical trial setting is an important area of future study.
CONCLUSIONS
Schizophrenic patients manifest negative symptoms and cognitive deficits throughout the course of their illness, and these symptoms tend to be more constant than positive symptoms such as hallucinations and delusions, which are more episodic in nature (Weinberger 1988). These deficit symptoms include emotional dullness; impaired judgement; poor initiative, motivation, or drive; lack of insight; difficulty in planning; impaired problem solving and abstract reasoning; decreased concern for personal hygiene; and social withdrawal. Neuropsychological and neurophysiological studies confirm the importance of the prefrontal cortex in cognition and in cognitive deficits observed in schizophrenia.
Studies of single-neuron activity in monkeys during performance of delayed-response tasks have confirmed the involvement of the prefrontal cortex in working memory. Separate populations of neurons have been identified whose activity is temporally linked to specific components of the delayed-response task (Fuster et al. 1982). One type of neuronal population, called a “memory field,” seems to be associated with maintaining the representation of the environmental cue during the delay between cue presentation and behavior. There is evidence that D1 receptors in the prefrontal cortex are involved in working memory. D1 antagonists, administered to neurons via iontophoresis, produce a dose-dependent effect (U-shaped) on the firing rate of cells within memory fields during delayed-response tasks. At high doses, D1 antagonists cause a nonspecific inhibition of cell firing, affecting not only the memory field of the cells but also the neuronal activity during all phases of the delayed-response task and all target locations. However, at lower doses, D1 antagonists produce a delay-specific enhancement of cell firing within memory fields.
Disordered cognitive processes in schizophrenia can be attributed to impairment of function in the prefrontal cortex. The schizophrenic brain is normal in gross appearance, and the types of lesions observed in neurodegenerative disorders such as Huntington's disease are not present (Selemon and Goldman-Rakic 1999). However, recent studies have shown increased neuronal density in the prefrontal and to a lesser extent in the occipital cortices of schizophrenics as compared to healthy controls (Selemon et al. 1998). This increased neuronal density characterizes the more subtle pathology of schizophrenia, presumably indicating a compromised cell structure, impoverished neural connectivity, and loss of functional interneuron communication.
Direct evidence of prefrontal dysfunction in schizophrenia comes from studies using physiological brain imaging techniques. Schizophrenic patients show an inability to learn how to perform the WCST (Goldberg et al. 1987) and reduced activation of dorsolateral prefrontal cortex while engaged in the WCST (Weinberger et al. 1986). Schizophrenic subjects also show significant impairments on oculomotor delayed-response tasks (Park and Holzman 1992), a behavioral paradigm that has been demonstrated to be a selective and reliable measure of dorsolateral prefrontal cortex function. Furthermore, the degree of prefrontal hypometabolism has been correlated with clinical ratings of negative symptoms.
Although the involvement of dopamine D2 receptors in schizophrenia has been studied extensively because typical antipsychotics are D2 antagonists, recently, more attention has been focused on the role of D1 receptors in schizophrenia. Autoradiographic and PET studies have determined that there is a high density of D1 receptors compared with D2 receptors in the prefrontal cortex; this density is altered in schizophrenic patients. Increasingly, more detailed information is becoming available concerning the localization of D1 receptors and their involvement in cognition and schizophrenia. Further characterization of D1 receptors in the prefrontal cortex should lead to additional insights on the neuropharmacology of cognition as well as on effective treatments for schizophrenia.
References
Andreasen NC, Arndt S, Swayze V II, Cizadlo T, Flaum M, O'Leary D, Ehrhardt JC, Yuh WTC . (1994): Thalamic abnormalities in schizophrenia visualized through magnetic resonance image averaging. Science 266: 294–298
Andreasen NC . (1988): Brain imaging: Applications in psychiatry. Science 239: 1381–1388
Angrist B, Peselow E, Rubinstein M, Corwin J, Rotrosen J . (1982): Partial improvement in negative schizophrenic symptoms after amphetamine. Psychopharmacology 78: 128–130
Angrist B, Rotrosen J, Gershon S . (1980): Differential effects of amphetamine and neuroleptics on negative vs. positive symptoms in schizophrenia. Psychopharmacology 72: 17–19
Ariel RN, Golden CJ, Berg RA, Quaife MA, Dirkson JW, Forsell T, Wilson J, Graber B . (1983): Regional cerebral blood flow in schizophrenics. Tests using the Xenon Xe 133 inhalation method. Arch Gen Psychiat 40: 258–263
Arnold SE, Hyman BT, Van Hoesen GW, Damasio AR . (1991): Some cytoarchitectural abnormalities of the entorhinal cortex in schizophrenia. Arch Gen Psychiat 48: 625–632
Arnsten AFT, Cai JX, Murphy BL, Goldman-Rakic PS . (1994): Dopamine D1 receptor mechanisms in the cognitive performance of young adult and aged monkeys. Psychopharmacology 116: 143–151
Batuev AS, Orlov AA, Pirogov AA . (1981): Short-term spatiotemporal memory and cortical unit reactions in the monkey. Acta Physiol Acad Sci Hung 58: 207–216
Batuev AS, Shaefer VI, Orlov AA . (1985): Comparative characteristics of unit activity in the prefrontal and parietal areas during delayed performance in monkeys. Behav Brain Res 16: 57–70
Benes FM . (1993): Neurobiological investigations in cingulate cortex of schizophrenic brain. Schizophr Bull 19: 537–549
Benes FM, Vincent SL, Alsterberg G, Bird ED, SanGiovanni JP . (1992): Increased GABAA receptor binding in superficial layers of cingulate cortex in schizophrenics. J Neurosci 12: 924–929
Berger B, Trottier S, Gaspar P, Verney C, Alvarez C . (1986): Major dopamine innervation of the cortical motor areas in the cynomolgus monkey. A radioautographic study with comparative assessment of serotonergic afferents. Neurosci Lett 72: 121–127
Bergson C, Mrzljak L, Smiley JF, Pappy M, Levenson R, Goldman-Rakic PS . (1995): Regional, cellular, and subcellular variations in the distribution of D1 and D5 dopamine receptors in primate brain. J Neurosci 15: 7821–7836
Berman KF, Zec RF, Weinberger DR . (1986): Physiologic dysfunction of dorsolateral prefrontal cortex in schizophrenia: II. Role of neuroleptic treatment, attention, and mental effort. Arch Gen Psychiat 43: 126–135
Bogerts B . (1993): Recent advances in the neuropathology of schizophrenia. Schizophr Bull 19: 431–445
Brown RM, Crane AM, Goldman PS . (1979): Regional distribution of monoamines in the cerebral cortex and subcortical structures of the rhesus monkey: Concentrations and in vivo synthesis rates. Brain Res 168: 133–150
Buchsbaum MS, DeLisi LE, Holcomb HH, Cappelletti J, King AC, Johnson J, Hazlett E, Dowling-Zimmerman S, Post RM, Morihisa J, Carpenter W, Cohen R, Pickar D, Weinberger DR, Margolin R, Kessler RM . (1984): Anteroposterior gradients in cerebral glucose use in schizophrenia and affective disorders. Arch Gen Psychiat 41: 1159–1166
Cai JX, Arnsten AF . (1997): Dose-dependent effects of the dopamine D1 receptor agonists A77636 or SKF81297 on spatial working memory in aged monkeys. J Pharmacol Exp Ther 283: 183–189
Camps M, Cortés R, Gueye B, Probst A, Palacios JM . (1989): Dopamine receptors in human brain: Autoradiographic distribution of D2 sites. Neuroscience 28: 275–290
Cannon TD, Marco E . (1994): Structural brain abnormalities as indicators of vulnerability to schizophrenia. Schizophr Bull 20: 89–102
Chipkin RE, Iorio LC, Coffin VL, McQuade RD, Berger JG, Barnett A . (1988): Pharmacological profile of SCH39166: A dopamine D1 selective benzonaphthazepine with potential antipsychotic activity. J Pharmacol Exp Ther 247: 1093–1102
Cortés R, Gueye B, Pazos A, Probst A, Palacios JM . (1989): Dopamine receptors in human brain: Autoradiographic distribution of D1 sites. Neuroscience 28: 263–273
Creese I, Burt DR, Snyder SH . (1976): Dopamine receptor binding predicts clinical and pharmacological potencies of antischizophrenic drugs. Science 192: 481–483
Farde L, Halldin C, Stone-Elander S, Sedvall G . (1987): PET analysis of human dopamine receptor subtypes using 11C-SCH 23390 and 11C-raclopride. Psychopharmacology 92: 278–284
Farde L, Pauli S, Hall H, Eriksson L, Halldin C, Högberg T, Nilsson L, Sjögren I, Stone-Elander S . (1988): Stereoselective binding of 11C-raclopride in living human brain—A search for extrastriatal central D2-dopamine receptors by PET. Psychopharmacology 94: 471–478
Farkas T, Wolf AP, Jaeger J, Brodie JD, Christman DR, Fowler JS . (1984): Regional brain glucose metabolism in chronic schizophrenia. A positron emission transaxial tomographic study. Arch Gen Psychiat 41: 293–300
Freedman M, Oscar-Berman M . (1986): Bilateral frontal lobe disease and selective delayed response deficits in humans. Behav Neurosci 100: 337–342
Friedman HR, Goldman-Rakic PS . (1994): Coactivation of prefrontal cortex and inferior parietal cortex in working memory tasks revealed by 2DG functional mapping in the rhesus monkey. J Neurosci 14: 2775–2788
Funahashi S, Bruce CJ, Goldman-Rakic PS . (1990): Visuospatial coding in primate prefrontal neurons revealed by oculomotor paradigms. J Neurophysiol 63: 814–831
Funahashi S, Bruce CJ, Goldman-Rakic PS . (1989): Mnemonic coding of visual space in the monkey's dorsolateral prefrontal cortex. J Neurophysiol 61: 331–349
Funahashi S, Bruce CJ, Goldman-Rakic PS . (1986): Perimetry of spatial memory representation in primate prefrontal cortex: Evidence for mnemonic hemianopia. Soc Neurosci Abstr 12: 554
Fuster JM . (1973): Unit activity in prefrontal cortex during delayed-response performance: Neuronal correlates of transient memory. J Neurophysiol 36: 61–78
Fuster JM, Alexander GE . (1971): Neuron activity related to short-term memory. Science 173: 652–654
Fuster JM, Bauer RH, Jervey JP . (1982): Cellular discharge in the dorsolateral prefrontal cortex of the monkey in cognitive tasks. Exp Neurol 77: 679–694
Gingrich JA, Caron MG . (1993): Recent advances in the molecular biology of dopamine receptors. Ann Rev Neurosci 16: 299–321
Goldberg TE, Torrey EF, Gold JM, Ragland JD, Bigelow LB, Weinberger DR . (1993): Learning and memory in monozygotic twins discordant for schizophrenia. Psychol Med 23: 71–85
Goldberg TE, Weinberger DR, Berman KF, Pliskin NH, Podd MH . (1987): Further evidence for dementia of the prefrontal type in schizophrenia? Arch Gen Psychiat 44: 1008–1014
Goldman PS, Rosvold HE, Vest B, Galkin TW . (1971): Analysis of the delayed-alternation deficit produced by dorsolateral prefrontal lesions in the rhesus monkey. J Comp Physiol Psychol 77: 212–220
Goldman-Rakic PS . (1998): The cortical dopamine system: Role in memory and cognition. Adv Pharmacol 42: 707–711
Goldman-Rakic PS . (1995): Psychopathology and neuropathology of prefrontal cortex in schizophrenia. In Fog R, Gerlach J, Hemmingsen R (eds), Schizophrenia. Copenhagen, Denmark: Munksgaard, pp 126–136
Goldman-Rakic PS . (1994): Working memory dysfunction in schizophrenia. J Neuropsychiat 6: 348–357
Goldman-Rakic PS . (1988a): Topography of cognition: Parallel distributed networks in primate association cortex. Ann Rev Neurosci 11: 137–156
Goldman-Rakic PS . (1988b): Changing concepts of cortical connectivity: Parallel distributed cortical networks. In Rakic P, Singer W (eds), Neurobiology of Neocortex. New York: John Wiley & Sons, pp 177–202
Goldman-Rakic PS . (1987): Circuitry of the prefrontal cortex and the regulation of behavior by representational knowledge. In Plum F, Mountcastle V (eds), Handbook of Physiology, vol 5. Bethesda, Maryland: American Physiological Society, pp 373–417
Goldman-Rakic PS . (1991): Prefrontal Cortical Dysfunction in Schizophrenia: The Relevance of Working Memory. In Bernard J. Carroll and James E. Barrett (eds), Psychopathology and the Brain. American Psychopathological Association, Raven Press, New York, pp 1–23
Goldman-Rakic PS, Bergson C, Mrzljak L, Williams GV . (1996): Dopamine receptors and cognitive function in nonhuman primates. In Neve KA, Neve RL (eds), The Dopamine Receptors. Totowa, New Jersey: Humana Press, pp 499–522
Goldman-Rakic PS, Chafee M, Friedman H . (1993): Allocation of function in distributed circuits. In Ono T, Squire LR, Raichle ME, Perrett DI, Fukuda M (eds), Brain Mechanisms of Perception and Memory: From Neuron to Behavior. New York: Oxford University Press, pp 445–456
Goldman-Rakic PS, Lidow MS, Gallager DW . (1990): Overlap of dopaminergic, adrenergic, and serotoninergic receptors and complementarity of their subtypes in primate prefrontal cortex. J Neurosci 10: 2125–2138
Goldman-Rakic PS, Selemon LD . (1997): Functional and anatomical aspects of prefrontal pathology in schizophrenia. Schizophr Bull 23: 437–458
Hall H, Farde L, Sedvall G . (1988): Human dopamine receptor subtypes—In vitro binding analysis using 3H-SCH 23390 and 3H-raclopride. J Neural Transm 73: 7–21
Heckers S . (1997): Neuropathology of schizophrenia: Cortex, thalamus, basal ganglia, and neurotransmitter-specific projection systems. Schizophr Bull 23: 403–421
Honer WG, Bassett AS, Falkai P, Beach TG, Lapointe JS . (1996): A case study of temporal lobe development in familial schizophrenia. Psychol Med 26: 191–195
Hu XT, Wang RY . (1988): Comparison of effects of D-1 and D-2 dopamine receptor agonists on neurons in the rat caudate putamen: An electrophysiological study. J Neurosci 8: 4340–4348
Joseph JP, Barone P . (1987): Prefrontal unit activity during a delayed oculomotor task in the monkey. Exp Brain Res 67: 460–468
Kehr W, Lindqvist M, Carlsson A . (1976): Distribution of dopamine in the rat cerebral cortex. J Neural Transm 38: 173–180
Kojima S, Goldman-Rakic PS . (1984): Functional analysis of spatially discriminative neurons in prefrontal cortex of rhesus monkey. Brain Res 291: 229–240
Kojima S, Goldman-Rakic PS . (1982): Delay-related activity of prefrontal neurons in rhesus monkeys performing delayed response. Brain Res 248: 43–49
Kurachi M, Kobayashi K, Matsubara R, Hiramatsu H, Yamaguchi N, Matsuda H, Maeda T, Hisada K . (1985): Regional cerebral blood flow in schizophrenic disorders. Eur Neurol 24: 176–181
Levin S . (1984): Frontal lobe dysfunctions in schizophrenia—I. Eye movement impairments. J Psychiat Res 18: 27–55
Liddle PF, Friston KJ, Frith CD, Hirsch SR, Jones T, Frackowiak RSJ . (1992): Patterns of cerebral blood flow in schizophrenia. Br J Psychiat 160: 179–186
Lidow MS, Goldman-Rakic PS . (1997): Differential regulation of D2 and D4 dopamine receptor mRNAs in the primate cerebral cortex vs. neostriatum: Effects of chronic treatment with typical and atypical antipsychotic drugs. J Pharmacol Exp Ther 283: 939–946
Lidow MS, Elsworth JD, Goldman-Rakic PS . (1997): Down-regulation of the D1 and D5 dopamine receptors in the primate prefrontal cortex by chronic treatment with antipsychotic drugs. J Pharmacol Exp Ther 281: 597–603
Lidow MS, Goldman-Rakic PS . (1994): A common action of clozapine, haloperidol, and remoxipride on D1- and D2-dopaminergic receptors in the primate cerebral cortex. Proc Nat Acad Sci USA 91: 4353–4356
Lidow MS, Goldman-Rakic PS, Gallager DW, Rakic P . (1991): Distribution of dopaminergic receptors in the primate cerebral cortex: Quantitative autoradiographic analysis using [3H]raclopride, [3H]spiperone and [3H]SCH23390. Neuroscience 40: 657–671
Lidow MS, Goldman-Rakic PS, Rakic P, Innis RB . (1989): Dopamine D2 receptors in the cerebral cortex: distribution and pharmacological characterization with [3H]raclopride. Proc Nat Acad Sci USA 86: 6412–6416
Lidow MS, Williams GV, Goldman-Rakic PS . (1998): The cerebral cortex: A case for a common site of action of antipsychotics. TIPS 19: 136–140
Lynch MR . (1992): Schizophrenia and the D1 receptor: Focus on negative symptoms. Prog Neuropsychopharmacol Biol Psychiat 16: 797–832
MacKay AVP . (1980): Positive and negative schizophrenic symptoms and the role of dopamine. Br J Psychiat 137: 379–386
Matthysse S . (1973): Antipsychotic drug actions: A clue to the neuropathology of schizophrenia? Fed Proc 32: 200–205
Meador-Woodruff JH, Damask SP, Wang J, Haroutunian V, Davis KL, Watson SJ . (1996): Dopamine receptor mRNA expression in human striatum and neocortex. Neuropsychopharmacology 15: 17–29
Meltzer HY . (1979): Biochemical studies in schizophrenia. In Bellak L (ed), Disorders of the Schizophrenic Syndrome. New York: Basic Books, pp 45–149
Meltzer HY, Lee MA, Ranjan R . (1994): Recent advances in the pharmacotherapy of schizophrenia. Acta Psychiat Scand 90: 95–101
Meltzer HY, Stahl SM . (1976): The dopamine hypothesis of schizophrenia. Schizophr Bull 2: 19–76
Merriam AE, Kay SR, Opler LA, Kushner SF, van Praag HM . (1990): Neurological signs and the positive–negative dimension in schizophrenia. Biol Psychiat 28: 181–192
Morihisa JM, Duffy FH, Wyatt RJ . (1983): Brain electrical activity mapping (BEAM) in schizophrenic patients. Arch Gen Psychiat 40: 719–728
Murphy BL, Arnsten AF, Goldman-Rakic PS, Roth RH . (1996): Increased dopamine turnover in the prefrontal cortex impairs spatial working memory performance in rats and monkeys. Proc Nat Acad Sci USA 93: 1325–1329
Niki H, Watanabe M . (1976): Prefrontal unit activity and delayed response: Relation to cue location versus direction of response. Brain Res 105: 79–88
Nordström A-L, Farde L, Halldin C . (1992): Time course of D2-dopamine receptor occupancy examined by PET after single oral doses of haloperidol. Psychopharmacology 106: 433–438
O'Donnell P, Grace AA . (1998): Dysfunctions in multiple interrelated systems as the neurobiological bases of schizophrenic symptom clusters. Schizophr Bull 24: 267–283
Okubo Y, Suhara T, Suzuki K, Kobayashi K, Inoue O, Terasaki O, Someya Y, Sassa T, Sudo Y, Matsushima E, Iyo M, Tateno Y, Toru M . (1997): Decreased prefrontal dopamine D1 receptors in schizophrenia revealed by PET. Nature 385: 634–636
Pakkenberg B . (1990): Pronounced reduction of total neuron number in mediodorsal thalamic nucleus and nucleus accumbens in schizophrenics. Arch Gen Psychiat 47: 1023–1028
Park S, Holzman PS . (1992): Schizophrenics show spatial working memory deficits. Arch Gen Psychiat 49: 975–982
Paulman RG, Devous MD, Gregory RR, Herman JH, Jennings L, Bonte FJ, Nasrallah HA, Raese JD . (1990): Hypofrontality and cognitive impairment in schizophrenia: Dynamic single-photon tomography and neuropsychological assessment of schizophrenic brain function. Biol Psychiat 27: 377–399
Petty RG, Barta PE, Pearlson GD, McGilchrist IK, Lewis RW, Tien AY, Pulver A, Vaughn DD, Casanova MF, Powers RE . (1995): Reversal of asymmetry of the planum temporale in schizophrenia. Am J Psychiat 152: 715–721
Rajkowska G, Selemon LD, Goldman-Rakic PS . (1998): Neuronal and glial somal size in the prefrontal cortex. A postmortem study of schizophrenia and Huntington's disease. Arch Gen Psychiat 55: 215–224
Richfield EK, Young AB, Penney JB . (1989): Comparative distributions of dopamine D-1 and D-2 receptors in the cerebral cortex of rats, cats, and monkeys. J Compar Neurol 286: 409–426
Role LW, Kelly JP . (1991): The brain stem: Cranial nerve nuclei and the monoaminergic systems. In Kandel ER, Schwartz JH, Jessell TM (eds), Principles of Neural Science: Third Edition. New York: Elsevier, pp 683–699
Rossi A, Stratta P, Mancini F, Galluci M, Mattei P, Core L, Di Michele V, Casacchia M . (1994): Magnetic resonance imaging findings of amygdala-anterior hippocampus shrinkage in male patients with schizophrenia. Psychiat Res 52: 43–53
Sanfilipo M, Wolkin A, Angrist B, van Kammen DP, Duncan E, Wieland S, Cooper TB, Peselow ED, Rotrosen J . (1996): Amphetamine and negative symptoms of schizophrenia. Psychopharmacology 123: 211–214
Sawaguchi T, Goldman-Rakic PS . (1991): D1 dopamine receptors in prefrontal cortex: Involvement in working memory. Science 251: 947–950
Seeman P, Lee T, Chau-Wong M, Wong K . (1976): Antipsychotic drug doses and neuroleptic/dopamine receptors. Nature 261: 717–719
Seeman P, Van Tol HHM . (1994): Dopamine receptor pharmacology. TIPS 15: 264–270
Selemon LD, Goldman-Rakic PS . (1999): The reduced neuropil hypothesis: A circuit-based model of schizophrenia. Biol Psychiat 45: 17–25
Selemon LD, Goldman-Rakic PS . (1988): Common cortical and subcortical targets of the dorsolateral prefrontal and posterior parietal cortices in the rhesus monkey: Evidence for a distributed neural network subserving spatially guided behavior. J Neurosci 8: 4049–4068
Selemon LD, Rajkowska G, Goldman-Rakic PS . (1998): Elevated neuronal density in prefrontal area 46 in brains from schizophrenic patients: Application of a three-dimensional, stereologic counting method. J Comp Neurol 392: 402–412
Selemon LD, Rajkowska G, Goldman-Rakic PS . (1995): Abnormally high neuronal density in the schizophrenic cortex: A morphometric analysis of prefrontal area 9 and occipital area 17. Arch Gen Psychiat 52: 805–818
Shapiro RM . (1993): Regional neuropathology in schizophrenia: Where are we? Where are we going? Schizophr Res 10: 187–239
Shenton ME, Kikinis R, Jolesz FA, Pollak SD, LeMay M, Wible CG, Hokama H, Martin J, Metcalf D, Coleman M, McCarley RW . (1992): Abnormalities of the left temporal lobe and thought disorder in schizophrenia: A quantitative magnetic resonance imaging study. N Engl J Med 327: 604–612
Smiley JF, Levey AI, Ciliax BJ, Goldman-Rakic PS . (1994): D1 dopamine receptor immunoreactivity in human and monkey cerebral cortex: Predominant and extrasynaptic localization in dendritic spines. Proc Nat Acad Sci USA 91: 5720–5724
Suddath RL, Christison GW, Torrey EF, Casanova MF, Weinberger DR . (1990): Anatomical abnormalities in the brains of monozygotic twins discordant for schizophrenia. N Engl J Med 322: 789–794
Verin M, Partoit A, Pillon B, Malapani C, Agid Y, Dubois B . (1993): Delayed response tasks and prefrontal lesions in man—Evidence for self-generated patterns of behavior with poor environmental modulation. Neuropsychologia 31: 1279–1296
Volkow ND, Wolf AP, Van Gelder P, Brodie JD, Overall JE, Cancro R, Gomez-Mont F . (1987): Phenomenological correlates of metabolic activity in 18 patients with chronic schizophrenia. Am J Psychiat 144: 151–158
Weinberger DR . (1988): Schizophrenia and the frontal lobe. TINS 11: 367–370
Weinberger DR, Berman KF, Illowsky BP . (1988): Physiological dysfunction of dorsolateral prefrontal cortex in schizophrenia. III. A new cohort and evidence for a monoaminergic mechanism. Arch Gen Psychiat 1988;45: 609–615
Weinberger DR, Berman KF, Zec RF . (1986): Physiological dysfunction of dorsolateral prefrontal cortex in schizophrenia. I. Regional cerebral blood flow (rCBF) evidence. Arch Gen Psychiat 43: 114–125
Weinberger DR, Wagner RL, Wyatt RJ . (1983): Neuropathological studies of schizophrenia: A selective review. Schizophr Bull 9: 193–212
Wexler BE, Stevens AA, Bowers AA, Sernyak MJ, Goldman-Rakic PS . (1999): Word and tone working memory deficits in schizophrenia. Arch Gen Psychiat 55: 1093–1096
Williams GV, Goldman-Rakic PS . (1995): Modulation of memory fields by dopamine D1 receptors in prefrontal cortex. Nature 376: 572–575
Williams RW, Rakic P . (1988): Three-dimensional counting: An accurate and direct method to estimate numbers of cells in sectioned material. J Compar Neurol 278: 344–352
Wolkin A, Barouche F, Wolf AP, Rotrosen J, Fowler JS, Shiue CY, Cooper TB, Brodie JD . (1989): Dopamine blockade and clinical response: Evidence for two biological subgroups of schizophrenia. Am J Psychiat 146: 905–908
Wolkin A, Angrist B, Wolf A, Brodie JD, Wolkin B, Jaeger J, Cancro R, Rotrosen J . (1988): Low frontal glucose utilization in chronic schizophrenia: A replication study. Am J Psychiat 145: 251–253
Acknowledgements
This work was supported by NIMH 38546 and 44866 and an unrestricted educational grant from Hoechst Marion Roussel.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Goldman-Rakic, P. The Relevance of the Dopamine-D1 Receptor in the Cognitive Symptoms of Schizophrenia. Neuropsychopharmacol 21 (Suppl 2), S170–S180 (1999). https://doi.org/10.1016/S0893-133X(99)00107-4
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1016/S0893-133X(99)00107-4
Keywords
This article is cited by
-
D1 dopamine receptors intrinsic activity and functional selectivity affect working memory in prefrontal cortex
Molecular Psychiatry (2021)
-
Effects of Risperidone on Procedural Learning in Antipsychotic-Naive First-Episode Schizophrenia
Neuropsychopharmacology (2009)
-
In vivo pharmacological characterization of the structurally novel, potent, selective mGlu2/3 receptor agonist LY404039 in animal models of psychiatric disorders
Psychopharmacology (2007)
-
Clozapine, SCH 23390 and α-flupenthixol but not haloperidol attenuate acute phencyclidine-induced disruption of conditional discrimination performance
Psychopharmacology (2007)
-
Treatments for schizophrenia: a critical review of pharmacology and mechanisms of action of antipsychotic drugs
Molecular Psychiatry (2005)