Abstract
Introduction
Following approval of dabigatran and other antithrombotics in Japan, few studies have specifically evaluated the clinical characteristics of patients prescribed these antithrombotics for nonvalvular atrial fibrillation (NVAF) in real-world practice.
Methods
We conducted a descriptive analysis of data from two real-world studies [J-dabigatran surveillance and Japanese study on current Anticoagulation therapies for Patients with nonvalvular Atrial Fibrillation (JAPAF); conducted at sites common to both studies] to determine the characteristics of patients with NVAF initiated on dabigatran etexilate [110 mg twice daily (BID; DE110) or 150 mg BID (DE150)], warfarin, rivaroxaban, or antiplatelets as their first antithrombotic treatment. Inferential statistical analyses were not performed, and no statistical hypothesis was tested.
Results
Data for 1270 and 3011 eligible patients from the J-dabigatran surveillance (DE110, 976; DE150, 273) and JAPAF study (warfarin, 82.5%; rivaroxaban, 10.3%; antiplatelets, 21%), respectively, were extracted. In the J-dabigatran surveillance, 31.8% (full cohort, 28.1%) of patients had been switched from warfarin to dabigatran. Among patients prescribed DE110/DE150, 41.4%/57.5% and 41.5%/18.7% of patients had low-to-intermediate risk for ischemic stroke (CHADS2 score of 0 or 1) and high risk for bleeding (HAS-BLED score ≥ 3), respectively. Similarly, 33.7%/41.3%/40.2% and 48.7%/42.6%/75.7% of patients taking warfarin/rivaroxaban/antiplatelets had a CHADS2 score of 0 or 1 and HAS-BLED score ≥ 3, respectively. Dabigatran was favored in patients with creatinine clearance > 50 ml/min.
Conclusions
In Japan, physicians who attempt stroke prevention in patients with atrial fibrillation choose appropriate anticoagulant treatment, taking into consideration the individual patient backgrounds as well as the features of each antithrombotic agent.
Trial Registration
ClinicalTrials.gov Identifier, NCT01491178 and University Hospital Medical Information Network (UMIN) Clinical Trial Registry Identifier, UMIN000009644.
Funding
Nippon Boehringer Ingelheim Co., Ltd.
Plain Language Summary
Plain language summary available for this article.
Similar content being viewed by others
Plain Language Summary
Several drugs became available to prevent blood clotting and blocking of the blood supply to part of the brain (stroke) in patients having an abnormal heart rhythm (nonvalvular atrial fibrillation or NVAF). However, it is still unclear what types of patients are taking what types of drugs in daily clinical care. The authors looked into data from patients who participated in two studies conducted in Japan [1270 patients from the J-dabigatran surveillance and 3011 patients from the Japanese study on current Anticoagulation therapies for Patients with nonvalvular Atrial Fibrillation (JAPAF)] to find out the relation between the types of patients with NVAF and the drugs for blood clotting prevention they were taking (dabigatran 110 mg twice daily, dabigatran 150 mg twice daily, rivaroxaban, warfarin, or antiplatelet drugs). Around 30% of the patients had changed their drug from warfarin to dabigatran. Among patients who took dabigatran 110 mg twice daily, dabigatran 150 mg twice daily, warfarin, rivaroxaban, and antiplatelet drugs, 41.4, 57.5, 33.7, 41.3, and 40.2% had low-to-intermediate risk for stroke, respectively, and 41.5, 18.7, 48.7, 42.6, and 75.7% had high risk for bleeding, respectively. Dabigatran was favored in patients having normal to mildly reduced renal function. From this research, the authors concluded that physicians in Japan choose appropriate treatment to prevent blood clotting in patients with NVAF.
Introduction
Atrial fibrillation (AF) is the most common arrhythmia in clinical practice [1], and it is estimated that the number of patients with AF in Japan will steadily increase to 1.03 million by 2050 [2]. Risk factors for thromboembolic and bleeding events in patients with nonvalvular AF (NVAF) and AF differ among Japanese, Western, and non-Asian populations. For example, female sex is not a risk factor for thromboembolic events, whereas male sex is a risk factor for major bleeding and all-cause mortality among Japanese patients with NVAF [3]. In addition, Japanese patients with AF have a higher risk of stroke and systemic embolism, increased prevalence of previous stroke, more bleeding events while taking warfarin (lower time spent in the therapeutic range), different target anticoagulation levels with warfarin [prothrombin time-international normalized ratio (PT-INR) 1.6–2.6 in patients aged ≥ 70 years], and lower body mass index (BMI) compared with non-Asians [4]. Furthermore, fewer Japanese patients with AF have hypertension or congestive heart failure, but more have diabetes mellitus, compared with non-Asians [4].
Non-vitamin K–dependent direct oral anticoagulants (DOACs; dabigatran, rivaroxaban, apixaban, and edoxaban) are recommended for the prevention of stroke and systemic embolism in patients with NVAF [5], where they are at least as effective and safe as warfarin [6,7,8,9]. In general, DOACs have a specific and improved risk profile compared with warfarin [10,11,12] and may be prescribed at suboptimal doses, depending on the bleeding risk [13].
Dabigatran was approved for reduction of the risk of stroke and systemic embolism in patients with NVAF by the United States Food and Drug Administration in 2010 [14] and by the Ministry of Health, Labour and Welfare of Japan in 2011 [15]. According to the Japanese Circulation Society (JCS), dabigatran is recommended for patients with NVAF with CHADS2 scores ≥ 1 [5].
Following approval of dabigatran in Japan, a postmarketing surveillance (PMS) study (J-dabigatran surveillance) was initiated in December 2011 to investigate the safety and effectiveness of long-term use of dabigatran in real-world settings [16]. The Japanese study on current Anticoagulation therapies for Patients with nonvalvular Atrial Fibrillation (JAPAF) [17] was also conducted in parallel to evaluate the relationship between patient characteristics and antithrombotic therapy prescribed for the prevention of ischemic stroke and systemic embolism in Japanese patients with NVAF in daily clinical practice. Because the intention was to compare results with the J-dabigatran surveillance study, the JAPAF study did not include patients who were prescribed dabigatran.
DOACs other than dabigatran (rivaroxaban, apixaban, and edoxaban) are also approved for use in Japan; however, considering the specific differences in risk factors for thromboembolic and bleeding events in Japanese patients [3], the clinical characteristics of patients prescribed dabigatran and other antithrombotic agents remain unclear. The aim of the present study was to analyze the characteristics of Japanese patients with NVAF started on dabigatran and other antithrombotics as their initial treatment by using data from the J-dabigatran surveillance and JAPAF study.
Methods
Study Designs and Patients
Details of the study designs and patient inclusion criteria for the J-dabigatran surveillance and JAPAF study have been reported previously [16, 17]. For this descriptive analysis, data pertaining to patient demographics and clinical characteristics were extracted for patients with NVAF who took dabigatran etexilate [110 mg twice daily (BID; DE110) or 150 mg BID (DE150)], warfarin, rivaroxaban (10–15 mg once daily), or antiplatelets as their first antithrombotic treatment. Only patients enrolled at sites common to both studies were included in this analysis. This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
J-dabigatran Surveillance
J-dabigatran surveillance was a prospective PMS study conducted at 1042 sites in Japan (ClinicalTrials.gov Identifier: NCT01491178). Adults with NVAF who took dabigatran for the first time between December 12, 2011, and November 30, 2013, were enrolled. Data were extracted from electric case report forms. Patients who used warfarin within 7 days prior to starting dabigatran were defined as “switchers,” and those who did not use warfarin within the evaluation period were defined as “newly initiated” [16]. A total of 6772 patients were registered, of which 6443 comprised the analysis population. Patients who were ineligible for registration or who did not visit the site after the first visit were excluded.
JAPAF Study
JAPAF study was a cross-sectional study with surveillance performed between October 2011 and March 2014 [University Hospital Medical Information Network (UMIN) Clinical Trial Registry: UMIN000009644]. Patients were enrolled between April 2012 and December 2013 at 268 sites that participated in J-dabigatran surveillance. Adults with NVAF who received antithrombotic treatment other than dabigatran were enrolled. Patients with artificial valve replacement or valvular disease were excluded. Patient data were extracted from medical records at the first visit after registration. Of 3138 patients registered at 274 sites, 3053 were eligible; 85 were considered ineligible [17]. A full list of the investigators and study sites is available from a previously published article [17].
Statistical Analysis
Patient demographics and baseline clinical characteristics [e.g., comorbidities, creatinine clearance (CrCl), risk of ischemic stroke (CHADS2 score and CHA2DS2-VASc score), risk of bleeding (HAS-BLED score), and concomitant medication] were descriptively analyzed for the two studies and for individual initial antithrombotics (DE110, DE150, warfarin, rivaroxaban, and antiplatelets). PT-INR control in patients aged < 70 and ≥ 70 years was also evaluated at treatment initiation (index date) in warfarin “switchers” and those who continued on warfarin. Inferential statistical analyses were not performed, and no statistical hypothesis was tested.
Results
Descriptive Analysis of Patient Demographics and Baseline Clinical Characteristics Between J-dabigatran Surveillance and JAPAF Study
Data for 1270 and 3011 eligible patients from the J-dabigatran surveillance and JAPAF study, respectively, were extracted for analysis (Table 1); mean [± standard deviation (SD)] age (71.1 ± 9.3 vs. 74.1 ± 9.4 years, respectively) and proportion of men (66.2 vs. 66.1%, respectively) were comparable between the studies. However, numerically fewer patients in the J-dabigatran surveillance than in the JAPAF study were aged ≥ 75 years, and more patients in the J-dabigatran surveillance had paroxysmal AF and CrCl > 50 ml/min (Table 1). In contrast, more patients in the JAPAF study than in the J-dabigatran surveillance had permanent AF, CrCl < 30 ml/min, or were at high risk for ischemic stroke (CHADS2 score ≥ 2; CHA2DS2-VASc score ≥ 2) or bleeding (HAS-BLED score ≥ 3) (Table 1).
Descriptive Analysis of Patient Demographics and Baseline Clinical Characteristics Based on Initial Antithrombotic/Anticoagulant Treatment
Among patients in the J-dabigatran surveillance, the mean age was 73.1 and 63.4 years and the proportion of men was 62.2 and 81.7% in the DE110 and DE150 groups, respectively (Table 2). CrCl was between 30 and 50 ml/min in 20.4 and 1.6% of patients taking DE110 and DE150, respectively. CrCl was < 30 ml/min in 9.7, 2.3, and 10.5% of patients taking warfarin, rivaroxaban, and antiplatelets, respectively (Table 2). The majority of the patients in the J-dabigatran surveillance were newly initiated (DE110, 67.5%; DE150, 65.2%), and the proportions of newly initiated patients in the JAPAF study were 35.1, 9.0, and 7.2% for rivaroxaban, antiplatelets, and warfarin, respectively. Overall, a similar number of dabigatran-treated patients were switched from warfarin in the J-dabigatran surveillance at baseline. However, in the JAPAF study, only 4.2% of all patients were switchers, and the majority of patients prescribed warfarin and antiplatelets continued on the same treatment (prevalent use). Most of the switchers were prescribed rivaroxaban.
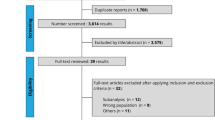
Among patients at low-to-intermediate risk for ischemic stroke (CHADS2 score of 0 or 1), 41.4 and 57.5% were prescribed DE110 and DE150, respectively, in the J-dabigatran surveillance, and the lowest proportion took warfarin among other oral anticoagulants in the JAPAF study. Among patients at high risk for ischemic stroke (CHADS2/CHA2DS2-VASc score ≥ 2), 58.6%/87.5% were prescribed DE110 and 42.5%/63.4% were prescribed DE150 in the J-dabigatran surveillance, and warfarin was taken more often than antiplatelets or rivaroxaban in the JAPAF study. Finally, among patients at high risk for bleeding (HAS-BLED score ≥ 3), most took antiplatelets, followed by warfarin and rivaroxaban in the JAPAF study, while 41.5 and 18.7% took DE110 and DE150, respectively, in the J-dabigatran surveillance (Table 2 and Fig. 1).
PT-INR Control in Warfarin-treated Patients
Only 16.4% of patients aged < 70 years who switched from warfarin to dabigatran in the J-dabigatran surveillance had optimal PT-INR control (between 2 and 3) on the index date. In contrast, approximately half of the patients aged < 70 years who continued on warfarin in the JAPAF study had optimal PT-INR control. More patients aged ≥ 70 years had optimal PT-INR control (between 1.6 and 2.6) on the index date in both studies (switchers in the J-dabigatran surveillance, 49.2%; initiated and continued warfarin in the JAPAF study, 77.3%). Suboptimal PT-INR control (< 2.0) was observed on the index date in more than three-quarters and half of patients aged < 70 years in the J-dabigatran surveillance and JAPAF study, respectively. In contrast, substantially more patients aged ≥ 70 years in the J-dabigatran surveillance than in the JAPAF study had suboptimal PT-INR control (< 1.6) on the index date (Table 3).
Discussion
Dabigatran became available in Japan in March 2011 [15], and this large descriptive analysis represents the first evaluation of the real-world characteristics of Japanese patients with NVAF treated with dabigatran (DE110 or DE150) [18] or other antithrombotic medications after approval of dabigatran. In the JAPAF study, the majority of patients were continued on warfarin treatment, and the study included a higher percentage of patients aged ≥ 75 years. With respect to type of AF, most patients prescribed dabigatran had paroxysmal AF, followed by permanent AF and vice versa for anticoagulant prescriptions in the JAPAF study. In the J-dabigatran surveillance, physicians chose dabigatran for patients with higher average CrCl in contrast to the JAPAF study where patients with CrCl ≤ 50 ml/min were more common. As anticipated, newly initiated cases were more common than switched cases in the J-dabigatran surveillance. In the JAPAF study, physicians chose to continue patients on their long-term warfarin prescriptions, suggesting good PT-INR control and lack of perceived need to switch.
It appears that physicians are prescribing according to the Japanese label that recommends an oral dose of dabigatran 150 mg BID in adults. However, for patients with moderate renal impairment (CrCl 30–50 ml/min) and those taking an oral P-glycoprotein inhibitor, a lower dose of 110 mg BID is recommended. The Japanese label also recommends administering the 110 mg BID dose with care in patients aged ≥ 70 years or in those with a history of gastrointestinal hemorrhage [15]. Similarly, the recommended dose of rivaroxaban in patients with NVAF is 15 mg/day for adults with CrCl > 50 ml/min and 10 mg/day for CrCl 30–49 ml/min per the Japanese label. Caution should be exercised with the 10 mg/day dose in patients with CrCl 15–29 ml/min [19]. This analysis suggests that in patients with reduced renal function (CrCl < 50 ml/min), DE110 was more commonly prescribed than DE150 among patients in the J-dabigatran surveillance, and warfarin and antiplatelets were more commonly prescribed than rivaroxaban in the JAPAF study. DOACs were more often prescribed to those with CrCl ≥ 50 ml/min. Furthermore, a higher dose of dabigatran was administered, particularly in patients with CrCl ≥ 50 ml/min.
The JCS recommends DOACs such as dabigatran or warfarin for patients with NVAF at high risk for ischemic stroke (CHADS2 score ≥ 2) [5]. These antithrombotic agents may also be considered in patients with other risk factors [e.g., cardiomyopathy, age 65–74 years, and vascular disease (prior myocardial infarction, aortic plaque, and peripheral vascular disease)]. Further, dabigatran and apixaban are recommended, and rivaroxaban, edoxaban, and warfarin may be considered, in patients at intermediate risk for ischemic stroke (CHADS2 score of 1). The JCS also states that the CHADS2 score can be used to accurately identify patients who are at high risk for ischemic stroke; however, this clinical prediction measure is less accurate for low-risk patients [5]. Patients at low-to-intermediate risk (CHADS2 score of 0 or 1) account for approximately half of patients with NVAF, but the efficacy of warfarin in these patients has not been established [20]. Contrary to these recommendations, 9.7–12.3% of patients at low risk (CHADS2 score of 0) were prescribed warfarin in both studies, indicating physicians’ discretion or a cautious preventive measure in these patients. DOACs were marginally favored over warfarin and antiplatelets in patients at intermediate risk (CHADS2 score of 1) for ischemic stroke. This suggests a transition towards the use of newer anticoagulants compared to warfarin and antiplatelets in low-risk patients. However, considering the years that were evaluated for data collection, warfarin was more commonly prescribed for patients with a higher risk of ischemic stroke, and also for patients who were elderly and had more comorbidities.
Overall, these results should be evaluated considering the rate of knowledge dissemination and physicians’ concerns during the transition period when the newer anticoagulants were introduced.
The JCS also recommends a PT-INR of 1.6–2.6 with warfarin in patients with NVAF aged ≥ 70 years [5]. For those aged < 70 years, a PT-INR between 2 and 3 should be maintained. Among patients aged < 70 years, only 16.4% of patients who switched from warfarin to dabigatran in the J-dabigatran surveillance had optimal PT-INR control (between 2.0 and 3.0) on the index date. However, half of the warfarin users aged < 70 years in the JAPAF study had optimal PT-INR control. In addition, optimal PT-INR control (between 1.6 and 2.6) with warfarin was observed in considerably fewer patients aged ≥ 70 years in the J-dabigatran surveillance than in the JAPAF study. These results suggest that warfarin did not produce optimal PT-INR in these age groups, necessitating a switch to another antithrombotic drug. The results also suggest that most patients with suboptimal PT-INR control may have been switched to dabigatran, although the J-dabigatran surveillance had constraints of only including switched patients from warfarin. These results are also important for other Asia–Pacific countries because, although international guidelines recommend that the optimal PT-INR of warfarin is 2.0–3.0, the practice in Asia–Pacific countries (excluding Australia and New Zealand) follows the JCS guidelines; therefore, the Asia Pacific Heart Rhythm Society 2013 statement also recommends an PT-INR of 1.6–2.6 for patients aged ≥ 70 years [21].
Finally, the JCS asserts that in patients aged > 75 years taking anticoagulants, low body weight (≤ 50 kg), CrCl ≤ 50 ml/min, and use of antiplatelets are major risk factors for bleeding [5]. Antiplatelets are expected to prevent only lacunar infarction and minor infarction associated with atherothrombotic infarction [22]. They are not recommended as first-line therapy for patients with AF and should be considered only when anticoagulation cannot be used. In an analysis of data from the J-RHYTHM registry, antiplatelet use was a negative determinant of warfarin use, suggesting some physicians use antiplatelets as an alternative to warfarin for prevention of thromboembolism in patients with AF in Japan [23]. In the current analysis, 189 patients in the JAPAF study were prescribed antiplatelets. Among these patients, more than half (59.8%) were at high risk for ischemic stroke and three-quarters (75.7%) were at high risk for bleeding.
Limitations
Data were analyzed descriptively, and no statistical analyses were performed. Further, direct comparison was made among subgroups from two different studies. Patient background data were analyzed immediately after DOAC administration became available in Japan. Therefore, as time has elapsed since both studies were conducted, it is possible that the physicians’ treatment trends have already changed. Nevertheless, the study does reflect the surveillance period of the anticoagulant prescriptions in patients with NVAF when knowledge of newer agents was disseminated and incorporated into the guidelines. Finally, generalizability of our results may be limited because this study included only Japanese patients with NVAF.
Conclusions
The results of this descriptive analysis of the transition phase when newer anticoagulants were introduced suggest that most patients prescribed dabigatran were newly diagnosed, non-elderly, and with good renal function. On the other hand, antithrombotic agents, especially warfarin, were continued long-term for patients who were elderly and/or with long duration of AF, with relatively favorable PT-INR control. In addition, patients with high risk of both stroke and bleeding continued treatment with antiplatelets only. These findings suggest that physicians aiming to prevent stroke in patients with AF choose appropriate anticoagulant treatment, taking into consideration individual patient backgrounds as well as the features of each antithrombotic agent.
References
Kodani E, Atarashi H. Prevalence of atrial fibrillation in Asia and the world. J Arrhythm. 2012;28(6):330–7.
Inoue H, Fujiki A, Origasa H, et al. Prevalence of atrial fibrillation in the general population of Japan: an analysis based on periodic health examination. Int J Cardiol. 2009;137(2):102–7.
Inoue H, Atarashi H, Okumura K, et al. Impact of gender on the prognosis of patients with nonvalvular atrial fibrillation. Am J Cardiol. 2014;113(6):957–62.
Gómez-Molina M, Valdés M, Marín F. Oral anticoagulation in Japanese patients with atrial fibrillation—insight to the use of non-vitamin K antagonist oral anticoagulants. Circ J. 2015;79(2):292–4.
JCS Joint Working Group. Guidelines for pharmacotherapy of atrial fibrillation (JCS 2013). Circ J. 2014;78(8):1997–2021.
Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361(12):1139–51.
Granger CB, Alexander JH, McMurray JJ, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365(11):981–92.
Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365(10):883–91.
Giugliano RP, Ruff CT, Braunwald E, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369(22):2093–104.
Graham DJ, Reichman ME, Wernecke M, et al. Cardiovascular, bleeding, and mortality risks in elderly Medicare patients treated with dabigatran or warfarin for nonvalvular atrial fibrillation. Circulation. 2015;131(2):157–64.
Lip GY, Pan X, Kamble S, et al. Major bleeding risk among non-valvular atrial fibrillation patients initiated on apixaban, dabigatran, rivaroxaban or warfarin: a “real-world” observational study in the United States. Int J Clin Pract. 2016;70(9):752–63.
Sharma M, Cornelius VR, Patel JP, Davies JG, Molokhia M. Efficacy and harms of direct oral anticoagulants in the elderly for stroke prevention in atrial fibrillation and secondary prevention of venous thromboembolism: systematic review and meta-analysis. Circulation. 2015;132(3):194–204.
Umei M, Kishi M, Sato T, et al. Indications for suboptimal low-dose direct oral anticoagulants for non-valvular atrial fibrillation patients. J Arrhythm. 2017;33(5):475–82.
Pradaxa® (package insert). Revised March 2018. http://docs.boehringer-ingelheim.com/Prescribing%20Information/PIs/Pradaxa/Pradaxa.pdf. Accessed 28 Nov 2018.
Prazaxa® (Japanese package insert). http://www.info.pmda.go.jp/go/pack/3339001M1024_1_12/. Accessed 28 Nov 2018.
Inoue H, Uchiyama S, Atarashi H, et al. Post-marketing surveillance on the long-term use of dabigatran in Japanese patients with nonvalvular atrial fibrillation: preliminary report of the J-dabigatran surveillance. J Arrhythm. 2016;32(2):145–50.
Kusakawa K, Harada KH, Kagimura T, Koizumi A. Major determinants for the selecting antithrombotic therapies in patients with nonvalvular atrial fibrillation in Japan (JAPAF study). J Arrhythm. 2017;33(2):99–106.
Suzuki S, Otsuka T, Sagara K, et al. Dabigatran in clinical practice for atrial fibrillation with special reference to activated partial thromboplastin time. Circ J. 2012;76:755–7.
Xarelto® (package insert). http://www.info.pmda.go.jp/go/pack/3339003F1024_1_15/. Accessed 28 Nov 2018.
Olesen JB, Lip GY, Hansen ML, et al. Validation of risk stratification schemes for predicting stroke and thromboembolism in patients with atrial fibrillation: nationwide cohort study. BMJ. 2011;342:d124.
Ogawa S, Aonuma K, Tse H-F, et al. The APHRS’s 2013 statement on antithrombotic therapy of patients with nonvalvular atrial fibrillation. J Arrhythm. 2013;29:190–200.
Sato H, Ishikawa K, Kitabatake A, et al. Low-dose aspirin for prevention of stroke in low-risk patients with atrial fibrillation: Japan Atrial Fibrillation Stroke Trial. Stroke. 2006;37(2):447–51.
J-RHYTHM Registry Investigators. Determinants of warfarin use and international normalized ratio levels in atrial fibrillation patients in Japan—subanalysis of the J-RHYTHM Registry. Circ J. 2011;75(10):2357–62.
Acknowledgements
We thank the participants of the studies.
Funding
This study was conducted under the sponsorship of Nippon Boehringer Ingelheim Co., Ltd. Article processing charges were funded by Nippon Boehringer Ingelheim Co., Ltd. All authors had full access to all of the data in this study and take complete responsibility for the integrity of the data and accuracy of the data analysis.
Medical Writing, Editorial, and Other Assistance
Editorial support, in the form of medical writing, assembling tables and creating high-resolution images based on authors’ detailed directions, collating author comments, copyediting, fact checking, and referencing, was provided by Annirudha Chillar, MD, PhD, and Maribeth Bogush, PhD, of Cactus Communications. Support for this assistance was funded by Nippon Boehringer Ingelheim Co., Ltd.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
List of Investigators
A full list of the investigators and study sites is available from a previously published article [17].
Disclosures
Yukihiro Koretsune has received remuneration from Daiichi Sankyo, Boehringer Ingelheim, Bayer Healthcare, Bristol-Myers Squibb, and Pfizer. Koichi Kusakawa was an employee of Nippon Boehringer Ingelheim until January 2013 and currently works in the Department of Health and Environmental Sciences, Kyoto University Graduate School of Medicine, Kyoto, Japan. Kouji H. Harada has received research funding from Boehringer Ingelheim. Akio Koizumi has received research funding from Boehringer Ingelheim. Shinichiro Uchiyama has received remuneration from Boehringer Ingelheim, Bayer Healthcare, Daiichi Sankyo, and Sanofi. Hirotsugu Atarashi has received remuneration from Boehringer Ingelheim and Daiichi Sankyo. Ken Okumura has received remuneration from Boehringer Ingelheim, Bayer Healthcare, Daiichi Sankyo, and Pfizer. Masahiro Yasaka has received remuneration from Boehringer Ingelheim, Bayer Healthcare, and Daiichi Sankyo, and research funding from Boehringer Ingelheim. Takeshi Yamashita has received remuneration from Boehringer Ingelheim, Daiichi Sankyo, Bayer Healthcare, Pfizer, and Bristol-Myers Squibb, and research funding from Daiichi Sankyo, Bayer Healthcare, and Bristol-Myers Squibb. Atsushi Taniguchi is an employee of Nippon Boehringer Ingelheim. Taku Fukaya is an employee of Nippon Boehringer Ingelheim. Hiroshi Inoue has received remuneration from Boehringer Ingelheim, Bayer Healthcare, Daiichi Sankyo, and Bristol-Myers Squibb.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Data Availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Enhanced Digital Features
To view enhanced digital features for this article go to https://doi.org/10.6084/m9.figshare.7637978.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Koretsune, Y., Kusakawa, K., Harada, K.H. et al. Characteristics of Japanese Patients with Nonvalvular Atrial Fibrillation on Anticoagulant Treatment: A Descriptive Analysis of J-dabigatran Surveillance and JAPAF Study. Cardiol Ther 8, 43–54 (2019). https://doi.org/10.1007/s40119-019-0129-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40119-019-0129-2