Abstract
Introduction
Inverse psoriasis is a rare form of psoriasis that affects between 3% and 7% of the patients with psoriasis. It can comprise genital skin folds as part of genital psoriasis, and it is one of the most commonly seen dermatoses of this area. There are few evidence-based studies about the treatment of intertriginous psoriasis involving genital skin folds.
Case Presentation
The authors present a 42-year-old female patient with erythematous plaques in the vulva, groin, and perianal region. The patient had previously received a broad range of topical and systemic therapies that had to be discontinued due to ineffectiveness or side effects. She was treated with 100 mg dapsone daily for 10 months, showing a significant improvement of her cutaneous and mucous lesions. Complete clearance of psoriatic lesions was observed after 4 weeks of treatment. She has remained in remission for up to 2 years, using only topical therapy with tacrolimus 0.1% and calcipotriol.
Discussion
Genital psoriasis is a skin disease that causes great discomfort. It is important to include examination of the genital region and to adopt this conduct in daily clinical practice. Research in this field is still poor, making no discrimination between flexural and genital psoriasis, and is based on case series and expert opinion; therefore, empirical recommendations for the treatment of genital psoriasis remain. Dapsone has been shown to be an effective and convenient alternative for the treatment of inverse psoriasis in genital skin folds, which can provide effective control of the disease. Further studies are required to determine the efficacy and safety of current therapies, and to decide whether dapsone therapy should be considered in the management of this form of psoriasis when topical and other systemic agents are not effective.
Similar content being viewed by others
Introduction
Psoriasis is a chronic inflammatory skin disease involving the epidermis. It is characterized by scaly erythematous plaques and compromise of different body zones, usually with pruritus, and has a significant negative impact on quality of life [1]. The worldwide prevalence of psoriasis is estimated to be 2% [2–4]. Inverse psoriasis, also known as intertriginous or skin-fold psoriasis, is a form of psoriasis that presents itself as erythematous plaques with poor or non-desquamation in skin flexion folds [5]. It affects between 3% and 7% of the patients with psoriasis; however, the actual incidence is still unknown [6]. Inverse psoriasis can compromise genital skin folds as part of genital psoriasis, and it is one of the most commonly seen dermatoses of this area in both females and males [1]. In most cases, genital psoriasis can accompany plaque psoriasis lesions on other parts of the body, but it has also been reported as being isolated to the genital skin; this form of presentation is rare and occurs in only 2–5% of psoriatic patients [7, 8]. Local conditions of intertriginous areas, such as warmth, moisture, and friction, make it susceptible to maceration, fissuring, constant irritation, and absence of scaling, which induces the modified clinical appearance of psoriasis in flexion folds when compared with classical characteristics of psoriasis vulgaris. As a result, differential diagnosis with fungal and sexually transmitted diseases becomes difficult, and resistance to treatment is higher than in other skin zones. Treatment options are limited and difficult to determine because of the lack of evidence-based data, high sensitivity of the area involved, and increased penetration of topical treatments in this vulnerable zone, making it a challenge for the clinician.
There are few evidence-based studies on the treatment of inverse psoriasis involving genital flexion folds, and data reported related to the efficacy and safety are, so far, extremely limited and only supported by expert opinion (level of evidence 5 and recommendation class D) [1]. The evidence-based recommendations suggest the use of weaker topical corticosteroids as a first-line treatment, and vitamin D preparations or tar-based treatments as second-line options [1]. There are reported cases that have used dapsone (Aczone®, Allergan, Marlow, UK) as a treatment option, which has shown great effectiveness and complete remission after 4 weeks of treatment [9]. The case reported in this article is of a female patient with inverse and genital psoriasis successfully treated with dapsone.
Case Presentation
A 42-year-old female patient, without co-morbid conditions, presented with clinical manifestations of 2 years duration, characterized by extensive erythematous and exudative plaques in the groin and vulva, lately appearing intergluteal and perianal intertriginous plaques, and associated with secondary recurrent vulvovaginitis, which had an immensely negative impact on her quality of life and psychosexual wellbeing (Figs. 1, 2).
The patient had previously received a broad range of topical and systemic therapies that had to be discontinued due to ineffectiveness or side effects. A genital skin biopsy was performed, with the results showing superficial interstitial psoriasiform spongiotic and perivascular dermatitis, with signs of lichenification. The patient started treatment with 20 mg methotrexate weekly. Over the next few months the patient had irregular clinical progression with partial therapeutic response, and in addition, presented with recurrent episodes of urinary tract infections. After 4 months of treatment, the patient was changed to 500 mg mycophenolate mofetil (CellCept®, Roche, Welwyn Garden City, UK) twice a day for 2 months, which induced slowly improving clinical results. Due to financial issues and after written informed consent from the patient was obtained, treatment was changed to 100 mg dapsone daily, which produced an excellent response and significant improvement, with complete clearance of cutaneous and mucous psoriatic lesions after 1 month of oral treatment, which was maintained over a period of 10 months of therapy. The patient has remained in remission for up to 2 years after treatment, using only topical therapy with tacrolimus 0.1% and calcipotriol (Figs. 3, 4). No adverse events were recorded.
Discussion
Scientific evidence shows that involvement of the genital skin occurs in 29–40% of patients with psoriasis [10–14]. When there is inverse psoriasis, the genital area is usually involved in up to 79% of the patients [6]. In dermatological consults for chronic symptomatic vulvar disorders, 2% of the cases are caused by psoriasis [15]. Articles that analyzed non-neoplastic biopsies of vulva and vagina reported that 1.8–6.9% of the samples were histologically diagnosed as vulvar psoriasis [16, 17]. In children, vulvar psoriasis was the third most common cutaneous condition among prepubertal girls (9.5–17% of cases) [18, 19]. In males, genital psoriasis of the penis was diagnosed in 3% of patients with alterations of penile skin and genital skin folds [20]. The etiology of inverse and genital psoriasis is still unknown and further studies are needed in order to clarify these diseases [1]. However, as treatment for psoriasis vulgaris is also effective for genital psoriasis, it seems to have a pathophysiology similar to plaque psoriasis in other skins zones. The pathophysiology involves an alteration in the activation of CD4+ and CD8+ T-cells and an anomalous proliferation and differentiation of keratinocytes. It is still not understood as to what causes the disease to commence in this particular zone; the anomalous proliferation and differentiation of keratinocytes suggests that maybe the Koebner phenomenon of constant local mechanical and chemical irritation of flexion folds possibly perpetuates the process [21].
Inverse psoriasis in genital skin folds usually presents itself as erythematous, irregular, well-demarcated, thin, and often symmetrical plaques in the vulva and vagina, with poor or non-desquamation because of the local conditions, as discussed earlier [5, 6, 22–25] and lacks the typical scaling of plaque psoriasis in other skin zones. However, minimal scaling can be seen on the more keratinized regions of the genital skin [26, 27]. The mucosa of the vagina can also be compromised as part of genital psoriasis, showing exudative and bright erythematous plaques, this compromise is less frequently diagnosed in women than in men [26, 28]. Lesions may also have fissures, maceration, and rhagades, and may be accompanied with pruritus, pain, or burning sensation, causing irritation and scratching, producing more plaques through the Koebner phenomenon and local lichenification; therefore, perpetuating the process. Other conditions may also cause irritation, such as sexual intercourse, urine, feces, underwear, clothes, and local infections [27]. Genital psoriasis usually does not produce scarring. However, one case report of two patients described atrophic scarring of the labia minora, mimicking the scarring caused by genital lichen sclerosus [29]. Another condition rarely seen is genital compromise with pustular psoriasis as part of a localized or generalized pustular process, but this complication has only been reported in men [1, 9, 30, 31]. Genital psoriasis can affect not only prepubertal girls, but also small children presenting localized or disseminated psoriatic eruptions in the napkin and genital area [32]. Reports showed that 13% of children with psoriasis had psoriatic napkin eruptions with dissemination, whereas 4% had a localized psoriatic napkin eruption [32], with anogenital psoriasis occurring four-times more often in children over 2 years old than in children under 2 years of age [32].
Diagnosis is based on clinical background, symptoms, clinical signs, and the appearance of skin lesions in the genital area or elsewhere in the body [19, 23, 33, 34]. However, in cases where genital lesions are the only clinical finding, skin biopsy might be an option, showing the same classical histopathological characteristics of non-genital plaque psoriasis, such as Kogoj’s and Munro-Sabouraud’s collections of neutrophils, thickening of the Malpighian layer, hypogranulosis, hyperkeratosis, parakeratosis, and elongation of the papillae [3, 5, 16, 17, 35], but with the slight difference that this findings may be less evident in vulvar and penile psoriatic lesions [17, 29].
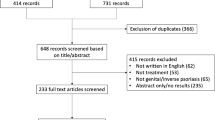
There are numerous therapeutic options for treating psoriasis, which is a therapeutic challenge when it is limited to intertriginous areas such as genital skin flexion folds. So far, there are few evidence-based studies regarding the treatment of inverse psoriasis involving genital flexion folds, and data related to efficacy and safety are extremely limited and only supported by expert opinion (level of evidence 5 and recommendation class D) [1]. In fact, only six casuistic reports and one open-label study have described the effects of therapies used [1], and 24 articles, selected by the only systematic literature review available, reflected the opinion of experts on the preferred treatment for genital psoriasis [1].
Evidence-based recommendations for genital psoriasis indicate the use of short-term topical low-to-medium power corticoids as a first-line treatment option, which can be combined with vitamin D analogs or mild tar preparations [1]. Experts advise the intermittent, short-term use of moderate-to-potent corticosteroids followed by a subsequent gradual shift towards a weaker corticosteroid in cases where weak corticosteroids seem insufficiently potent to induce a response; these treatments should always be monitored for possible local atrophic effects [35–37]. Mild topical coal-tar preparations are the second most advised topical therapy in adults and the first choice for children with napkin plaque psoriasis [1], and are used as an individual topical therapy or combined/alternated therapy with topical steroids [36, 37]. It should be noted that secondary effects have been reported, such as irritation or folliculitis [1, 24, 28, 38]. The use of tar preparations with a steroid preparation has been recommended to reduce irritation [27]. In children, it can also be used mixed with zinc oxide [39, 40]. Topical treatment of vitamin D analogs (such as calcipotriol) has also shown benefits either alone as monotherapy or combined with steroid preparations (to reduce the irritation that these analogs cause), especially in male patients [1, 33]. The use of topical immunomodulator agents, such as tacrolimus or 1% pimecrolimus cream, have shown benefits for long-term therapies [41, 42], and should be regarded as third-line treatment options [1, 24], but patients should be monitored periodically for possible complications, such as local irritation, stinging, irritant or allergic contact dermatitis, candidiasis, and/or (re)activation of viral skin infections [1]. Topical cyclosporine has also shown beneficial effects when used in genital psoriasis of the glans, penis, and prepuce [43]. If concurrent bacterial or fungal infections are present, they should be treated with topical antibiotics or antifungal drugs, and local irritation should be reduced with mild emollients in order to eliminate the possible Koebner effect [1]. If vulvar plaques are resistant to treatment, a biopsy should be carried out to rule out malignancy [44].
Systemic therapies (methotrexate, cyclosporine, oral retinoids, or biological drugs) are used for severe or extensive psoriasis, or when there is a significant negative impact on quality of life [1, 45, 46], but they are not used as common practice for isolated genital psoriasis [1]. Local treatment with topical dithranol (anthralin) and tazarotene should be avoided in the genital area [1, 24, 27]. Laser therapies (excimer, continuous carbon dioxide, erbium, pulsed dye laser) and UV phototherapy are commonly used for localized skin plaque psoriasis [47–50], except for YAG (yttrium–aluminum–garnet) laser, which has been shown not to improve localized plaque psoriasis [51]. However, these treatments are not recommended for genital psoriasis. Moreover, it has been suggested that these modalities should be avoided in inverse psoriasis with compromised genital skin folds [1].
Nonstandard and off-label therapies for psoriasis should be chosen when there is resistance to conventional therapies, when there are multiple side effects, in unusual presentations, or in cases with specific comorbidities [45, 46]. One of these therapies is dapsone, a sulfone initially used for the treatment of leprosy. Nowadays, its use has extended to other inflammatory dermatoses [46]. It has antibiotic, anti-inflammatory, and immunomodulatory properties [46]. MacMillan and Champion first reported the use of dapsone as a treatment for psoriasis in an adult with treatment-resistant generalized pustular psoriasis [52]. Since then it has been used in cases of pustular psoriasis, especially in children [53–59]. Side effects are dose-dependent, hemolysis and methemoglobinemia being the most frequently reported, and more rarely reported agranulocytosis, hypersensitivity syndrome, and peripheral neuropathy [46, 60]. The recommended dosing of dapsone in childhood pustular psoriasis is 1 mg/kg daily, whereas in adults with dermatitis herpetiformis a starting dose of 50 mg daily is recommended, which can be increased, as tolerated, up to 300 mg daily or higher if necessary. The dosage should be reduced to a lower maintenance dose if possible [46]. Dapsone has been chosen by physicians as a treatment option for genital psoriasis; this type of therapeutic regimen was first described in 2008 in a case report by Singh and Thappa [9]. They used dapsone 100 mg daily in a male patient with pustular psoriasis of the penis, the lesions subsided completely after 4 weeks of treatment, similar to the results obtained in the present case. Regarding monitoring, it is recommended that complete blood cell and platelet counts are undertaken weekly for 4 weeks, monthly for 6 months, and then every 6 months, and liver function tests and total bilirubin are performed periodically [46].
In conclusion, genital psoriasis is a skin disease that causes great discomfort. It is important to include an examination of the genital region and to adopt this conduct in daily clinical practice. Thus far, research in this field is poor, making no discrimination between flexural and genital psoriasis, and is based on case series and expert opinion; therefore, recommendations for the treatment of genital psoriasis are empirical. Dapsone has been shown to be an effective and convenient alternative for the treatment of inverse psoriasis in genital skin folds, which can provide effective control of the disease. Further studies are required to determine the efficacy and safety of current therapies, and to decide whether this therapy should be considered in the management of this form of psoriasis when topical and other systemic agents are not effective.
References
Meeuwis K, De Hullu J, Massuger L, Van de Keerkhof P, Van Rossum M. Genital psoriasis: a systematic literature review on this hidden skin disease. Acta Derm Venereol. 2011;91:5–11.
Christophers E. Psoriasis—epidemiology and clinical spectrum. Clin Exp Dermatol. 2001;26:314–20.
Myers WA, Gottlieb AB, Mease P. Psoriasis and psoriatic arthritis: clinical features and disease mechanisms. Clin Dermatol. 2006;24:438–47.
Raychaudhuri SP, Farber EM. The prevalence of psoriasis in the world. J Eur Acad Dermatol Venereol. 2001;15:16–7.
Joham E, James E. Psoriasis. In: Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AM, Leffell DJ, editors. Fitzpatrick’s dermatology in general medicine. New York: McGraw Hill Medicine; 2007. p. 169–94.
Wang G, Li C, Gao T, Liu Y. Clinical analysis of 48 cases of inverse psoriasis: a hospital-based study. Eur J Dermatol. 2005;15:176–8.
Van de Kerkhof PCM. Clinical features. In: van de Kerkhof PCM, editor. Textbook of psoriasis. Oxford: Blackwell Publishing Ltd.; 2003. p. 3–29.
Stoof TJ, van der Meijden WI. Psoriasis. In: van der Meijden WI, ter Harmsel WA, editors. Vulvapathologie. Assen: Koninklijke Van Gorcum BV; 2007. p. 137–46.
Singh N, Thappa DM. Circinate pustular psoriasis localized to glans penis mimicking “circinate balanitis” and responsive to dapsone. Indian J Dermatol Venereol Leprol. 2008;74:388–9.
Hellgren L. Psoriasis. A statistical, clinical and laboratory investigation of 255 psoriatics and matched healthy controls. Acta Derm Venereol. 1964;44:191–207.
Farber EM, Bright RD, Nall ML. Psoriasis. A questionnaire survey of 2,144 patients. Arch Dermatol. 1968;98:248–59.
Farber EM, Nall ML. The natural history of psoriasis in 5,600 patients. Dermatologica. 1974;148:1–18.
Van de Kerkhof PC, de Hoop D, de Korte J, Cobelens SA, Kuipers MV. Patient compliance and disease management in the treatment of psoriasis in the Netherlands. Dermatology. 2000;200:292–8.
Fouéré S, Adjadj L, Pawin H. How patients experience psoriasis: results from a European survey. J Eur Acad Dermatol Venereol. 2005;19:2–6.
Fischer G, Spurrett B, Fischer A. The chronically symptomatic vulva: aetiology and management. Br J Obstet Gynaecol. 1995;102:773–9.
O’Keefe RJ, Scurry JP, Dennerstein G, Sfameni S, Brenan J. Audit of 114 non-neoplastic vulvar biopsies. Br J Obstet Gynaecol. 1995;102:780–6.
Ambros RA, Malfetano JH, Carlson JA, Mihm MC. Nonneoplastic epithelial alterations of the vulva: recognition assessment and comparisons of terminologies used among the various specialties. Mod Pathol. 1997;10:401–8.
Singh N, Thappa DM, Jaisankar TJ, Habeebullah S. Pattern of non-venereal dermatoses of female external genitalia in South India. Dermatol Online J. 2008;14:1.
Fischer G, Rogers M. Vulvar disease in children: a clinical audit of 130 cases. Pediatr Dermatol. 2000;17:1–6.
Kohn FM. Skin changes of the penis. Differentiation between local findings and systemic diseases. MMW Fortschr Med. 2002;144:30–5.
Krueger JG, Bowcock A. Psoriasis pathophysiology: current concepts of pathogenesis. Ann Rheum Dis. 2005;64:30–6.
Lisi P. Differential diagnosis of psoriasis. Reumatismo. 2007;59:56–60.
Rosen T. Update on genital lesions. JAMA. 2003;290:1001–5.
Trager JDK. What’s your diagnosis? Well-demarcated vulvar erythema in two girls. J Pediatr Adolesc Gynecol. 2005;18:43–6.
Eichmann AR. Dermatoses of the male genital area. Dermatology. 2005;210:150–6.
Varghese M, Kindel S. Pigmentary disorders and inflammatory lesions of the external genitalia. Urol Clin North Am. 1992;19:111–21.
Farber EM, Nall L. Genital psoriasis. Cutis. 1992;50:263–6.
Salim A, Wojnarowska F. Skin diseases affecting the vulva. Curr Obstet Gynaecol. 2002;12:81–9.
Albert S, Neill S, Derrick EK, Calonje E. Psoriasis associated with vulval scarring. Clin Exp Dermatol. 2004;29:354–6.
Tolman MM, Moschella SL. Pustular psoriasis (Zumbusch). Arch Dermatol. 1960;81:400–4.
Quan MB, Ruben BS. Pustular psoriasis limited to the penis. Int J Dermatol. 1996;35:202–4.
Morris A, Rogers M, Fischer G, Williams K. Childhood psoriasis: a clinical review of 1,262 cases. Pediatr Dermatol. 2001;18:188–98.
Buechner SA. Common skin disorders of the penis. BJU Int. 2002;90:498–506.
Van Dijk F, Thio HB, Neumann HAM. Non-oncological and non-infectious diseases of the penis (penile lesions). EAU-EBU Update Ser. 2006;41:13–9.
MacLean AB, Roberts DT, Reid WMN. Review of 1,000 women seen at two specially designated vulval clinics. Curr Obstet Gynaecol. 1998;8:159–62.
Welsh B, Howard A, Cook K. Vulval itch. Aust Fam Physician. 2004;337:505–10.
Fischer GO. Vulval disease in pre-pubertal girls. Australas J Dermatol. 2001;424:225–34.
Nunns D. Pruritus vulvae. Curr Obstet Gynaecol. 2002;12:231–4.
Camilleri MJ, Calobrisi SD. Skin eruptions in the diaper area. Curr Probl Dermatol. 1999;11:214–43.
Hogan P. Irritant napkin dermatitis. Aust Fam Physician. 1999;28:385–6.
Kalb RE, Bagel J, Korman NJ, et al. Treatment of intertriginous psoriasis: from the Medical Board of the National Psoriasis Foundation. J Am Acad Dermatol. 2009;60:120–4.
Kreuter A, Sommer A, Hyun J, et al. 1% Pimecrolimus, 0.005% calcipotriol, and 0.1% betamethasone in the treatment of intertriginous psoriasis: a double-blind, randomized controlled study. Arch Dermatol. 2006;142:1138–43.
Jemec GB, Baadsgaard O. Effect of cyclosporine on genital psoriasis and lichen planus. J Am Acad Dermatol. 1993;29:1048–9.
Goldman BD. Common dermatoses of the male genitalia. Recognition of differences in genital rashes and lesions is essential and attainable. Postgrad Med. 2000;108:89–91, 95–6.
Menter A, Korman NJ, Elmets CA, et al. Guidelines of care for the management of psoriasis and psoriatic arthritis: section 4. Guidelines of care for the management and treatment of psoriasis with traditional systemic agents. J Am Acad Dermatol. 2009;61:451–85.
Halverstam C, Lebwohl M. Nonstandard and off-label therapies for psoriasis. Clin Dermatol. 2008;26:546–53.
Feldman SR, Mellen BG, Housman TS, et al. Efficacy of the 308-nm excimer laser for treatment of psoriasis: results of a multicenter study. J Am Acad Dermatol. 2002;46:900–6.
Taibjee SM, Cheung ST, Laube S, Lanigan SW. Controlled study of excimer and pulsed dye lasers in the treatment of psoriasis. Br J Dermatol. 2005;153:960–6.
Spicer MS, Goldberg DJ. Lasers in dermatology. J Am Acad Dermatol. 1996;34:1–25.
Tse Y, Ostad A, Lee HS, et al. A clinical and histologic evaluation of two medium-depth peels: glycolic acid versus Jessner’s trichloroacetic acid. Dermatol Surg. 1996;22:781–6.
Van Lingen RG, de Jong EM, van Erp PE, van Meeteren WS, van De Kerkhof PC, Seyger MM. Nd:YAG laser (1,064 nm) fails to improve localized plaque type psoriasis: a clinical and immunohistochemical pilot study. Eur J Dermatol. 2008;18:671–6.
MacMillan A, Champion R. Generalized pustular psoriasis treated with dapsone. Br J Dermatol. 1973;88:183–5.
Peachey R. Atypical pustular psoriasis treated with dapsone. Br J Dermatol. 1977;97:64–6.
Juanqin G, Zhiqiang C, Zijia H. Evaluation of the effectiveness of childhood generalized pustular psoriasis treatment in 30 cases. Pediatr Dermatol. 1998;15:144–6.
Mazzatenta C, Martini P, Luti L, Domenici R. Diffuse sterile pustular eruption with changing clinical features in a 2-year-old. Pediatr Dermatol. 2005;22:250–3.
Chaves YN, Cardoso DN, Jorge PF, Follador I, Oliveira Mde F. Childhood pustular psoriasis: case report. An Bras Dermatol. 2010;85:899–902.
Staughton R. Infantile generalized pustular psoriasis responding to dapsone. Proc R Soc Med. 1977;70:286–7.
Yu H, Park JW, Park JM, Hwang DK, Park YW. A case of childhood generalized pustular psoriasis treated with dapsone. J Dermatol. 2001;28:316–9.
Farber EM, Nall L. Pustular psoriasis. Cutis. 1993;51:29–32.
EM-Consulte, Elsevier Masson SAS. Dapsona en dermatología. 2005. Available at: http://www.em-consulte.com/es/article/43765. Accessed Sep 27 2011.
Acknowledgments
Dr. Conlledo Villalobos is the guarantor for this article, and takes responsibility for the integrity of the work as a whole. All authors declare having no conflicts of interests of any kind.
Conflict of interest
None.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License (https://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Guglielmetti, A., Conlledo, R., Bedoya, J. et al. Inverse Psoriasis Involving Genital Skin Folds: Successful Therapy with Dapsone. Dermatol Ther (Heidelb) 2, 15 (2012). https://doi.org/10.1007/s13555-012-0015-5
Received:
Published:
DOI: https://doi.org/10.1007/s13555-012-0015-5