Abstract
Purpose
This case report describes the use of ultrasound-guided stellate ganglion blockade to treat sepsis-related digital ischemia in the intensive care unit (ICU).
Clinical features
A 71-yr-old female was admitted to the ICU with septic shock and acute respiratory distress syndrome (ARDS) following an initial right hemicolectomy complicated by an anastomotic leak and peritonitis. The patient’s condition was further complicated by an abdominal abscess 22 days later. She had type-2 diabetes mellitus and hypertension but no history of vascular disease. With continuing sepsis from the abscess and requiring mechanical ventilation due to ARDS, she developed upper limb digital ischemia refractory to treatment with a low dose of dobutamine and isosorbide dinitrate. We subsequently performed ultrasound-guided bilateral stellate ganglion blockade with the intent of restoring perfusion to her fingers before digital necrosis developed. One hour after each stellate ganglion block, the symptoms of digital ischemia completely resolved. The benefit persisted for two days, and then a repeat block was performed with similar results.
Conclusions
This case illustrates the potential advantages of ultrasound-guided stellate ganglion blockade for the treatment of sepsis-related digital ischemia refractory to standard therapy.
Résumé
Objectif
Cette étude de cas décrit l’utilisation du bloc échoguidé du ganglion cervico-thoracique pour traiter une ischémie des doigts secondaire à un sepsis dans une unité des soins intensifs (USI).
Caractéristiques cliniques
Une femme âgée de 71 ans a été hospitalisée à l’USI en état de choc septique avec un syndrome de détresse respiratoire (SDRA) à la suite d’une hémicolectomie droite initiale, compliquée d’une fuite de l’anastomose et d’une péritonite. L’état de la patiente a encore été compliqué par la formation d’un abcès abdominal 22 jours plus tard. Elle avait un diabète de type 2 et une hypertension, mais sans antécédent de maladie vasculaire. Avec la persistance du sepsis dû à l’abcès et la nécessité de la ventilation mécanique en raison du SDRA, elle a développé une ischémie digitale du membre supérieur réfractaire au traitement par faibles doses de dobutamine et de dinitrate d’isosorbide. Nous avons alors réalisé un bloc bilatéral échoguidé du ganglion cervico-thoracique dans le but de restaurer la perfusion de ses doigts avant la survenue d’une nécrose. Une heure après la réalisation de chaque bloc du ganglion cervico-thoracique, les symptômes de l’ischémie des doigts avaient complètement disparu. Ce bénéfice a persisté pendant deux jours et la répétition du bloc a alors entraîné les mêmes résultats.
Conclusions
Ce cas illustre les avantages potentiels du bloc échoguidé du ganglion cervico-thoracique pour le traitement d’une ischémie des doigts secondaire à un sepsis et réfractaire au traitement standard.
Similar content being viewed by others
Severe sepsis can lead to many complications, including shock and multi-organ system failure. Distal limb hypoperfusion can develop and can be further worsened by the administration of vasoconstrictors such as epinephrine or norepinephrine.1 Furthermore, this distal extremity ischemia can lead to infection and the need for amputation. Vasoconstrictor and sepsis-induced microcirculatory alterations2 have been treated with isosorbide dinitrate3 or dobutamine;4 however, their efficiency remains debatable.5,6
The stellate ganglion is the principal sympathetic relay for the upper limbs and participates in the regulation of the microcirculation.7 Stellate ganglion blockade has previously been used to treat patients with vasomotor symptoms,8 refractory ventricular arrhythmias,9 and complex regional pain syndrome type I7 as well as to salvage an ischemic hand caused by vasopressor extravasation.10,11
We report the successful use of ultrasound-guided bilateral stellate ganglion blockade in a patient with sepsis complicated by upper limb digital ischemia unresponsive to standard therapy (i.e., dobutamine and isosorbide dinitrate infusions). This case suggests the potential utility of stellate ganglion blockade in this setting. The family provided consent for publication of this report.
Clinical features
A 71-yr-old female was transferred to our intensive care unit (ICU) in June 2015 with acute respiratory distress syndrome (ARDS) and septic shock following right hemicolectomy for cancer. Her medical history included hypertension, type-2 diabetes mellitus, and depression. The patient had no other history of vascular disease before ICU admission. She had developed peritonitis six days postoperatively due to an anastomotic leak that required subsequent reoperation. She subsequently developed moderately severe ARDS (PaO2/FiO2 ratio of 100-200) requiring mechanical ventilation at the time of ICU admission. The initial septic shock required norepinephrine (maximum dose 0.3 µg·kg−1·min−1) and dobutamine (5 µg·kg−1·min−1) to preserve organ perfusion, which were administered for two days via a central venous catheter. No other vasopressor was used. The patient’s initial lactate level was 4 mmol·L−1 but decreased to normal by the second ICU day. She was treated with antibiotics and underwent hemodynamic optimization.
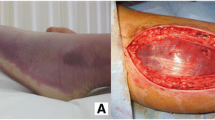
Twenty-two days after the initial operation, she developed severe sepsis (white blood cell count 4,000·mm−3, body temperature 38.5°C, an increase in C-reactive protein from 60-120 mg·L−1, and procalcitonin value 17 ng·mL−1) requiring additional norepinephrine (0.03 µg·kg−1·min−1) for six hours. A computed tomography scan showed an abdominal abscess (5 cm × 15 cm) that was drained under ultrasound control. Enterococcus faecalis (susceptible to linezolid) was isolated and continuous treatment with antibiotics commenced once the abscess was diagnosed. Echocardiography showed no evidence of endocarditis. Before the abdominal abscess was drained, the patient presented with bilateral upper limb digital ischemia affecting all the fingers of both hands (Fig. 2A). The vasopressors were weaned and dobutamine (1 µg·kg−1·min−1) and isosorbide dinitrate (0.3 µg·kg−1·min−1) were administered for two days without benefit.
Ultrasound imaging of left stellate ganglion. The white arrow on the left image (1A) shows the needle path with the anterolateral approach. CA = carotid artery; IJV = internal jugular vein; Th = thyroid; C7 = transverse process of the seventh cervical vertebral body; VA = vertebral artery. The arrow on the right image (1B) shows the needle tip controlled by colour Doppler imaging and hydrolocalization (Doppler colour is due to active injection at the time of imaging). LA = local anesthetic
Doppler imaging of the radial arteries at the level of the wrist showed preserved bilateral perfusion. Worsening of ischemia led us to perform ultrasound-guided bilateral stellate ganglion blockade with the aim of restoring peripheral perfusion and preventing bilateral digital necrosis. The patient had no contraindication to performing regional anesthesia (i.e., sepsis-related coagulopathy - prothrombin ratio 68%, international normalized ratio (INR) 1.2, activated partial thromboplastin time 1.17 times control, and platelet count 231,000·mm−3), and the patient’s family provided informed consent for the procedure.
An experienced anesthesiologist (B.B.) performed the stellate ganglion block beginning on the left side. The transverse process of C7 and the vertebral artery (i.e., anterior to the transverse process of C7) were visualized using a Toshiba AplioTM 300 ultrasound system (Toshiba Medical System—Europe B.V., Zoetermeer, The Netherlands) with an 8-12 MHz linear array probe (Fig. 1A). A StimuQuikTM 50-mm needle (Arrow International Inc., Reading PA, USA) was inserted through the skin lateral to the internal jugular vein, parallel to the ultrasound probe, and advanced obliquely under real-time ultrasound guidance so that the needle tip was lying medially to the vertebral artery. The progression of the needle tip was determined by colour Doppler imaging and hydrodissection (Fig. 1B).12,13 When the needle tip was anterior to the transverse process of C7 and medial to the vertebral artery, 0.5% ropivacaine (15 mL) was injected following negative aspiration. Ropivacaine was injected in divided doses, with real-time ultrasound imaging showing good spread of the local anesthetic in the area of the lower cervical sympathetic chain.
Fifteen minutes after the block was administered, the patient developed vasodilatation of the left upper extremity and her hand was warm with an increase in capillary refilling. One hour after the block, the fingers on her left hand regained their colouration (Fig. 2). There was no significant hemodynamic variation. Two hours after the first block, the anesthesiologist (B.B.) performed a second stellate ganglion block on the opposite (right) side using the same technique. Two days later, the digital ischemia recurred so the blocks were repeated and were equally successful. No additional subsequent blocks were required. On postoperative day 30, the patient received a tracheostomy as she had developed a critical illness neuromyopathy. On postoperative day 40, she was transferred by airplane to another hospital ICU; the digits appeared completely healed at that time. The patient was discharged from the ICU on postoperative day 60.
Discussion
This is a novel case report describing the successful use of ultrasound-guided stellate ganglion blockade to treat digital ischemia due to septic shock that was refractory to conventional dobutamine and isosorbide dinitrate therapy.5,6 Delehanty et al.4 showed that intravenous dobutamine not only increases resting forearm blood flow and decreases resting forearm vascular resistance but also augments the reactive hyperemic flow and improves the vasodilatory response of the forearm vessels to transient ischemic occlusion. Lima et al.3 showed that the clinical manifestations of poor peripheral perfusion in patients with circulatory shock can revert with the use of nitroglycerin. Nevertheless, the above two therapeutic options were not successful in this patient.
The sympathetic cervical chain is composed of superior, middle, intermediate, and inferior cervical ganglia. In 80% of the population, the stellate ganglion is formed by fusion of the inferior cervical ganglion with the first thoracic ganglion.14 The stellate ganglion is located anterior to the neck of the first rib and may extend to the seventh cervical vertebral body (C7). Nevertheless, if the inferior cervical ganglion is not fused with the first thoracic ganglion, the inferior cervical ganglion lies in front of the transverse tubercle of C7. The stellate ganglion lies medial to the scalene muscles, lateral to the trachea and esophagus, anterior to the transverse processes, and posterior to the vertebral artery at the C7 level (Fig. 1A).
Risks associated with ultrasound-guided stellate ganglion block should always be considered when contemplating this modality. These risks include, but are not limited to, hematoma, nerve damage, inadvertent intravascular injection, hypotension, pneumothorax, and puncture of the esophagus or thyroid. Study results by Bhatia et al. showed that the esophagus was situated lateral to the airway at the C7 level in 74% of subjects, which is in close proximity to needle pathways during the anterior approach.15 Based on French guidelines for perimedullary anesthesia,16 a perimedullary block is contraindicated in hemodynamically unstable patients on vasopressor therapy: no low-molecular-weight heparin should be injected within ten hours before and after the block; the platelet number should be > 80,000·mm−3; warfarin therapy should be stopped, and the block should not be attempted until the INR is < 1.5.
We used an anterolateral approach guided by ultrasound imaging to minimize some of the risks linked to stellate ganglion block14—ultrasound can help to identify and potentially avoid the puncture of vessels, nerves, and other soft tissue structures. Moreover, the progression of the needle tip was controlled by colour Doppler imaging and hydrolocalization (Fig. 1B).12,13 The hydrolocalization technique consists of repetitive injections of small volumes of fluid (0.5-1 mL) in order to narrow down the position of the needle tip. The “in-plane” lateral approach was used and the needle was advanced step-by-step toward the targeted structures. Bilateral stellate ganglion blocks were considered possible because the patient was tracheally intubated and mechanically ventilated due to the initial ARDS, therefore minimizing the risk of phrenic or recurrent laryngeal nerve blockade from diffusion of local anesthetic. Wei et al. evaluated 156 ultrasound-guided stellate ganglion blocks performed in 16 patients with complex regional pain syndrome. Their study results showed a 3.8% occurrence of transient hoarseness and no severe side effects were observed.17
In conclusion, this case illustrates the potential advantages of ultrasound-guided stellate block on digital ischemia refractory to standard therapy. Nevertheless, larger studies are necessary to define the optimal modalities.
References
Dellinger RP, Levy MM, Rhodes A, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med 2013; 41: 580-637.
Doerschug KC, Delsing AS, Schmidt GA, Haynes WG. Impairments in microvascular reactivity are related to organ failure in human sepsis. Am J Physiol Heart Circ Physiol 2007; 293: H1065-71.
Lima A, van Genderen ME, van Bommel J, Klijn E, Jansem T, Bakker J. Nitroglycerin reverts clinical manifestations of poor peripheral perfusion in patients with circulatory shock. Crit Care 2014; 18: R126.
Delehanty J, Liang CS, Odorisi ML. Effects of dobutamine on ischemic vasodilation of the forearm in patients with severe congestive heart failure. J Card Fail 1999; 5: 25-30.
van der Voort PH, van Zanten M, Bosman RJ, et al. Testing a conceptual model on early opening of the microcirculation in severe sepsis and septic shock: a randomised controlled pilot study. Eur J Anaesthesiol 2015; 32: 189-98.
Hernandez G, Bruhn A, Luengo C, et al. Effects of dobutamine on systemic, regional and microcirculatory perfusion parameters in septic shock: a randomized, placebo-controlled, double-blind, crossover study. Intensive Care Med 2013; 39: 1435-43.
Zhou Y, Yi X, Xing W, Hu S, Maslov KI, Wang LV. Microcirculatory changes identified by photoacoustic microscopy in patients with complex regional pain syndrome type I after stellate ganglion blocks. J Biomed Opt 2014; 19: 086017.
Walega DR, Rubin LH, Banuvar S, Shulman LP, Maki PM. Effects of stellate ganglion block on vasomotor symptoms: findings from a randomized controlled clinical trial in postmenopausal women. Menopause 2014; 21: 807-14.
Scanlon MM, Gillespie SM, Schaff HV, Cha YM, Wittwer ED. Urgent ultrasound-guided bilateral stellate ganglion blocks in a patient with medically refractory ventricular arrhythmias. Crit Care Med 2015. DOI:10.1097/CCM.0000000000001086.
Tran DQ, Finlayson RJ. Use of stellate ganglion block to salvage an ischemic hand caused by the extravasation of vasopressors. Reg Anesth Pain Med 2005; 30: 405-8.
De Gasperis A, Cosimati F, Lorenzetti A, Rossini P. Stellate ganglion block in the treatment of ischemic syndrome in an upper limb due to accidental intra-arterial injection of pharmacologic substances or narcotics (Italian). Minerva Anestesiol 1990; 56: 1443-5.
Saranteas T, Adoni A, Sidiropoulou T, Paraskeuopoulos T, Kostopanagiotou G. Combined ultrasound imaging and hydrolocalization technique for accurate placement of perineural catheters. Br J Anaesth 2011; 107: 1008-9.
Bloc S, Ecoffey C, Dhonneur G. Controlling needle tip progression during ultrasound-guided regional anesthesia using the hydrolocalization technique. Reg Anesth Pain Med 2008; 33: 382-3.
Narouze S, Vydyanathan A, Patel N. Ultrasound-guided stellate ganglion block successfully prevented esophageal puncture. Pain Physician 2007; 10: 747-52.
Bhatia A, Flamer D, Peng PW. Evaluation of sonoanatomy relevant to performing stellate ganglion blocks using anterior and lateral simulated approaches: an observational study. Can J Anesth 2012; 59: 1040-7.
Anonymous. Les blocs périmédullaires chez l’adulte. Ann Fr Anesth Reanim 2007; 26: 720-52.
Wei K, Feldmann RE Jr, Brascher AK, Benrath J. Ultrasound-guided stellate ganglion blocks combined with pharmacological and occupational therapy in Complex Regional Pain Syndrome (CRPS): a pilot case series ad interim. Pain Med 2014; 15: 2120-7.
Conflicts of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author contributions
Benoît Bataille, Bastian Nucci, Michel Mora, Stein Silva, Pierre Cocquet have made substantial contributions to the design and interpretation of this case report. Benoît Bataille has performed the ultrasound-guided stellate ganglion blocks. Benoît Bataille and Bastian Nucci have written the manuscript. All authors agree to the conditions outlined in the Instructions for Authors.
Rights and permissions
About this article
Cite this article
Bataille, B., Nucci, B., Mora, M. et al. Ultrasound-guided bilateral stellate ganglion blockade to treat digital ischemia in a patient with sepsis: a case report. Can J Anesth/J Can Anesth 63, 56–60 (2016). https://doi.org/10.1007/s12630-015-0503-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-015-0503-z