Abstract
The biotransformation of venlafaxine (VF) into its two major metabolites, O-desmethylvenlafaxine (ODV) and N-desmethylvenlafaxine (NDV) was studied in vitro with human liver microsomes and with microsomes containing individual human cytochromes from cDNA-transfected human lymphoblastoid cells. VF was coincubated with selective cytochrome P450 (CYP) inhibitors and several selective serotonin reuptake inhibitors (SSRIs) to assess their inhibitory effect on VF metabolism. Formation rates for ODV incubated with human microsomes were consistent with Michaelis-Menten kinetics for a single-enzyme mediated reaction with substrate inhibition. Mean parameters determined by non-linear regression were: Vmax = 0.36 nmol/min/mg protein, Km = 41 μM, and Ks 22901 μM (Ks represents a constant which reflects the degree of substrate inhibition). Quinidine (QUI) was a potent inhibitor of ODV formation with a Ki of 0.04 μM, and paroxetine (PX) was the most potent SSRI at inhibiting ODV formation with a mean Ki value of 0.17 μM. Studies using expressed cytochromes showed that ODV was formed by CYP2C9, −2C19, and −2D6. CYP2D6 was dominant with the lowest Km, 23.2 μM, and highest intrinsic clearance (Vmax/Km ratio). No unique model was applicable to the formation of NDV for all four livers tested. Parameters determined by applying a single-enzyme model were Vmax = 2.14 nmol/min/mg protein, and Km = 2504 μM. Ketoconazole was a potent inhibitor of NDV production, although its inhibitory activity was not as great as observed with pure 3A substrates. NDV formation was also reduced by 42% by a polyclonal rabbit antibody against rat liver CYP3A1. Studies using expressed cytochromes showed that NDV was formed by CYP2C9, −2C19, and −3A4. The highest intrinsic clearance was attributable to CYP2C19 and the lowest to CYP3A4. However the high in vivo abundance of 3A isoforms will magnify the importance of this cytochrome. Fluvoxamine (FX), at a concentration of 20 μM, decreased NDV production by 46% consistent with the capacity of FX to inhibit CYP3A, 2C9, and 2C19. These results are consistent with previous studies that show CYP2D6 and −3A4 play important roles in the formation of ODV and NDV, respectively. In addition we have shown that several other CYPs have important roles in the biotransformation of VF.
Similar content being viewed by others
Main
The last several years has seen a dramatic increase in our understanding of drug metabolism and drug-drug interactions that are mediated through the inhibition or induction of cytochrome P-450 (CYP) enzymes. This is due in part to advances in techniques collectively called “reaction phenotyping,” and includes the use of cDNA-expressed enzymes, and human liver microsomal preparations in combination with chemical inhibitors and antibodies directed against specific CYPs.
One of the most frequently prescribed classes of medications is the antidepressants, many of which are either substrates of CYP2D6 or CYP3A3/4, or are inhibitors of these two CYP systems. With the large amount of data being produced, clinicians have been looking for a way to generalize information regarding the capacity of antidepressants to inhibit various CYPs.
At least seven other studies have examined the relative inhibitory potencies of the SSRIs and their metabolites in relation to 2D6 mediated reactions. These reactions include sparteine to 2-dehydrosparteine (Crewe et al. 1992), dextromethorphan to dextrorphan (Otton et al. 1993), desipramine to 2-hydroxydesipramine (von Moltke et al. 1995), imipramine to 2-hydroxyimipramine (Skjelbo and Brøsen 1992; Ball et al. 1997), clomipramine to 8-hydroxyclomipramine (Nielsen et al. 1996), desmethylclomipramine to 8-hydroxydesmethylclomipramine (Nielsen et al. 1996), and metoprolol to α-hydroxymetoprolol and O-demethylmetoprolol (Belpaire et al. 1998).
One of the newer antidepressants, venlafaxine (VF), is a structurally novel compound of the phenylethylamine class. VF inhibits the presynaptic reuptake of serotonin, norepinephrine, and to a lesser extent dopamine (Muth et al. 1986). It has little to no affinity for α-1 adrenergic, muscarinic, or histaminergic receptors, and does not inhibit monoamine oxidase (Muth et al. 1986). VF is effective as an antidepressant (Schweizer et al. 1994; Cunningham et al. 1994), and may have utility in the treatment of panic disorder (Geracioti 1995), and attention-deficit disorder (Findling et al. 1996).
VF is biotransformed in the liver to O-desmethylvenlafaxine (ODV), N-desmethylvenlafaxine (NDV), and N,O-didesmethylvenlafaxine (N,O-DV) (Muth et al. 1991). ODV has a receptor affinity profile similar to its parent compound VF, while the latter two metabolites have little if any affinity for the above receptor sites (Muth et al. 1991). Previous studies have shown that the biotransformation of VF to ODV is mediated by CYP2D6, and NDV via CYP3A3/4, and possibly a second enzyme (Otton et al. 1996).
We used an in vitro model of human liver microsomal preparations and of microsomes containing individual human cytochromes expressed by cDNA-transfected human lymphoblastoid cells, to evaluate the biotransformation of VF to its principal metabolites ODV and NDV over a large range of substrate concentrations. We also assessed the inhibitory potencies of the currently available SSRIs and their metabolites. This was done to evaluate the possibility of pharmacokinetic interactions of VF with SSRIs, and to evaluate the consistency across substrates of impaired CYP2D6 mediated metabolism caused by SSRIs.
METHODS
Chemicals
VF, ODV, and NDV were generously provided by Wyeth-Ayerst Laboratories (Philadelphia, PA). Ketoconazole (KET) was provided by Janssen Research Foundation (Beerse, Belgium). Dextrorphan D-tartrate was purchased from Research Biochemicals International (Natick, MA). Quinidine (QUI), α-naphthoflavone (ANA), and sulfinpyrazone (SFZ) were purchased from Sigma Chemical (St. Louis, MO). Sertraline (SER) and desmethylsertraline (DES) were gifts from Pfizar (Groton, CT), and fluoxetine (FLU) and norfluoxetine (NOR) were gifts from Eli Lilly (Indianapolis, IN). Paroxetine (PX) was generously provided by SmithKline Beecham (Philadelphia, PA), and fluvoxamine (FX) from Solvay (Marietta, GA). The cofactors, including NADP, (±)-isocitric acid, MgCl2, and isocitrate dehydrogenase, as well as the potassium phosphate salt used in the buffer solution were purchased from Sigma. All organic solvents were reagent grade.
Liver Samples and Preparation of Microsomes
Liver samples were obtained from the International Institute for the Advancement of Medicine (Exton, PA), or the Liver Tissue Procurement and Distribution Service, University of Minnesota (Minneapolis, MN).
Donors had no known liver disease. The tissue was partitioned and stored at −80° until microsome preparation. Microsomes were prepared as previously described by von Moltke et al. (1993; 1994), and protein concentrations of the microsome samples was determined using the Bicinchoninic Acid Protein Assay (BCA-Pierce Rockford IL). Bovine serum albumin was used as the standard.
Microsomes containing human cytochromes P4501A2, −2C9, −2C19, −2D6, −2E1, and −3A4, expressed in cDNA-transfected human lymphoblastoid cells (Crespi 1995) were obtained from Gentest (Woburn, MA).
Antibody
Serum containing polyclonal antibody against rabbit rat liver CYP3A1 and goat antibody against rat CYP2C were purchased from Human Biologics, Inc. (Phoenix, AZ).
Calibration Standards
Mixtures used to generate calibration curves contained ODV (0–10 nmoles) or NDV (0–10 nmoles) which were evaporated to dryness prior to the addition of 50 mM potassium phosphate buffer (pH adjusted to 7.5 at 25°C), and dextrorphan as internal standard.
Studies with Human Liver Microsomes
Velocity versus substrate concentration curves were generated by incubating varying concentrations of VF (0–20,000 μM) with cofactor composed of 50 mM potassium phosphate buffer (pH adjusted to 7.5 at 25°C), 0.5 mM NADP, 3.75 mM (±)-isocitric acid, 1 unit/ml isocitrate dehydrogenase, and 5 mM Mg++. Final volumes were 250 μL, with a microsomal protein concentration of 400 μg/ml. Solvents were evaporated to dryness prior to the addition of cofactors and buffer, and preincubated for 15 minutes at 37°C. The reaction was initiated by the addition of microsomes. Similarly VF (25, 50, 100, and 1000 μM), microsomal protein, and cofactor were incubated with FLU (2.5 and 10 μM), NOR (2.5 and 10 μM), SER (2.5 and 10 μM), DES (2.5 and 10 μM), FX (5 and 20 μM), and PX (1 and 2.5 μM). Identical mixtures of VF at concentrations of 50 μM and 750 μM were incubated with cofactor, microsomal protein, and QUI (0–50 μM), ANA (0–5.0 μM), KET (0–20 μM), or SFZ (0–50 μM).
Incubations lasted for 40 minutes, and were stopped by the addition of 50 μL acetonitrile and cooling on ice. Dextrorphan was added an internal standard, and the mixture was centrifuged at 5000 rev/min for 5 minutes in a Micro-MB centrifuge. Supernatants were removed and placed in the appropriate vials for HPLC analysis. All incubations were done in duplicate. The protein concentration and reaction time were predetermined to fall within the linear range. Incubations were done without cofactor to exclude the presence of non-NADP dependent metabolite formation. Products were verified by matching retention times of incubated samples to retention times of pure samples of VF, ODV, and NDV.
Studies with Microsomes Containing cDNA-Expressed Cytochromes
Initial studies indicated that ODV, NDV, or both, were formed by CYP2C9, −2C19, −2D6, and −3A4. Accordingly varying concentrations of VF (0–5000 μM) were incubated with these individual cytochromes (1 mg of protein per ml). After 40 minutes reactions were stopped, and incubates processed for HPLC analysis. Control incubations were performed with microsomes from cells transfected with expression vector alone.
Immunoinhibition Studies
Using the same incubation preparations as above, microsomes and either antibody or control serum were preincubated at 37° for 20 minutes with a fixed VF concentration (750 μM). Antibody concentrations varied from 1:5 to 1:15 microsomal:antibody mass ratios. Reactions were initiated by the addition of cofactors, and incubated for 40 minutes at 37°. Final reaction volumes were 250 μL. The mixtures were processed as above prior to HPLC analysis.
HPLC Analysis
Concentrations of ODV and NDV were determined using HPLC with UV detection. A 30 cm × 3.9 mm steel C18 μBondapack column (Waters, Milford, MA) was used for separation. A Lambda-Max Model 480 LC ultraviolet spectrophotometer (Waters) was set at a wavelength of 225 nm. The mobile phase consisted of 22% acetonitrile and 78% 50 mM potassium phosphate buffer (pH 6). The flow rate was 1.3 ml/min. The inhibitors did not interfere with substrate, product, or internal standard peaks. Substrate, metabolite, and internal standard were stable at room temperature over 36 hours.
Data Analysis
For studies with human liver microsomes, plots of reaction velocity versus substrate concentration (Figure 1 ) and reciprocal (Eadie-Hofstee) plots (not shown) for ODV were consistent with single-enzyme Michaelis-Menten kinetics with substrate inhibition. Furthermore this model was statistically superior to a single enzyme model as assessed by the F-test and Akaike's information criterion (Motulsky and Ransnas 1987; Schmider et al. 1996). Accordingly, the following equation (equation 1) was fitted to the data points using derivative-free iterative nonlinear least-squares regression (Norby et al. 1991): 
Rate of formation of ODV in relation to concentrations of the substrate venlafaxine by microsomal preparations from a representative human sample. Reaction velocities are shown without inhibitor, and with coaddition of quinidine (QUI) 0.25 or 0.5 μM. Function lines were determined by nonlinear least squares regression. Inset: Rate of formation of ODV in relation to concentrations of the substrate, venlafaxine, up to a concentration of 20,000 μM.
Iterated variables were Vmax, the maximum velocity, Km the substrate concentration at which the reaction velocity equals 50% of Vmax, and Ks, a constant reflecting the degree of substrate inhibition.
Data for reaction velocities with addition of inhibitors was initially evaluated by double reciprocal (Lineweaver-Burke) plots, which were consistent with competitive inhibition. Furthermore, because substrate inhibition constants (Ks) were large, we assumed that the addition of this variable into the determination of competitive inhibition constants would not significantly change their value.
Accordingly, data points obtained for the incubation of substrate plus inhibitor were fitted to the following equation (equation 2), consistent with Michaelis-Menten kinetics and competitive inhibition:  where I is the inhibitor concentration, and Ki is the iterated variable, the competitive inhibition constant. Vmax and Km were predetermined using the control data points without inhibitor.
where I is the inhibitor concentration, and Ki is the iterated variable, the competitive inhibition constant. Vmax and Km were predetermined using the control data points without inhibitor.
The same methods used to assess the production of NDV did not yield a single model that best fit the data for all four liver microsomal protein preparations. The data points for two of the samples used were best fit by a single-enzyme Michaelis-Menten model, while the goodness of fit was slightly improved by a 2-component model in the other 2 cases (Figure 2 ). For the purposes of comparison a single enzyme model was employed for all 4 livers. Data consisted of reaction velocities (V) at varying substrate concentrations (S) and were fitted to the equation (equation 3):  where Vmax and Km were the iterated variables.
where Vmax and Km were the iterated variables.
Rate of formation of NDV in relation to concentration of the substrate venlafaxine by microsomal preparations from a representative human sample. Function lines were determined by nonlinear least squares regression. Dotted line (---) represents non-linear least squares regression analysis using a one-enzyme model (Equation 3). Solid line (—) represents non-linear least squares regression analysis using a two-enzyme model.
Inhibitory effects of chemical inhibitors versus NDV formation were evaluated as the ratio of the velocity of NDV formation rate in the presence of inhibitor to the velocity without inhibitor at a fixed VF concentration of 1000 μM (Table 1).
The reaction velocity versus substrate concentration relationship for studies of individual human cytochromes was evaluated by graphical methods, and fit to the appropriate model. Kinetic parameters were determined by nonlinear regression as described above.
RESULTS
Incubation of VF with human liver microsomes resulted in the formation of ODV and NDV. Formation of ODV from VF had a mean Vmax of 0.36 nmol/min/mg protein, a mean Km of 40.6 μM, and a mean Ks of 22901 μM (Table 2). Using the Vmax//Km ratio as a quantity to estimate intrinsic clearance, approximately 90% of total intrinsic clearance was accounted for by the O-demethylation pathway.
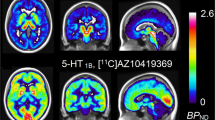
Incubations of 50 μM VF with varying concentrations of SFZ and ANA, inhibitors of CYP2C9 and CYP1A2, respectively, revealed no consistent inhibitory effect on ODV formation. There was a 40% decrease with KET at the highest concentration (25 μM), although this inhibitor is only considered specific for CYP3A4 at concentrations of 1 μM or less (Newton et al. 1995). The CYP2D6 inhibitor, QUI, caused significant inhibition at all concentrations (Figure 3 ). All six SSRIs inhibited the formation of ODV with PX being the most potent and DES being the least potent (Table 3).
Effect of varying concentrations of ketoconazole (⋄), quinidine (□), sulfinpyrazone (▴), and α-naphthoflavone (•) on the formation of O-desmethylvenlafaxine. Each point is the ratio, expressed in percent, of the reaction velocity at the indicated inhibitor concentration divided by the velocity with no inhibitor.
ODV was formed by human CYP2C9, −2C19, and −2D6. CYP2D6 was dominant, with the highest intrinsic clearance, and a low Km (23 μM) similar to the Km obtained in human liver microsomes (Table 4 and Table 2). The concentration-velocity curves for ODV formation using pure CYP2D6 and microsomal preparations both were consistent with single enzyme Michaelis-Menten kinetics with substrate inhibition (equation 1; Figure 1; Figure 4 ).
Rate of formation of O-desmethylvenlafaxine in relation to concentration of the substrate venlafaxine by microsomes containing pure human cytochromes expressed by cDNA-transfected human lymphoblastoid cells. Function lines determined by nonlinear least squares regression. Inset: venlafaxine concentrations up to 1000 μM.
Formation of NDV had a mean Vmax of 2.14 nmol/min/mg protein, and a mean Km of 2504 μM (Table 2). Incubations of 750 μM VF with SFZ and QUI led to 18% and 23% reduction in NDV production respectively, while increasing concentrations of ANA led to an 11% increase in NDV formation over baseline. KET had a more profound effect on NDV formation, leading to a 65% mean reduction in production of this metabolite (Figure 5 ).
Effect of varying concentrations of ketoconazole (⋄), quinidine □), sulfinpyrazone (▴), and α-naphthoflavone (•) on the formation of N-desmethylvenlafaxine. Each point is the ratio, expressed in percent, of the reaction velocity at the indicated inhibitor concentration divided by the velocity with no inhibitor.
A polyclonal rabbit antibody against rat liver CYP3A1, in microsomal protein/antibody ratios varying from 1:5 to 1:15 reduced the formation of NDV from 36 to 42% respectively, while there was no effect on ODV formation. There was no inhibition with rabbit control serum, goat control serum, or goat antibody against rat CYP2C, on either ODV or NDV formation.
Of the SSRIs, only FX at a concentration of 20 μM had a significant inhibitory effect on NDV production (Table 1). All other SSRIs employed were weak inhibitors of NDV formation at the concentrations used.
NDV was formed by CYP2C9, −2C19, and −3A4 (Table 4, Figure 6 ). The highest intrinsic clearance was attributable to CYP2C19. NDV formation by CYP3A4 was best described by a two-component Michaelis-Menten model, in which most of the intrinsic clearance was attributable to the high affinity component (Km = 556 μM).
Rate of formation on N-desmethylvenlafaxine in relation to concentration of the substrate venlafaxine by microsomes containing pure human cytochromes expressed by cDNA-transfected human lymphoblastoid cells. Function lines determined by nonlinear least squares regression. Inset: venlafaxine concentrations up to 1000 μM.
DISCUSSION
The biotransformation of VF to ODV and NDV was studied by using several complimentary methods of reaction phenotyping including pure human CYPs expressed by cDNA-transfected human lymphoblastoid cells, and human liver microsomal preparations in combination with CYP specific antibodies and chemical inhibitors. Our data obtained through the use of multiple experimental methods agrees with, but extends previous studies using only human liver microsomes (Otton et al. 1996). Several recent studies have used a combination of methods to achieve a better understanding of the metabolic pathways for other compounds including amitriptyline (Venkatakrishnan et al. 1998a), dextromethorphan (von Moltke et al. 1998), and citalopram (Kobayashi et al. 1997).
cDNA-expressed enzymes can determine with a high degree of certainty whether a CYP isoform is capable of catalyzing a metabolic reaction, and are often sensitive enough to detect the involvement of CYPs that make a relatively minor contribution to the overall biotransformation of a substrate. In the present study, ODV was produced by cDNA-expressed CYP2C9, CY2C19, and CYP2D6, although we were unable to identify the contribution of CYP2C9 or CYP2C19 in liver microsomes using either chemical inhibition by SFZ or anti-2C antibodies in human microsomes.
Unlike microsomal preparations that contain all of the CYPs in their native proportions, cDNA-expressed enzymes alone cannot determine whether an enzymatic pathway makes a quantitatively important contribution to the overall metabolism of a compound. The method developed by Crespi (1995) attempts to quantify the contribution of an cDNA-expressed enzyme to the overall metabolism of a substrate by multiplying the intrinsic clearance via a specific pathway by the relative abundance of the enzyme in human liver (Shimada et al. 1994; Venkatakrishnan et al. 1998b). Using the data from the pure cytochromes with normalization for relative abundance, the relative contribution of the CYP2D6 pathway to ODV formation was 89% (Table 4). This is in good agreement with the results obtained in human microsomal preparations that showed QUI reduced ODV by 89% to 100% of control levels (Figure 3).
While several CYPs may catalyze the same reaction, at the low concentrations that exist during normal therapeutic use, the isoform with the highest affinity for the substrate (lowest Km value) is more likely to have the predominant role in the biotransformation of that compound. Consequently, inhibition of that isoform is likely to have the greatest clinical effect. Because the CYP2D6 pathway makes the greatest relative contribution to the reaction, compounds that are strong CYP2D6 inhibitors should have the lowest Ki values. All six of the SSRIs tested inhibited the formation of ODV, though they were one to two orders of magnitude less potent than QUI. Previous studies have examined the inhibitory potency of SSRIs on CYP2D6 mediated reactions (Table 5). In general, PX, FLU, and NOR are strong inhibitors of CYP2D6 mediated reactions, while SER, DES, and FX are weaker.
The kinetics of NDV formation in human liver microsomes were determined using concentrations up to 20,000 μM, which is higher than the maximum (500 μM) used in previous studies (Otton et al. 1996). Although a single unique enzyme kinetic mechanism for NDV formation could not be clearly identified, a one enzyme model (equation 3) adequately fit the data and allowed us to compare kinetic parameters in a relative fashion (Table 2).
Studies using cDNA-expressed cytochromes show that CYP2C19, −2C9 and −3A4 can all catalyze the formation of NDV. Although less abundant than CYP3A in vivo, CYP2C19 had the highest affinity and highest intrinsic clearance for NDV formation (Table 4). KET, at concentrations less than 1 μM, is a potent and relatively specific inhibitor of CYP3A, inhibited the formation of NDV (750 μM) by approximately 70%. Antibodies directed against rat liver CYP3A1, known to cross-react and inhibit human CYP3A (von Moltke et al. 1995), decreased NDV formation rate by about 40%. At the high concentration used (750 μM), anti-CYP2C antibodies had no effect on NDV production. We would predict that during routine clinical use of VF, CYP2C19, CYP2C9, as well as CYP3A all would contribute importantly to the formation of NDV. At higher VF concentrations, or in individuals with reduced CYP2C19 activity secondary to genetic polymorphism or chemical inhibition, CYP3A4 increases in importance.
Of the SSRIs used, only FX at a concentration of 20 μM had a significant inhibitory effect on NDV production (Table 1). This is consistent with the activity of FX as an inhibitor of both CYP3A and 2C19, as well as CYP2C9. The other SSRIs used had little or no inhibitory effect at the concentrations tested. Studies using different CYP3A substrates including triazolam (von Moltke et al. 1996a), alprazolam (von Moltke et al. 1995), terfenadine (von Moltke et al. 1996b), amitriptyline (Schmider et al. 1995), and midazolam (Ring et al. 1995; von Moltke et al. 1996c) clearly show that the SSRIs and their metabolites can inhibit CYP3A isoforms, with FX and NOR generally evident as the most potent.
References
Ball SE, Ahern D, Scatina J, Kao J . (1997): Venlafaxine: In vitro inhibition of CYP2D6 dependent imipramine and desipramine metabolism; comparative studies with selected SSRIs, and effects on human hepatic CYP3A4, CYP2C9, and CYP1A2. Br J Clin Pharmacol 43: 619–626
Belpaire FM, Wijnant P, Temmerman A, Rasmussen BB, Brosen K . (1998): The oxidative metabolism of metoprolol in human liver microsomes: Inhibition by the selective serotonin reuptake inhibitors. Eur J Clin Pharmacol 54: 261–264
Crespi CL . (1995): Xenobiotic—metabolizing human cells as tools for pharmacological and toxicological research. Advances Drug Res 26: 179–235.
Crewe HK, Lennard MS, Tucker GT, Woods FR, Haddock RE . (1992): The effect of selective serotonin reuptake inhibitors on cytochrome P4502D6 (CYP2D6) activity in human liver microsomes. Br J Clin Pharmacol 34: 262–265
Cunningham LA, Borison RL, Carman JS, Chouinard G, Crowder JE, Diamond BI, Fischer DE, Hearst E . (1994): A comparison of venlafaxine, trazadone, and placebo in major depression. J Clin Psychopharm 14: 99–106
Findling RL, Schwartz MA, Flannery DJ, Manos MJ . (1996): Venlafaxine in adults with attention-deficit/hyperactivity disorder: an open clinical trial. J Clin Psych 57: 184–189
Geracioti TD . (1995): Venlafaxine treatment of panic disorder: A case series. J Clin Psych 56: 408–410
Kobayashi K, Chiba K, Yagi T, Shimada N, Taniguchi T, Horie T, Tani M, Yamamoto T, Ishizaki T, Kuroiwa Y . (1997): Identification of cytochrome P450 isoforms involved in citalopram N-demthylation by human liver microsome. JPET 280: 927–933
Motulsky HJ, Ransnas LA . (1987): Fitting curves to data using nonlinear regression: A practical and nonmathematical review. FASEB 1: 365–374
Muth EA, Haskins JT, Moyer JA, Husbands GEM, Nielsen ST, Sig EB . (1986): Antidepressant biochemical profile of the novel bicyclic compound Wy-45,030, an ethyl cyclohexanol derivative. Biochem Pharmacol 5: 4493–4497
Muth EA, Moyer JA, Haskins JT . (1991): Biochemical, neurophysiological, and behavioral effects of WY-45, 233 and other identified metabolites of the antidepressant venlafaxine. Drug Dev Res 23: 191–199
Newton DJ, Wang RW, Lu AYH . (1995): Cytochrome P450 inhibitors: Evaluation of specificities in the in vitro metabolism of therapeutic agents by human liver microsomes. Drug Metab Dispos 23: 154–158
Nielsen KK, Flinois JP, Beaune P, Brosen K . (1996): The biotransformation of clomipramine in vitro, identification of the cytochrome P450s responsible for the separate metabolic pathways. J Pharmacol Exp Ther 77: 1659–1664
Norby J, Rubenstein S, Tuerke T, Farmer S, Forood R, Bennington J . (1991): Sigma Plot, v. 2.00. Jandel Corporation.
Otton SV, Ball SE, Cheung SW, Inaba T, Rudolph RL, Sellers EM . (1996): Venlafaxine oxidation in vitro is catalyzed by CYP2D6. Br J Clin Pharmacol 41: 149–156
Otton SV, Wu D, Joffe RT, Cheung SW, Sellers EM . (1993): Inhibition by fluoxetine of cytochrome P450 2D6 activity. Clin Pharmacol Ther 53: 401–409
Ring BJ, Binkley SN, Roskos L, Wrighton SA . (1995): Effect of fluoxetine, norfluoxetine, sertraline, and desmethylsertraline on human CYP3A catalyzed 1′-hydroxy midazolam formation in vitro. J Pharmacol Exp Ther 275: 1131–1135
Schmider J, Greenblatt DJ, Harmatz JS, Shader RI . (1996): Enzyme kinetic modelling as a tool to analyse the behaviour of cytochrome P450 catalysed reactions: application to amitriptyline N-demethylation. Br J Clin Pharmacol 41: 593–604
Schmider J, Greenblatt DJ, von Moltke LL, Harmatz JS, Shader RI . (1995): N-demethylation of amitriptyline in vitro: Role of cytochrome P-450 3A (CYP3A) isoforms and effect of metabolic inhibitors. J Pharmacol Exp Ther 275: 592–597
Schweizer E, Feighner J, Mandos LA, Rickels K . (1994): Comparison of venlafaxine and imipramine in the acute treatment of major depression in outpatients. J Clin Psych 55: 104–108
Shimada T, Yamazaki H, Mimura M, Inui Y, Guengerich FP . (1994): Interindividual variations in human liver cytochrome P-450 enzymes involved in the oxidation of drugs, carcinogens and toxic chemicals: Studies with liver microsomes of 30 Japanese and 30 Caucasians. JPET 270: 414–423
Skjelbo E, Brøsen K . (1992): Inhibitors of imipramine metabolism by human liver microsomes. Br J Clin Pharmacol 34: 256–261
Venkatakrishnan K, Greenblatt DJ, von Moltke LL, Schmider J, Harmatz JS, Shader RI . (1998a): Five distinct human cytochromes mediate amitriptyline N-demethylation in vitro: Dominance of CYP2C19 and 3A4. J Clin Pharmacol 38: 112–121
Venkatakrishnan K, von Moltke LL, Greenblatt DJ . (1998b): Relative quantities of catalytically active CYP2C9 and 2C19 in human liver microsomes: application of the relative activity factor approach. J Pharm Sci 87: 845–853
von Moltke LL, Greenblatt DJ, Cotreau-Bibbo MM, Duan SX, Harmatz JS, Shader RI . (1994): Inhibition of desipramine hydroxylation in vitro by serotonin-reuptake-inhibitor antidepressants, and by quinidine and ketoconazole: A model system to predict drug interactions in vivo. J Pharmacol Exp Ther 268: 1278–1283
von Moltke LL, Greenblatt DJ, Court MH, Duan SX, Harmatz JS, Shader RI . (1995): Inhibition of alprazolam and desipramine hydroxylation in vitro by paroxetine and fluvoxamine: Comparison with other selective serotonin reuptake inhibitor antidepressants. J Clin Psychopharm 15: 125–131
von Moltke LL, Greenblatt DJ, Grassi JM, Granda BW, Venkatakrishnan K, Schmider J, Harmatz JS, Shader RI . (1998): Multiple human cytochromes contribute to biotransformation of dextromethorphan in vitro: Role of CYP2C9, CYP2C19, CYP2D6, and CYP3A. J Pharm Pharmacol 50: 997–1004
von Moltke LL, Greenblatt DJ, Harmatz JS, Shader RI . (1993): Alprazolam metabolism in vitro: Studies of human, monkey, mouse, and rat liver microsomes. Pharmacology 47: 268–276
von Moltke LL, Greenblatt DJ, Harmatz JS, Duan SX, Harrel LM, Cotreau-Bibbo MM, Pritchard GA, Wright CE, Shader RI . (1996a): Triazolam biotransformation by human liver microsomes in vitro. Effects of metabolic inhibitors and clinical confirmation of a predicted interaction with ketoconazole. J Pharmacol Exp Ther 276: 370–379
von Moltke LL, Greenblatt DJ, Duan SX, Harmatz JS, Wright CE, Shader RI . (1996b): Inhibition of terfenadine metabolism in vitro by azole antifungals agents and by selective serotonin reuptake inhibitor antidepressants: Relation to pharmacokinetic interactions in vivo. J Clin Psychopharmacol 16: 104–112
von Moltke LL, Greenblatt DJ, Schmider J, Duan SX, Wright CE, Harmatz JS, Shader RI . (1996c): Midazolam hydroxylation by human liver microsomes in vitro: Inhibition by fluoxetine, norfluoxetine, and by azole antifungal agents. J Clin Pharmacol 36: 783–791
Acknowledgements
This work was supported by Grants MH-34223, MH-19924, and RR-00054 from the USPHS. Dr. Fogelman is the recipient of an American College of Neuropsychopharmacology Glaxo-Wellcome Fellowship in Clinical Neuropsychopharmacology. Dr. Schmider was the recipient of a Merck International Fellowship in Clinical Pharmacology. Dr. von Moltke is the recipient of a Scientist Development Award (K21-MH-01237) from the National Institutes of Mental Health.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Fogelman, S., Schmider, J., Venkatakrishnan, K. et al. O- and N-demethylation of Venlafaxine In Vitro by Human Liver Microsomes and by Microsomes from cDNA-Transfected Cells: Effect of Metabolic Inhibitors and SSRI Antidepressants. Neuropsychopharmacol 20, 480–490 (1999). https://doi.org/10.1016/S0893-133X(98)00113-4
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1016/S0893-133X(98)00113-4
Keywords
This article is cited by
-
Physiologically Based Pharmacokinetic Modeling to Unravel the Drug-gene Interactions of Venlafaxine: Based on Activity Score-dependent Metabolism by CYP2D6 and CYP2C19 Polymorphisms
Pharmaceutical Research (2024)
-
Pharmacokinetic correlates of venlafaxine: associated adverse reactions
European Archives of Psychiatry and Clinical Neuroscience (2019)
-
Functional and structural characterisation of common cytochrome P450 2D6 allelic variants—roles of Pro34 and Thr107 in catalysis and inhibition
Naunyn-Schmiedeberg's Archives of Pharmacology (2019)
-
Pharmacokinetics of venlafaxine in treatment responders and non-responders: a retrospective analysis of a large naturalistic database
European Journal of Clinical Pharmacology (2019)
-
WhichP450: a multi-class categorical model to predict the major metabolising CYP450 isoform for a compound
Journal of Computer-Aided Molecular Design (2018)