Abstract
Introduction
Direct oral anticoagulants (DOACs) were developed to overcome some of the limitations associated with vitamin K antagonists (VKAs), such as interindividual variability or the need for therapeutic drug monitoring. However, the complexity of DOAC dose regimens can still lead to dosing errors and potential bleeding-related or thromboembolic adverse events, especially in the elderly.
Objective
Our objective was to evaluate the rate of inappropriate preadmission DOAC prescriptions at hospital and to evaluate the ability of hospitals to correct them.
Methods
An observational prospective study was conducted in elderly patients (aged ≥ 65 years) hospitalized in six acute units of three Parisian university hospitals between February and July 2018. DOAC prescriptions prior to admission and at discharge were analyzed according to the guidelines in the summaries of product characteristics.
Results
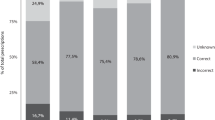
A total of 157 patients were included in the study, with a median age of 84 years (interquartile range [IQR] 77–89). The median glomerular filtration rate, determined with the Cockcroft–Gault equation, was 48 mL/min (IQR 35–61). Apixaban was the most frequently prescribed drug, mainly for atrial fibrillation. Overall, 48 (30.6%) and 34 (22.4%) prescriptions were inappropriate prior to admission and at discharge, respectively, showing a significant decrease (p < 0.001). Hospitals significantly corrected more inappropriate prescriptions (37.5%) than they generated (4.6%) (p < 0.05). The nature of the inappropriate prescribing was underdosing (68.8% and 76.5% prior to admission and at discharge, respectively), followed by overdosing (stable rate at almost 20%) and indication errors. No risk factors for inappropriate use were identified by our analysis.
Conclusion
One-third of DOAC preadmission prescriptions for elderly patients were inappropriate, indicating that a need remains to strengthen DOAC prescribing guidelines in ambulatory clinical practice. However, the rate of inappropriate prescriptions decreased at patient discharge. Future studies are needed to test actions to promote the proper use of DOACs.

Similar content being viewed by others
References
Pradaxa® (dabigatran). Summary of Product Characteristics. Boehringer Ingelheim.
Xarelto® (rivaroxaban). Summary of Product Characteristics. Bayer Healthcare.
Eliquis® (apixaban). Summary of Product Characteristics. Bristol-Myers Squibb.
Connoly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus Warfarin in Patients with Atrial Fibrillation. N Engl J Med. 2009;361(12):1139–51.
Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365(10):883–91.
Granger CB, Alexander JH, McMurray JJ, et al. Apixaban versus Warfarin in Patients with Atrial Fibrillation. N Engl J Med. 2011;365(11):981–92.
Rapport d’évaluation des médicaments anticoagulants oraux. HAS, commission de la transparence. 2018.
Etude de l’Assurance Maladie sur l’utilisation des nouveaux anticoagulants oraux. Assurance Maladie. 2013.
Kirchhof P, Benussi S, Kotecha D, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur J Cardiothorac Surg. 2016;50(5):e1–88.
Ruff CT, Giugliano RP, Braunwald E, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014;383(9921):955–62. https://doi.org/10.1016/S0140-6736(13)62343-0 (Epub 2013 Dec 4).
Shrestha S, Baser O, Kwong WJ. Effect of renal function on dosing of non-vitamin K antagonist direct oral anticoagulants among patients with nonvalvular atrial fibrillation. Ann Pharmacother. 2018;52(2):147–53.
Bourcier E, Mille F, Brunie V, et al. Quality of prescribing in community-dwelling elderly patients in France: an observational study in community pharmacies. Int J Clin Pharm. 2017;39(6):1220–7. https://doi.org/10.1007/s11096-017-0531-6 (Epub 2017 Sep 14).
Sorensen R, Gislason G, Torp-Pedersen C, et al. Dabigatran use in Danish atrial fibrillation patients in 2011: a nationwide study. BMJ Open. 2013;3(5):e002758. https://doi.org/10.1136/bmjopen-2013-002758.
Howard M, Lipshutz A, Roess B, et al. Identification of risk factors for inappropriate and suboptimal initiation of direct oral anticoagulants. J Thromb Thrombolysis. 2017;43(2):149–56.
Pattullo CS, Barras M, Tai B, et al. New oral anticoagulants: appropriateness of prescribing in real-world setting. Intern Med J. 2016;46(7):812–8.
Lafon T, Vallejo C, Hadj M, et al. Misuse and adverse effects of new direct oral anticoagulants: A prospective observational study in patients admitted to an emergency unit of a French university hospital. Therapie. 2018;73(3):209–15.
Piau A, Huet Y, Gallini A, et al. Optimization of drug therapy in elderly individuals admitted to a geriatric unit. Clin Interv Aging. 2017;12:1691–6.
Lee JK, Slack MK, Martin J, et al. Geriatric patient care by U.S. pharmacists in healthcare teams: systematic review and meta-analyses. J Am Geriatr Soc. 2013;61(7):1119–27.
Moudallel S, Steurbaut S, Cornu P, et al. Appropriateness of DOAC prescribing before and during hospital admission and analysis of determinants for inappropriate prescribing. Front Pharmacol. 2018;9:1220. https://doi.org/10.3389/fphar.2018.01220 (eCollection 2018).
Franchi C, Antoniazzi S, Proietti M, et al. Appropriateness of oral anticoagulant therapy prescription and its associated factors in hospitalized older people with atrial fibrillation. Br J Clin Pharmacol. 2018;84(9):2010–9. https://doi.org/10.1111/bcp.13631 (Epub 2018 Jun 19).
Yao X, Shah ND, Sangaralingham LR, et al. Non-vitamin K antagonist oral anticoagulant dosing in patients with atrial fibrillation and renal dysfunction. J Am Coll Cardiol. 2017;69(23):2779–90.
Froissart M, Rossert J, Jacquot C, et al. Predictive performance of the modification of diet in renal disease and Cockcroft-Gault equations for estimating renal function. J Am Soc Nephrol. 2005;16(3):763–73.
Pérez Cabeza AI, Chinchurreta Capote PA, Gonzalez Correa JA, et al. Discrepancies between the use of MDRD-4 IDMS and CKD-EPI equations, instead of the Cockcroft-Gault equation, in the determination of the dosage of direct oral anticoagulants in patients with non-valvular atrial fibrillation. Med Clin (Barc). 2018;150(3):85–91.
Mantha S, Ansell J. An indirect comparison of dabigatran, rivaroxaban and apixaban for atrial fibrillation. Thromb Haemost. 2012;108(3):476–84.
Acknowledgements
The authors gratefully acknowledge the pharmacists from the six centers for their participation in this study. The kind assistance of Stella Ghouti, qualified translator is also gratefully acknowledged.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of funding were used to conduct this study or prepare this manuscript.
Conflict of interest
A. Bruneau, C. Schwab, M. Anfosso, C. Fernandez and P. Hindlet have no potential conflicts of interest that might be relevant to the contents of this manuscript.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bruneau, A., Schwab, C., Anfosso, M. et al. Burden of Inappropriate Prescription of Direct Oral Anticoagulants at Hospital Admission and Discharge in the Elderly: A Prospective Observational Multicenter Study. Drugs Aging 36, 1047–1055 (2019). https://doi.org/10.1007/s40266-019-00710-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-019-00710-8