Abstract
Objective
When superficial tumors are treated with radiotherapy, bolus may be needed to ensure adequate dose delivery to target tissue. The bolus is typically fabricated at the time of computed tomography (CT) simulation, but in many cases, creating a bolus prior to simulation can be more efficient. Therefore, we devised a workflow that would allow for 3D patient scanning at the initial consultation so that bolus can be fabricated by rapid prototyping before CT simulation.
Methods
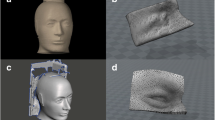
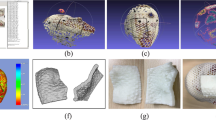
A 3D-printed bolus was fabricated using surface scans of a head phantom that were obtained from a Microsoft Kinect. After processing the scans, a commercially printed 3D bolus was made. To test the feasibility and conformity of the process, masks were made for patients using the above method.
Results
3D-printed bolus created using the rapid scanning technique proved to be the most conformal when compared with bolus made of VPS and SuperFlab. The printed masks also showed that they were formed fitting and comfortable to wear.
Conclusion
We present a new workflow that combines current known methods of both rapidly scanning a patient’s surface and the subsequent rapid creation of bolus that then increases bolus conformity, improves comfort and the patient experience, reduces simulation time, and may decrease exposure to radiation.





Similar content being viewed by others
References
Butson MJ, Cheung T, Yu P, Metcalfe P (2000) Effects on skin dose from unwanted air gaps under bolus in photon beam radiotherapy. Radiat Meas 32(3):201–204. https://doi.org/10.1016/S1350-4487(99)00276-0
Canters RA, Lips IM, Wendling M, Kusters M, van Zeeland M, Gerritsen RM, Poortmans P, Verhoef CG (2016) Clinical implementation of 3D printing in the construction of patient specific bolus for electron beam radiotherapy for non-melanoma skin cancer. Radiother Oncol 121(1):148–153. https://doi.org/10.1016/j.radonc.2016.07.011
Fujimoto K, Shiinoki T, Yuasa Y, Hanazawa H, Shibuya K (2017) Efficacy of patient-specific bolus created using three-dimensional printing technique in photon radiotherapy. Phys Med 38:1–9. https://doi.org/10.1016/j.ejmp.2017.04.023
Kong Y, Yan T, Sun Y, Qian J, Zhou G, Cai S, Tian Y (2019) A dosimetric study on the use of 3D-printed customized boluses in photon therapy: a hydrogel and silica gel study. J Appl Clin Med Phys 20(1):348–355. https://doi.org/10.1002/acm2.12489
Shin B, Venkatramani R, Borker P, Olch A, Grimm J, Wong K (2013) Spatial accuracy of a low cost high resolution 3D surface imaging device for medical applications. Int J Med Phys Clin Eng Radiat Oncol 2(2):45–51. https://doi.org/10.4236/ijmpcero.2013.22007
Cignoni P, Callieri M, Corsini M, Dellepiane M, Ganovelli F, Ranzuglia G (2008) MeshLab: an open-source mesh processing tool. Eurographics Italian Chapter Conference:8 pages. doi:https://doi.org/10.2312/localchapterevents/italchap/italianchapconf2008/129-136
Peltola SM, Melchels FPW, Grijpma DW, Kellomäki M (2008) A review of rapid prototyping techniques for tissue engineering purposes. Ann Med 40(4):268–280. https://doi.org/10.1080/07853890701881788
Zou KH, Warfield SK, Bharatha A, Tempany CM, Kaus MR, Haker SJ, Wells WM 3rd, Jolesz FA, Kikinis R (2004) Statistical validation of image segmentation quality based on a spatial overlap index. Acad Radiol 11(2):178–189. https://doi.org/10.1016/S1076-6332(03)00671-8
Kim S-W, Shin H-J, Kay CS, Son SH (2014) A customized bolus produced using a 3-dimensional printer for radiotherapy. PLoS One 9(10). https://doi.org/10.1371/journal.pone.0110746
Robar JL, Moran K, Allan J et al (2018) Intrapatient study comparing 3D printed bolus versus standard vinyl gel sheet bolus for postmastectomy chest wall radiation therapy. Pract Radiat Oncol 8(4):221–229. https://doi.org/10.1016/j.prro.2017.12.008
LeCompte MC, Chung SA, McKee MM, Marshall TG, Frizzell B, Parker M, Blackstock AW, Farris MK (2019) Simple and rapid creation of customized 3-dimensional printed bolus using iPhone X true depth camera. Pract Radiat Oncol 9(4):e417–e421. https://doi.org/10.1016/j.prro.2019.03.005
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Emi J. Yoshida, MD; Justin M Low, MD; Nicole J.H. Lee, BA; Priya V. Borker, MD; Berthold Shin, MD, MS; Arthur J. Olch, PhD; Rajkumar Venkatramani, MD, MS; Alexander Bruno; Adam Kolawa, BA; Omar Ragab, MD; and Kenneth K. Wong, MD, declare that they have no conflict of interest.
Ethical approval
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Informed consent
Informed consent was obtained from all patients for being included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yoshida, E.J., Low, J.M., Lee, N.J.H. et al. Capturing 3D patient features for rapid prototyping in radiotherapy prior to simulation. J Radiat Oncol 9, 75–80 (2020). https://doi.org/10.1007/s13566-020-00415-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13566-020-00415-1