Abstract
The prevalence of hypertension and comorbidities such as metabolic syndrome, diabetes mellitus, and chronic kidney disease in India is alarmingly high. Amlodipine, an older-generation calcium channel blocker (CCB), is currently the gold standard for hypertension management in India. However, it has several disadvantages, including reflex tachycardia and pedal edema. Therefore, an effective antihypertensive agent that does not cause these adverse effects and provides end-organ protection is required for the holistic management of hypertension in the country. Azelnidipine is a new-generation CCB that has recently been approved for the treatment of hypertension in India. This review provides an overview of the utility of azelnidipine for hypertension control, including comparisons with traditional CCBs such as amlodipine. It discusses the key antihypertensive effects of azelnidipine as well as its advantages in the prevention of tachycardia and associated complications. In addition, this review highlights the extensive cardio- and renoprotective activities of azelnidipine, including its effects on systolic and diastolic function and urinary albumin excretion. Overall, this substantial body of evidence supports the use of azelnidipine for the treatment of hypertension, especially in India. It suggests that the adoption of azelnidipine as the new gold standard CCB could help India battle its hypertension epidemic.
Similar content being viewed by others
The multiple disadvantages of amlodipine, the gold standard calcium channel blocker (CCB) for hypertension, can be overcome using the newer-generation CCB azelnidipine. |
Azelnidipine can lower blood pressure without causing reflex tachycardia and has additional cardioprotective effects. |
Azelnidipine can also offer renal protection and prevent diabetic nephropathy. |
Azelnidipine appears to be an effective and well-tolerated agent for holistic hypertension management. |
Azelnidipine could be especially useful for tackling the hypertension epidemic in India, where the aging population has a high prevalence of comorbidities. |
Introduction
Hypertension is a disorder characterized by elevated blood pressure (BP) levels. According to guidelines from the European Society of Cardiology and European Society of Hypertension, hypertension is defined as a systolic BP (SBP) level of at least 140 mmHg and/or a diastolic BP (DBP) level of at least 90 mmHg [1]. Hypertension is often referred to as a “silent killer” because it typically presents without warning signs or symptoms. Moreover, many patients with hypertension are unaware that they have this condition [2].
In India, the rates of both hypertension and cardiovascular diseases caused by uncontrolled hypertension are growing rapidly [3]. A national survey showed that almost one in every three Indian adults had hypertension in 2019 [4]. Hypertension is the most important risk factor for cardiovascular disease in India [5]. However, the rates of hypertension awareness and treatment control in the country are low [6]. Moreover, individuals in India often show significant seasonal variation in BP, along with a combination of multiple cardiovascular risk factors [3]. Hence, the effective control of hypertension is necessary to reduce large-scale premature morbidity and mortality in India. The Indian guidelines for BP control recommend targets of 130/80 mmHg in individuals aged less than 60 years and 130–140/80–90 mmHg in those aged more than 60 years [3]. In addition to lifestyle changes, these guidelines also recommend calcium channel blockers (CCBs) as first-line treatment agents for patients with hypertension, especially those aged 60 years or more [3].
CCBs, also called calcium channel antagonists, have been widely used to treat hypertension for several decades [7]. This group of agents is often divided into two classes: non-dihydropyridines (e.g., verapamil and diltiazem) and dihydropyridines (e.g., nifedipine and amlodipine) (Fig. 1). CCBs exert their effects by binding to and inhibiting voltage-gated calcium channels in the heart and vascular smooth muscles [8]. There are several subtypes of calcium channels. Therefore, CCBs are classified on the basis of the type of calcium channel they predominantly inhibit, viz., L-type (e.g., amlodipine), L/T-type (e.g., cilnidipine), and L/N-type (e.g., benidipine) CCBs (Fig. 1) [9].
In clinical practice, earlier-generation CCBs such as amlodipine are associated with adverse events, including reflex tachycardia and pedal edema [10]. Therefore, newer CCBs that do not produce these unwanted effects have been developed. One such agent is azelnidipine, which has emerged as a novel and effective CCB for antihypertensive management. First developed in Japan [11], azelnidipine was approved for the treatment of hypertension by the Drug Controller General of India in 2020. Since its approval, azelnidipine has shown great promise in becoming a valuable tool in the country’s battle against hypertension. Therefore, to encourage the adoption of azelnidipine as the new gold standard CCB in India, this review summarizes its unique properties and its value in hypertension control. It also highlights the benefits of azelnidipine compared with other commonly used CCBs, such as amlodipine, especially from an Indian perspective. This review is based on previously conducted studies and does not contain any new studies with human participants or animals.
Characteristics and Pharmacodynamics of Azelnidipine
Azelnidipine (C33H34N4O6; molecular weight = 582.657), a novel, third-generation CCB, is a 1,4-dihydropyridine derivative [12]. Previously called CS-905, azelnidipine was jointly developed in Japan by Ube Industries, Ltd. (Yamaguchi, Japan) and Daiichi Sankyo Co, Ltd (Tokyo, Japan). Since then, it has undergone extensive clinical trials and was approved for the treatment of hypertension in Japan and China, before recently receiving approval as an antihypertensive agent in India. Clinically, azelnidipine is administered orally at a dose of 8–16 mg. Although higher doses up to 32 mg have been tested in volunteers, they are not recommended owing to concerns regarding clinical usefulness and safety. In patients with hypertension, azelnidipine 16 mg/day is rapidly absorbed after oral administration, with a time to peak drug concentration of 4.14 ± 1.46 h and a peak drug concentration of 48.3 ng/mL [13]. Other pharmacokinetic values during 6 weeks of treatment include an apparent total body clearance of 42,200 ± 15,400 mL/h, an area under the concentration–time curve from 0 to 24 h of 426 ± 151 ng·h/mL, and a half-life of 8.68 ± 1.33 h [13].
Azelnidipine exerts its action by inhibiting transmembrane Ca2+ influx through voltage-dependent channels in the cell membranes of smooth muscles [14]. Older-generation CCBs such as amlodipine and nifedipine predominantly target L-type calcium channels, which are located in the vascular smooth muscle cells of peripheral arteries [9]. However, azelnidipine also blocks T-type calcium channels, which are present in both afferent and efferent arterioles (Fig. 2) [9, 15]. Therefore, unlike older CCBs, which reduce heart contractility and increase pulse rate and glomerular pressure, azelnidipine decreases blood pressure (Fig. 3a), heart rate (HR) (Fig. 3b), and glomerular pressure [9, 16, 17]. Furthermore, because of the role of T-type channels in the zona glomerulosa of the adrenal glands, azelnidipine can also reduce the secretion of aldosterone [15, 18, 19], providing additional BP control. Azelnidipine is also more lipid-soluble than older CCBs like amlodipine and has a higher selectivity for the vascular wall [20]. Therefore, azelnidipine is retained in the vascular wall even after its clearance from the rest of the body and continues to elicit BP-lowering effects [21]. As detailed below, azelnidipine also has a number of other benefits that complement its antihypertensive action.
Azelnidipine: A Preclinical and Clinical Perspective
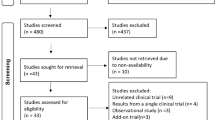
A number of preclinical (Table 1) and clinical studies (Table 2) have been conducted to determine the activity, efficacy, safety, and tolerability of azelnidipine.
BP-Lowering Effects and Safety
Oizumi et al. reported that a single dose of azelnidipine could dose-dependently reduce mean arterial pressure in conscious spontaneously hypertensive rats (SHR) [11]. This decrease in BP was gradual, peaking at 6 h post-administration, and was maintained up to 20 h post-treatment [11]. Additional experiments by the same group in conscious hypertensive dogs revealed similar findings [22]. Subsequently, the regular administration of azelnidipine over a 15-week period was shown to be associated with a sustained reduction in SBP in SHR, without the induction of tolerance. It was also found to be associated with increased blood flow to the kidneys, brain, and spleen [23]. The BP-lowering activity of azelnidipine was further confirmed in patients with essential hypertension, where treatment with azelnidipine 16 mg/day for 6 weeks significantly reduced BP over the 24-h dosing period, both during the day and night [13]. Since then, both short- and long-term studies and systematic reviews have confirmed the therapeutic efficacy of azelnidipine for reducing BP [13, 24–29]. Data from clinical trials have also established the safety of azelnidipine, demonstrating that it is usually well tolerated and is only associated with limited adverse effects such as mild headaches, light-headedness, and flushing [13, 24,25,26,27,28,29,30] (Table 2).
End-Organ Effects
In addition to detailed clinical studies on the hypertension-related therapeutic effects of azelnidipine, the effects of this CCB on other end organs have also been investigated. Azelnidipine has been found to have beneficial effects in the ischemic myocardium in dogs. A study showed that pre-treatment with azelnidipine improves myocardial contractile dysfunction in dogs during post-ischemia reperfusion [31]. Preclinical studies have also documented the renoprotective effects of azelnidipine in SHR, revealing increases in urine flow and sodium excretion post-treatment, without alterations in the glomerular filtration rate (GFR) and renal plasma flow (Fig. 4) [32]. The long-term administration of azelnidipine has also been reported to reduce arterial and glomerular injury in the kidneys of SHR [33]. In addition, orally administered azelnidipine (8–16 mg/day) has been shown to increase renal plasma and blood flow compared with baseline in patients with hypertension and normal renal function [34], indicating its potential renoprotective effects.
Given that the antihypertensive effects of CCBs can alter hemodynamics, the effects of azelnidipine on cerebral circulation have also been investigated. A study by Kimura et al. confirmed the maintenance of cerebral blood flow and cerebral vascular reserve after azelnidipine administration. It also revealed BP-lowering effects in patients with both hypertension and ischemic white matter lesions [35].
Other beneficial effects of azelnidipine have also been reported. Treatment with azelnidipine 8–16 mg/day for 12 weeks was associated with mild anti-atherosclerotic effects in patients with mild-to-moderate hypertension. This was thought to be due to its antioxidative action [36]. In a multicenter, prospective, randomized open-label study that enrolled patients with hypertension who were scheduled for coronary intervention, treatment with azelnidipine significantly reduced plaque volume 48 weeks after treatment initiation [37].
In addition, in vitro and in vivo experiments have suggested that azelnidipine has anti-inflammatory activity that is independent of its hemodynamic effects [38]. More recent preclinical studies (Table 1) have also reported the antioxidant benefits of azelnidipine. One study using human hepatic stellate (LX-2) cells and mouse models of fibrosis showed that azelnidipine inhibits liver fibrosis and increases antioxidant activity in these models [39]. Another study reported that azelnidipine can preserve insulin signaling and glucose uptake under conditions of oxidative stress in adipocytes [40]. These data highlight the potential benefits of azelnidipine beyond reductions in BP.
Advantages of Azelnidipine: Comparison with Amlodipine and Other CCBs
Amlodipine is currently considered the gold standard CCB for the management of hypertension. However, a growing body of evidence now supports the advantages of azelnidipine over amlodipine and other CCBs, both from the perspective of hemodynamic control and “beyond BP” effects on other end organs, such as the kidneys.
Cardiovascular Benefits
Data from recent studies suggest that azelnidipine might improve BP and HR to a greater extent than amlodipine (Table 3) [13, 40,41,42,43].
In a randomized double-blind clinical trial enrolling 220 patients with essential hypertension, Zhao et al. reported that azelnidipine reduced both SBP and DBP to a greater extent than amlodipine [44]. Another randomized double-blind study compared the effects of azelnidipine and amlodipine on 24-h BP in patients with essential hypertension [13]. Although both drugs had similar antihypertensive effects, the HR increased by 4 beats/min in amlodipine recipients but decreased by 2 beats/min in the azelnidipine group [13]. Consistent with these findings, Yamagishi reported a significant HR reduction after azelnidipine treatment in patients with a baseline HR > 70 beats/min [43]. A recent meta-analysis evaluating the clinical efficacy of azelnidipine in Chinese patients reported similar findings [21]. Preclinical data have shown that azelnidipine has a greater intrinsic negative chronotropic action than amlodipine and is associated with less baroreceptor reflex activation. This is most likely due to its slower onset of hypertensive effects [45]. Together, the evidence supports the dual action of azelnidipine for BP and HR control, which could contribute to its overall cardiovascular benefits.
The cardioprotective effects of azelnidipine have also been demonstrated in studies which show that it can prevent left ventricular (LV) remodeling and improve systolic and diastolic function [46,47,48]. A study of 32 patients with hypertension showed that treatment with azelnidipine or amlodipine reduced LV mass, improved transmitral flow and tissue Doppler findings, and significantly improved LV longitudinal strain compared with baseline [46]. Takami and Saito evaluated the effects of olmesartan (an angiotensin II receptor blocker) in combination with either azelnidipine or amlodipine on central BP and LV mass index (LVMI) in patients with hypertension [47]. Although the two regimens had similar effects on brachial BP, treatment with olmesartan/azelnidipine was associated with greater reductions in central BP and LVMI compared with olmesartan/amlodipine [47]. In another study of 92 Chinese patients with mild-to-moderate essential hypertension, LV diastolic function improved from baseline in both the azelnidipine and amlodipine groups [48]. However, plasma levels of brain natriuretic peptide (BNP), an indicator of cardiac function, were significantly lower in the azelnidipine group, indicating the net benefits of azelnidipine [48].
Owing to the link between autonomic activity and cardiovascular function [49], and especially the development and progression of heart failure (HF) [50], the autonomic effects of azelnidipine have attracted attention from researchers. In a small prospective, randomized, open-label, crossover study, Inomata et al. compared the effects of azelnidipine and amlodipine on muscle sympathetic nerve activity in 14 patients with hypertension. They performed microneurography of the peroneal nerve, a well-established method of sympathetic activity measurement in humans. They found that azelnidipine had more favorable effects on sympathetic nerve activity in patients with hypertension than did amlodipine, without any effects on baroreflex sensitivity [16]. The authors of this study suggested that azelnidipine might therefore be a better treatment option in patients with hypertension complicated by HF or ischemic heart disease [16]. Koike et al. used pupillometry to compare the effects of amlodipine and azelnidipine on changes in autonomic activity in patients with essential hypertension [51]. Patients were treated with azelnidipine or amlodipine and underwent assessments for BP, pulse rate, and pupillary function before and after an isometric handgrip exercise. The findings showed that azelnidipine was more effective in inhibiting autonomic activation and suppressing cardiovascular responses to an isometric handgrip exercise. Additionally, it was suggested that this sympathoinhibitory effect could be beneficial in patients with essential hypertension [51]. Consistent with these findings, Nada et al. found that patients with hypertension showed significant reductions in HR, the total number of extrasystoles, noradrenaline levels, the LF/HF ratio (an indicator of sympathovagal balance), and the washout rate on 123I-MIBG myocardial scintigraphy (an indicator of cardiac risk) after switching from amlodipine to azelnidipine [52]. In patients with HF with preserved ejection fraction, azelnidipine attenuated cardiac sympathetic nerve activity dysfunction to a significantly greater extent than cilnidipine [53]. Moreover, another study reported that the beneficial effects of azelnidipine on autonomic function in patients with hypertension were greater than those of benidipine [54]. Data from these studies highlight the broader cardiovascular benefits of azelnidipine, suggesting that it may be appropriate as the first-choice CCB in patients with hypertension, especially those with cardiac dysfunction or HF.
Diabetes-Related Benefits
Azelnidipine has the potential to be a useful treatment option in patients with hypertension and other comorbidities, such as diabetes. For example, azelnidipine has been shown to promote the healing of skin wounds in rat models of diabetes [55]. The specific antihypertensive benefits of azelnidipine have also been evaluated in patients with diabetes. For example, a multicenter, open-label trial investigated the efficacy and safety of azelnidipine in Japanese patients with type 2 diabetes and hypertension [56]. Treatment with azelnidipine for 48 weeks effectively reduced BP in this group of patients, although slight increases in glycosylated hemoglobin levels were observed [56]. Significant reductions in BP during treatment with azelnidipine (combined with the angiotensin-converting enzyme inhibitor temocapril) were also reported in another multicenter, randomized, open-label, ascending-dose study [57].
Patients with both hypertension and diabetes are at a substantially increased risk of cardiovascular disorders compared to patients with either condition alone [58]. This underscores the importance of preventing diabetes in patients with hypertension. Azelnidipine has been shown to have some potential in this regard. Fukao et al. compared the effects of azelnidipine and amlodipine on glucose and insulin levels at 120 min after a 75-g oral glucose tolerance test in patients with hypertension [41]. Reductions in both glucose and insulin levels were significantly greater in the azelnidipine group than in the amlodipine group. This suggested that azelnidipine might have glucose-lowering beneficial effects in non-diabetic patients with hypertension [41].
Renal Protection
Hypertension is both a cause and consequence of chronic kidney disease (CKD) [59]. Several effects of azelnidipine are likely to be beneficial in terms of renal protection, as described below.
Hyperuricemia has been linked to arterial hypertension. Serum uric acid levels are an independent risk factor for both the development of hypertension [60] and a non-dipper circadian pattern of hypertension [61]. Miyazaki et al. examined the effects of azelnidipine on uric acid metabolism in 72 patients with hypertension. After 2–3 months of treatment, reductions in both serum urate levels and the urinary uric acid to creatinine ratio were observed [62]. These findings indicate that azelnidipine may ameliorate uric acid-related conditions such as gout, in addition to hypertension.
Fujimoto et al. examined the effects of azelnidipine on peritubular capillary blood flow and tubulointerstitial injury induced by angiotensin II (AII) in rats [63]. They found that azelnidipine attenuated AII-induced decreases in peritubular capillary blood flow, and reduced tubulointerstitial injuries and hypoxia in the kidneys of AII-treated rats [63]. The effects of azelnidipine were stronger than those of nifedipine, another CCB [63].
Other modes of azelnidipine-induced renoprotection have also been explored. In the Jikei Azelnidipine Study (JAz-HDM), patients with hypertension and type 2 diabetes mellitus were enrolled. The treatment agent was switched from other CCBs to azelnidipine (16 mg/day), and patients underwent laboratory examinations before and 6 months after the switch [19]. Although switching to azelnidipine did not alter BP control, it decreased plasma aldosterone concentrations, without any change in plasma renin activity [19]. Given that aldosterone has been implicated in the induction of renal injury through multiple pathways (e.g., inflammation and glomerular hypertension) [64], these findings suggest that the blockade of aldosterone synthesis or aldosterone release by azelnidipine could provide some protection against CKD.
Protection Against Diabetic Nephropathy
Some of the renoprotective activities of azelnidipine relate to its effects on diabetic nephropathy, which is characterized by increased urinary albumin excretion (i.e., proteinuria). Diabetic nephropathy is a leading cause of end-stage CKD [65, 66] and also contributes to renal senescence [67].
Nakamura et al. performed a randomized clinical trial (RCT) that enrolled 30 patients with moderate hypertension and CKD. The patients were treated with azelnidipine 16 mg once daily or amlodipine 5 mg once daily over a 6-month period [68]. Endpoints included urinary protein excretion, and urinary levels of 8-hydroxy-2′-deoxyguanosine (8-OHdG, a biomarker of oxidative stress and damage) and liver-type fatty acid binding protein (L-FABP, an indicator of CKD prognosis) [68]. Patients treated with azelnidipine, but not those treated with amlodipine, showed decreases in urinary protein excretion, 8-OHdG levels, and L-FABP levels after 3 and 6 months of treatment [68]. The authors concluded that azelnidipine exerted renoprotective effects in patients with hypertension and mild CKD, in part owing to its antioxidant effects [68].
Subsequent studies confirmed these findings. An RCT compared the effects of azelnidipine and amlodipine on urinary albumin excretion and levels of 8-OHdG and L-FABP in patients with hypertension, diabetes, and CKD who were already under treatment with maximal dosages of olmesartan (Fig. 5) [69]. After 24 weeks of treatment, the urinary albumin-to-creatinine ratio and 8-OHdG and L-FABP levels were significantly lower in the azelnidipine group than in the amlodipine group [69]. In addition, the BOAT2 study showed that azelnidipine, but not amlodipine, reduced urinary albumin excretion, the maximum carotid intima-media thickness, and levels of inflammatory cytokines in patients with well-controlled type 2 diabetes [70].
Comparative effects of azelnidipine and amlodipine on a urinary albumin and b C-reactive protein levels (data from Abe et al. [69]). AML amlodipine, AZE azelnidipine, Cr creatinine, CRP C-reactive protein
Azelnidipine has also been compared with nifedipine with respect to its effects on urinary albumin excretion in patients with hypertension, type 2 diabetes, and nephropathy under treatment with renin–angiotensin system inhibitors [71]. After 16 weeks of treatment, azelnidipine significantly reduced serum levels of inflammatory markers and C-reactive protein, urinary levels of 8-OHdG, and the urinary albumin-to-creatinine ratio. However, no such improvements were seen during treatment with nifedipine [71].
Comparison with Fourth-Generation CCBs
Fourth-generation CCBs, such as cilnidipine (an L/N-type CCB) and lercanidipine, have now become available. They are highly lipophilic and offer advantages such as stable activity and fewer side effects. Unfortunately, most studies on these drugs compare their effectiveness and safety with that of amlodipine, because it is considered the gold standard CCB [72]. Therefore, few studies have compared azelnidipine with these drugs, especially lercanidipine. In a pilot study, cilnidipine and azelnidipine provided comparable BP- and HR-lowering effects, although cilnidipine produced a greater reduction in the urinary albumin-to-creatinine ratio [73]. However, a retrospective study comparing cilnidipine with older-generation CCBs found no difference between the effects of azelnidipine and cilnidipine on the estimated GFR and serum creatinine levels after 12 months of drug initiation [74]. Another study demonstrated that in patients with HF with preserved ejection fraction, switching from cilnidipine to azelnidipine tended to decrease the levels of BNP and could reduce dysfunctions in cardiac sympathetic nerve activity [53]. Therefore, the current data appear to be insufficient. Further studies are required to understand how azelnidipine compares to fourth-generation CCBs such as cilnidipine and lercanidipine in terms of its holistic effects on BP, cardiovascular health, metabolic syndrome, and renal function.
Advantages of Azelnidipine in an Indian Context
As mentioned previously, the prevalence of hypertension in India is high in both middle-aged and older individuals across regions and sociodemographic groups [4]. In addition, the prevalence among younger individuals is higher than previously estimated [4]. This is especially concerning because hypertension can significantly influence patient quality of life [75]. More importantly, hypertension is a major risk factor for cardiovascular disorders, metabolic syndrome, diabetes, and CKD [2], all of which are also highly prevalent in the Indian population [76, 77]. Therefore, patients and clinicians across the country would benefit from an agent that provides antihypertensive effects in individuals both with and without additional comorbidities, and protects against the development of cardiovascular, metabolic, and renal disorders. Currently available data suggest that azelnidipine is suited to fulfil this role.
Like many other countries around the world, India is experiencing population aging, with the number of older individuals expected to almost double by 2050 [78]. This will contribute to an increase in the burden of non-communicable diseases such as hypertension, and hypertension-related comorbidities such as cardiovascular, metabolic, and kidney disease. As described above, azelnidipine has a variety of beneficial effects in addition to BP-lowering effects. Therefore, although amlodipine is currently the CCB of choice for many clinicians in India, azelnidipine appears to be an appropriate, effective, and well-tolerated alternative for the holistic management of hypertension.
Conclusion
Azelnidipine has been approved for use as an antihypertensive agent in India. As noted in this review, azelnidipine has several advantages over the current CCB of choice in India (amlodipine) and other agents in this class. These include benefits beyond hypertension control, allowing holistic management of hypertension and related disorders such as cardiovascular disease, metabolic syndrome, and CKD. The evidence summarized here provides a good rationale for the adoption of azelnidipine as a first-line antihypertensive in India. Such a shift towards the use of azelnidipine in India could substantially help in the country’s fight against the hypertension epidemic and improve patient quality of life in the long term.
References
Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36:1953–2041.
World Health Organization. Hypertension Fact Sheet. https://www.who.int/news-room/fact-sheets/detail/hypertension. Accessed 17 May 2022.
Shah SN, Munjal YP, Kamath SA, et al. Indian guidelines on hypertension-IV (2019). J Hum Hypertens. 2020;34:745–58.
Ramakrishnan S, Zachariah G, Gupta K, et al. Prevalence of hypertension among Indian adults: results from the great India blood pressure survey. Indian Heart J. 2019;71:309–13.
Gupta R, Xavier D. Hypertension: the most important non communicable disease risk factor in India. Indian Heart J. 2018;70:565–72.
Anchala R, Kannuri NK, Pant H, et al. Hypertension in India: a systematic review and meta-analysis of prevalence, awareness, and control of hypertension. J Hypertens. 2014;32:1170–7.
Tocci G, Battistoni A, Passerini J, et al. Calcium channel blockers and hypertension. J Cardiovasc Pharmacol Ther. 2015;20:121–30.
McKeever RG, Hamilton RJ. Calcium channel blockers. Treasure Island (FL): StatPearls; 2022 Jan. https://www.ncbi.nlm.nih.gov/books/NBK482473/. Accessed 13 May 2022.
Abe M, Soma M. Multifunctional L/N- and L/T-type calcium channel blockers for kidney protection. Hypertens Res. 2015;38:804–6.
Elliott WJ, Ram CV. Calcium channel blockers. J Clin Hypertens (Greenwich). 2011;13:687–9.
Oizumi K, Nishino H, Koike H, Sada T, Miyamoto M, Kimura T. Antihypertensive effects of CS-905, a novel dihydropyridine Ca++ channel blocker. Jpn J Pharmacol. 1989;51:57–64.
DrugBank. Azelnidipine. https://go.drugbank.com/drugs/DB09230. Accessed 8 Feb 2022.
Kuramoto K, Ichikawa S, Hirai A, Kanada S, Nakachi T, Ogihara T. Azelnidipine and amlodipine: a comparison of their pharmacokinetics and effects on ambulatory blood pressure. Hypertens Res. 2003;26:201–8.
Sada T, Saito H. [Pharmacological profiles and clinical effects of azelnidipine, a long-acting calcium channel blocker]. Nihon Yakurigaku Zasshi. 2003;122:539–47.
Hayashi K. L-/T-type Ca channel blockers for kidney protection: ready for sophisticated use of Ca channel blockers. Hypertens Res. 2011;34:910–2.
Inomata J, Murai H, Kaneko S, et al. Differential effects of azelnidipine and amlodipine on sympathetic nerve activity in patients with primary hypertension. J Hypertens. 2014;32:1898–904.
Wellington K, Scott LJ. Azelnidipine. Drugs. 2003;63:2613–21.
Isaka T, Ikeda K, Takada Y, Inada Y, Tojo K, Tajima N. Azelnidipine inhibits aldosterone synthesis and secretion in human adrenocortical cell line NCI-H295R. Eur J Pharmacol. 2009;605:49–52.
Isaka T, Yahashi T, Sakamoto M, Sakamoto N, Ikeda K, Tojo K. Azelnidipine decreased plasma aldosterone and plasminogen activator inhibitor type 1 levels in the hypertensive patients with type 2 diabetes mellitus-the Jikei Azelnidipine study in the patients with Hypertension and Diabetes Mellitus (JAz-HDM). Ther Res. 2011;32:371–81.
Watanabe M, Hirano T, Okamoto S, Shiraishi S, Tomiguchi S, Uchino M. Azelnidipine, a long-acting calcium channel blocker, could control hypertension without decreasing cerebral blood flow in post-ischemic stroke patients. A 123I-IMP SPECT follow-up study. Hypertens Res. 2010;33:43–8.
Chen BL, Zhang YZ, Luo JQ, Zhang W. Clinical use of azelnidipine in the treatment of hypertension in Chinese patients. Ther Clin Risk Manag. 2015;11:309–18.
Oizumi K, Miyamoto M, Koike H. Antihypertensive effect of CS-905, a novel dihydropyridine calcium blocker, in conscious hypertensive dogs. Jpn J Pharmacol. 1990;53:264–6.
Oizumi K, Nishino H, Miyake S, et al. Hemodynamic changes following long-term administration of CS-905, a novel dihydropyridine calcium blocker, in conscious SHR. Jpn J Pharmacol. 1990;54:1–6.
Hirai A, Terano T, Saito Y. Efficacy and safety of CS-905 (azelnidipine) combination therapy on essential hypertension. Rinsho Iyaku. 1999;15:1505–45.
Yoshinaga K, Iimura O, Abe K, Ishii T, Saruta Y, Ogiwara T. Efficacy and safety of CS-905 (azelnidipine) in patients with essential hypertension: early phase II clinical study (pre-pilot and pilot I). Rinsho Iyaku. 1999;15:869–90.
Yoshinaga K, Iimura O, Abe K, Ishii T, Saruta Y, Ogiwara T. Efficacy and safety of CS-905 (azelnidipine) in patients with essential hypertension: early phase II clinical study (pilot II). Rinsho Iyaku. 1999;15:891–905.
Yoshinaga K, Iimura O, Abe K, Ishii T, Saruta Y, Ogiwara T. Late phase II study of CS-905, azelnidipine, in patients with essential hypertension: a multi-center, double-blind comparative study for evaluation of optimal dose. Rinsho Iyaku. 1999;15:907–42.
Yoshinaga K, Iimura O, Abe K, Ishii T, Saruta Y, Ogiwara T. Efficacy and safety of CS-905 (azelnidipine) monotherapy on essential hypertension in the long-term treatment. Rinsho Iyaku. 1999;15:943–83.
Yoshinaga K, Iimura O, Abe K, et al. Phase III clinical trial of CS-905 (azelnidipine) in patients with essential hypertension. Rinsho Iyaku. 2000;16:671–739.
Yoshinaga K, Hirai A, Yamakado M. Evaluation of safety profile of CS-905, azelnidipine, in clinical trials of hypertension. Rinsho Iyaku. 2000;16:741–62.
Satoh K, Yamamoto A, Hoshi K, Ichihara K. Effects of azelnidipine, a dihydropyridine calcium antagonist, on myocardial stunning in dogs. Jpn J Pharmacol. 1998;76:369–76.
Yagil Y, Miyamoto M, Frasier L, Oizumi K, Koike H. Effects of CS-905, a novel dihydropyridine calcium channel blocker, on arterial pressure, renal excretory function, and inner medullary blood flow in the rat. Am J Hypertens. 1994;7:637–46.
Oizumi K, Nishino H, Miyamoto M, Fukushige J, Fukami M, Koike H. Beneficial renal effects of CS-905, a novel dihydropyridine calcium blocker, in SHR. Jpn J Pharmacol. 1989;51:501–8.
Tomita K, Nonoguchi H, Marumo F. Effect of CS-905 (azelnidipine) on renal function in essential hypertension. Rinsho Iyaku. 1999;15:451–63.
Kimura Y, Kitagawa K, Oku N, et al. Hemodynamic influences of azelnidipine, a novel calcium channel blocker, on cerebral circulation in hypertensive patients with ischemic white matter lesions. Hypertens Res. 2008;31:2147–54.
Yamakado M. Clinical study of CS-905 (azelnidipine) on anti-atherosclerotics and protective effect of renal function in patients with hypertension. Rinsho Iyaku. 2000;16:355–73.
Kojima T, Miyauchi K, Yokoyama T, et al. Azelnidipine and amlodipine anti-coronary atherosclerosis trial in hypertensive patients undergoing coronary intervention by serial volumetric intravascular ultrasound analysis in Juntendo University (ALPS-J). Circ J. 2011;75:1071–9.
Komoda H, Inoue T, Node K. Anti-inflammatory properties of azelnidipine, a dihydropyridine-based calcium channel blocker. Clin Exp Hypertens. 2010;32:121–8.
Ohyama T, Sato K, Kishimoto K, et al. Azelnidipine is a calcium blocker that attenuates liver fibrosis and may increase antioxidant defence. Br J Pharmacol. 2012;165:1173–87.
Tatsumi F, Kaneto H, Hashiramoto M, et al. Anti-hypertensive azelnidipine preserves insulin signaling and glucose uptake against oxidative stress in 3T3-L1 adipocytes. Endocr J. 2015;62:741–7.
Fukao K, Shimada K, Hiki M, et al. Effects of calcium channel blockers on glucose tolerance, inflammatory state, and circulating progenitor cells in non-diabetic patients with essential hypertension: a comparative study between azelnidipine and amlodipine on glucose tolerance and endothelial function–a crossover trial (AGENT). Cardiovasc Diabetol. 2011;10:79.
Li D, Dong W, Chen Y. Azelnidipine in treatment of mild-moderate essential hypertension: a clinical trial. Jie Fang Jun Yi Xue Yuan Xue Bao. 2013;34:977–80.
Yamagishi T. Efficacy of azelnidipine on home blood pressure and pulse rate in patients with essential hypertension: comparison with amlodipine. Hypertens Res. 2006;29:767–73.
Zhao X, Wu F, Jia S, et al. Azelnidipine and amlodipine: a comparison of their effects and safety in a randomized double-blinded clinical trial in Chinese essential hypertensive patients. Clin Exp Hypertens. 2010;32:372–6.
Fujisawa M, Yorikane R, Chiba S, Koike H. Chronotropic effects of azelnidipine, a slow- and long-acting dihydropyridine-type calcium channel blocker, in anesthetized dogs: a comparison with amlodipine. J Cardiovasc Pharmacol. 2009;53:325–32.
Motoki H, Koyama J, Izawa A, et al. Impact of azelnidipine and amlodipine on left ventricular mass and longitudinal function in hypertensive patients with left ventricular hypertrophy. Echocardiography. 2014;31:1230–8.
Takami T, Saito Y. Effects of Azelnidipine plus OlmesaRTAn versus amlodipine plus olmesartan on central blood pressure and left ventricular mass index: the AORTA study. Vasc Health Risk Manag. 2011;7:383–90.
Yi S, Wu Z, Shao N, Wang Y, Feng W. The influence of azelnidipine on left ventricular diastolic function in hypertensive patients. Xian Dai Zhong Xi Yi Jie He Za Zhi. 2013;22:2797–8.
Johnson CD, Roe S, Tansey EA. Investigating autonomic control of the cardiovascular system: a battery of simple tests. Adv Physiol Educ. 2013;37:401–4.
Florea VG, Cohn JN. The autonomic nervous system and heart failure. Circ Res. 2014;114:1815–26.
Koike Y, Kawabe T, Nishihara K, Iwane N, Hano T. Effects of azelnidipine and amlodipine on exercise-induced sympathoexcitation assessed by pupillometry in hypertensive patients. Hypertens Res. 2016;39:863–7.
Nada T, Nomura M, Koshiba K, Kawano T, Mikawa J, Ito S. Clinical study with azelnidipine in patients with essential hypertension. Antiarteriosclerotic and cardiac hypertrophy-inhibitory effects and influence on autonomic nervous activity. Arzneimittelforschung. 2007;57:698–704.
Kiuchi S, Hisatake S, Kabuki T, et al. Effect of switching from cilnidipine to azelnidipine on cardiac sympathetic nerve function in patients with heart failure preserved ejection fraction. Int Heart J. 2018;59:120–5.
Yamada J, Tomiyama H, Matsumoto C, Yoshida M, Shiina K, Yamashina A. Effects of azelnidipine on the autonomic functions and its influence on arterial stiffness and endothelial functions. J Cardiol. 2008;51:114–20.
Bagheri M, Jahromi BM, Mirkhani H, et al. Azelnidipine, a new calcium channel blocker, promotes skin wound healing in diabetic rats. J Surg Res. 2011;169:e101–7.
Takihata M, Nakamura A, Kondo Y, Kawasaki S, Kimura M, Terauchi Y. Comparison of azelnidipine and trichlormethiazide in Japanese type 2 diabetic patients with hypertension: the COAT randomized controlled trial. PLoS ONE. 2015;10: e0125519.
Katayama S, Kawamori R, Iwamoto Y, Saito I, Kuramoto K. In half of hypertensive diabetics, co-administration of a calcium channel blocker and an angiotensin-converting enzyme inhibitor achieved a target blood pressure of < 130/80 mmHg: the azelnidipine and temocapril in hypertensive patients with type 2 diabetes (ATTEST) study. Hypertens Res. 2008;31:1499–508.
Sowers JR, Epstein M, Frohlich ED. Diabetes, hypertension, and cardiovascular disease: an update. Hypertension. 2001;37:1053–9.
Pugh D, Gallacher PJ, Dhaun N. Management of hypertension in chronic kidney disease. Drugs. 2019;79:365–79.
Masuo K, Kawaguchi H, Mikami H, Ogihara T, Tuck ML. Serum uric acid and plasma norepinephrine concentrations predict subsequent weight gain and blood pressure elevation. Hypertension. 2003;42:474–80.
Turak O, Ozcan F, Tok D, et al. Serum uric acid, inflammation, and nondipping circadian pattern in essential hypertension. J Clin Hypertens (Greenwich). 2013;15:7–13.
Miyazaki S, Hamada T, Hirata S, et al. Effects of azelnidipine on uric acid metabolism in patients with essential hypertension. Clin Exp Hypertens. 2014;36:447–53.
Fujimoto S, Satoh M, Nagasu H, Horike H, Sasaki T, Kashihara N. Azelnidipine exerts renoprotective effects by improvement of renal microcirculation in angiotensin II infusion rats. Nephrol Dial Transplant. 2009;24:3651–8.
Freel EM, Connell JM. Mechanisms of hypertension: the expanding role of aldosterone. J Am Soc Nephrol. 2004;15:1993–2001.
Webster AC, Nagler EV, Morton RL, Masson P. Chronic kidney disease. Lancet. 2017;389:1238–52.
Saran R, Robinson B, Abbott KC, et al. US renal data system 2016 annual data report: epidemiology of kidney disease in the United States. Am J Kidney Dis. 2017;69:A7–8.
Verzola D, Gandolfo MT, Gaetani G, et al. Accelerated senescence in the kidneys of patients with type 2 diabetic nephropathy. Am J Physiol Renal Physiol. 2008;295:F1563–73.
Nakamura T, Sugaya T, Kawagoe Y, et al. Azelnidipine reduces urinary protein excretion and urinary liver-type fatty acid binding protein in patients with hypertensive chronic kidney disease. Am J Med Sci. 2007;333:321–6.
Abe M, Maruyama N, Okada K, Matsumoto S, Matsumoto K, Soma M. Additive antioxidative effects of azelnidipine on angiotensin receptor blocker olmesartan treatment for type 2 diabetic patients with albuminuria. Hypertens Res. 2011;34:935–41.
Tawaramoto K, Kaneto H, Hashiramoto M, et al. Azelnidipine, but not amlodipine, reduces urinary albumin excretion and carotid atherosclerosis in subjects with type 2 diabetes: blood pressure control with olmesartan and azelnidipine in type 2 diabetes (BOAT2 study). Diabetol Metab Syndr. 2015;7:80.
Ogawa S, Mori T, Nako K, Ito S. Combination therapy with renin-angiotensin system inhibitors and the calcium channel blocker azelnidipine decreases plasma inflammatory markers and urinary oxidative stress markers in patients with diabetic nephropathy. Hypertens Res. 2008;31:1147–55.
Wang AL, Iadecola C, Wang G. New generations of dihydropyridines for treatment of hypertension. J Geriatr Cardiol. 2017;14(1):67–72.
Abe H, Mita T, Yamamoto R, Komiya K, et al. Comparison of effects of cilnidipine and azelnidipine on blood pressure, heart rate and albuminuria in type 2 diabetics with hypertension: a pilot study. J Diabetes Investig. 2013;4(2):202–5.
Nishida Y, Takahashi Y, Tezuka K, et al. Comparative effect of calcium channel blockers on glomerular function in hypertensive patients with diabetes mellitus. Drugs R D. 2017;17(3):403–12.
Trevisol DJ, Moreira LB, Kerkhoff A, Fuchs SC, Fuchs FD. Health-related quality of life and hypertension: a systematic review and meta-analysis of observational studies. J Hypertens. 2011;29:179–88.
Prabhakaran D, Jeemon P, Roy A. Cardiovascular diseases in India: current epidemiology and future directions. Circulation. 2016;133:1605–20.
Sreeniwas Kumar A, Sinha N. Cardiovascular disease in India: a 360 degree overview. Med J Armed Forces India. 2020;76:1–3.
HelpAge global network. Ageing population in India. https://ageingasia.org/ageing-population-india/. Accessed 18 May 2022.
Kario K, Sato Y, Shirayama M, et al. Inhibitory effects of azelnidipine tablets on morning hypertension. Drugs R D. 2013;13:63–73.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article. The Rapid Service Fee was funded by the author.
Medical Writing, Editorial, and Other Assistance
Writing and editorial assistance in the preparation of this article was provided by Ms. Zeba Khatri, ELS, and funded by the author.
Author Contributions
C Venkata S Ram had the idea for the article; performed the literature search; and drafted, reviewed, and edited the article.
Disclosures
Dr. Ram is the Editor-in-Chief of Hypertension Journal, published by Incessant Publications, Gurgaon, India, which receives advertisements from IPCA Laboratories.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by the author.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Ram, C.V.S. Therapeutic Usefulness of a Novel Calcium Channel Blocker Azelnidipine in the Treatment of Hypertension: A Narrative Review. Cardiol Ther 11, 473–489 (2022). https://doi.org/10.1007/s40119-022-00276-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40119-022-00276-4