Abstract
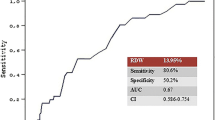
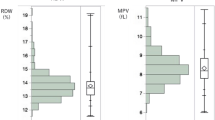
We aimed to investigate whether red cell distribution width (RDW) was associated with periprocedural myocardial infarction (PMI) in patients undergoing elective percutaneous coronary intervention (PCI). Among 1723 consecutive patients undergoing elective PCI, a total of 230 (13.3%) met the diagnostic criteria of PMI. The high RDW (≥ 12.6%) group tended to have PMI (15.4% vs. 11.2%, P = 0.010). RDW was an independent predictor of PMI whether as a categorical variable (adjusted odds ratio = 1.442, 95% confidence interval = 1.088 to 1.911, P = 0.011) or a continuous variable (adjusted odds ratio = 1.236, 95% confidence interval = 1.079 to 1.415, P = 0.002). High RDW was also significantly associated with increased risk of major adverse cardiovascular events (MACE) during follow-up. However, anemia was not independently associated with PMI or MACE in the current study. In conclusion, RDW showed strong and independent association with PMI in patients undergoing elective PCI.



Similar content being viewed by others
Abbreviations
- CI:
-
Confidence interval
- CRP:
-
C-reactive protein
- cTnT:
-
Cardiac troponin T
- HR:
-
Hazard ratio
- MACE:
-
Major adverse cardiovascular events
- MCH:
-
Mean corpuscular hemoglobin
- MCHC:
-
Mean corpuscular hemoglobin concentration
- MCV:
-
Mean corpuscular volume
- OR:
-
Odds ratio
- PCI:
-
Percutaneous coronary intervention
- PMI:
-
Periprocedural myocardial infarction
- RDW:
-
Red cell distribution width
References
Salvagno, G. L., Sanchis-Gomar, F., Picanza, A., et al. (2015). Red blood cell distribution width: a simple parameter with multiple clinical applications. Critical Reviews in Clinical Laboratory Sciences, 52(2), 86–105.
Bessman, J. D., Gilmer, P. J., & Gardner, F. H. (1983). Improved classification of anemias by MCV and RDW. American Journal of Clinical Pathology, 80(3), 322–326.
Felker, G. M., Allen, L. A., Pocock, S. J., et al. (2007). Red cell distribution width as a novel prognostic marker in heart failure: data from the CHARM program and the Duke Databank. Journal of the American College of Cardiology, 50(1), 40–47.
Pascual-Figal, D. A., Bonaque, J. C., Redondo, B., et al. (2009). Red blood cell distribution width predicts long-term outcome regardless of anemia status in acute heart failure patients. European Journal of Heart Failure, 11(9), 840–846.
Jackson, C. E., Dalzell, J. R., Bezlyak, V., et al. (2009). Red cell distribution width has incremental prognostic value to B-type natriuretic peptide in acute heart failure. European Journal of Heart Failure, 11(12), 1152–1154.
Forhecz, Z., Gombos, T., Borgulya, G., et al. (2009). Red cell distribution width in heart failure: prediction of clinical events and relationship with markers of ineffective erythropoiesis, inflammation, renal function, and nutritional state. American Heart Journal, 158(4), 659–666.
Tonelli, M., Sacks, F., Arnold, M., et al. (2008). Relation between red blood cell distribution width and cardiovascular event rate in people with coronary disease. Circulation, 117(2), 163–168.
Lippi, G., Filippozzi, L., Montagnana, M., et al. (2009). Clinical usefulness of measuring red blood cell distribution width on admission in patients with acute coronary syndromes. Clinical Chemistry and Laboratory Medicine, 47(3), 353–357.
Lee, K. H., Park, H. W., Cho, J. G., et al. (2015). Red cell distribution width as a novel predictor for clinical outcomes in patients with paroxysmal atrial fibrillation. Europace, 17(Suppl 2), i83–i88.
Baggen, V., van den Bosch, A. E., van Kimmenade, R. R., et al. (2018). Red cell distribution width in adults with congenital heart disease: a worldwide available and low-cost predictor of cardiovascular events. International Journal of Cardiology, 260, 60–65.
Prasad, A., Singh, M., Lerman, A., et al. (2006). Isolated elevation in troponin T after percutaneous coronary intervention is associated with higher long-term mortality. Journal of the American College of Cardiology, 48(9), 1765–1770.
Feldman, D. N., Kim, L., Rene, A. G., et al. (2011). Prognostic value of cardiac troponin-I or troponin-T elevation following nonemergent percutaneous coronary intervention: a meta-analysis. Catheterization and Cardiovascular Interventions, 77(7), 1020–1030.
Babu, G. G., Walker, J. M., Yellon, D. M., et al. (2011). Peri-procedural myocardial injury during percutaneous coronary intervention: an important target for cardioprotection. European Heart Journal, 32(1), 23–31.
Park, D. W., Kim, Y. H., Yun, S. C., et al. (2013). Frequency, causes, predictors, and clinical significance of peri-procedural myocardial infarction following percutaneous coronary intervention. European Heart Journal, 34(22), 1662–1669.
Jeremias, A., & Kirtane, A. (2008). Balancing efficacy and safety of drug-eluting stents in patients undergoing percutaneous coronary intervention. Annals of Internal Medicine, 148(3), 234–238.
Uyarel, H., Ergelen, M., Cicek, G., et al. (2011). Red cell distribution width as a novel prognostic marker in patients undergoing primary angioplasty for acute myocardial infarction. Coronary Artery Disease, 22(3), 138–144.
Isik, T., Kurt, M., Ayhan, E., et al. (2012). The impact of admission red cell distribution width on the development of poor myocardial perfusion after primary percutaneous intervention. Atherosclerosis, 224(1), 143–149.
Isik, T., Kurt, M., Tanboga, I. H., et al. (2016). The impact of admission red cell distribution width on long-term cardiovascular events after primary percutaneous intervention: a four-year prospective study. Cardiology Journal, 23(3), 281–288.
Bozorgi, A., Khaki, S., Mortazavi, S. H., et al. (2016). Effect of baseline red blood cell distribution width on short- and intermediate-term mortality of patients under primary percutaneous coronary intervention: a survival analysis. Critical Pathways in Cardiology, 15(2), 69–74.
Poludasu, S., Marmur, J. D., Weedon, J., et al. (2009). Red cell distribution width (RDW) as a predictor of long-term mortality in patients undergoing percutaneous coronary intervention. Thrombosis and Haemostasis, 102(3), 581–587.
Tsuboi, S., Miyauchi, K., Kasai, T., et al. (2013). Impact of red blood cell distribution width on long-term mortality in diabetic patients after percutaneous coronary intervention. Circulation Journal, 77(2), 456–461.
Yao, H. M., Sun, T. W., Zhang, X. J., et al. (2014). Red blood cell distribution width and long-term outcome in patients undergoing percutaneous coronary intervention in the drug-eluting stenting era: a two-year cohort study. PLoS One, 9(4), e94887.
Wu, T. T., Zheng, Y. Y., Hou, X. G., et al. (2019). Red blood cell distribution width as long-term prognostic markers in patients with coronary artery disease undergoing percutaneous coronary intervention. Lipids in Health and Disease, 18(1), 140.
Thygesen, K., Alpert, J. S., Jaffe, A. S., et al. (2018). Fourth universal definition of myocardial infarction (2018). Journal of the American College of Cardiology, 72(18), 2231–2264.
Blankenship, J. C., Haldis, T., Feit, F., et al. (2006). Angiographic adverse events, creatine kinase-MB elevation, and ischemic end points complicating percutaneous coronary intervention (a REPLACE-2 substudy). The American Journal of Cardiology, 97(11), 1591–1596.
Lippi, G., Targher, G., Montagnana, M., et al. (2009). Relation between red blood cell distribution width and inflammatory biomarkers in a large cohort of unselected outpatients. Archives of Pathology & Laboratory Medicine, 133(4), 628–632.
Faquin, W. C., Schneider, T. J., & Goldberg, M. A. (1992). Effect of inflammatory cytokines on hypoxia-induced erythropoietin production. Blood, 79(8), 1987–1994.
Weiss, G., & Goodnough, L. T. (2005). Anemia of chronic disease. The New England Journal of Medicine, 352(10), 1011–1023.
Ghaffari, S. (2008). Oxidative stress in the regulation of normal and neoplastic hematopoiesis. Antioxidants & Redox Signaling, 10(11), 1923–1940.
Qing, P., Luo, S. H., Guo, Y. L., et al. (2013). Evaluation of red blood cell distribution width in patients with cardiac syndrome X. Disease Markers, 34(5), 333–339.
Akpinar, I., Sayin, M. R., Gursoy, Y. C., et al. (2014). Plateletcrit and red cell distribution width are independent predictors of the slow coronary flow phenomenon. Journal of Cardiology, 63(2), 112–118.
Ghaffari, S., Tajlil, A., Aslanabadi, N., et al. (2017). Clinical and laboratory predictors of coronary slow flow in coronary angiography. Perfusion, 32(1), 13–19.
Luo, S. H., Jia, Y. J., Nie, S. P., et al. (2013). Increased red cell distribution width in patients with slow coronary flow syndrome. Clinics, 68(6), 732–737.
Karabulut, A., Uyarel, H., Uzunlar, B., et al. (2012). Elevated red cell distribution width level predicts worse postinterventional thrombolysis in myocardial infarction flow reflecting abnormal reperfusion in acute myocardial infarction treated with a primary coronary intervention. Coronary Artery Disease, 23(1), 68–72.
Yaylali, Y. T., Susam, I., Demir, E., et al. (2013). Increased red blood cell deformability and decreased aggregation as potential adaptive mechanisms in the slow coronary flow phenomenon. Coronary Artery Disease, 24(1), 11–15.
McKechnie, R. S., Smith, D., Montoye, C., et al. (2004). Prognostic implication of anemia on in-hospital outcomes after percutaneous coronary intervention. Circulation, 110(3), 271–277.
Lee, P. C., Kini, A. S., Ahsan, C., et al. (2004). Anemia is an independent predictor of mortality after percutaneous coronary intervention. Journal of the American College of Cardiology, 44(3), 541–546.
Dai, Y., Konishi, H., Takagi, A., et al. (2014). Red cell distribution width predicts short- and long-term outcomes of acute congestive heart failure more effectively than hemoglobin. Experimental and Therapeutic Medicine, 8(2), 600–606.
Funding
This study was supported by the National Natural Science Foundation of China (Grant No: 81970295, 81870267, 81670318 and 81570314), Grant of Shanghai Municipal Commission of Health and Family Planning (Grant No: 2017YQ057), Grant of Shanghai Science and Technology Committee (Grant No: 17411962300), the National Program on Key Basic Research Project of China (973 Program, Grant No: 2014CBA02003), Program for Outstanding Medical Academic Leader (Grant No: 2015-Weijiwei-24), Grant of Zhongshan Hospital Affiliated to Fudan University (Grant No: 2015ZSYXGG07 and 2017ZSYQ08), VG Funding of Clinical Trials (2017-CCA-VG-036), and Merck Funding (Xinxin-merck-fund-051).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human Subjects/Informed Consent Statement
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. This study was approved by the Ethics Committee of Zhongshan Hospital (Approval No.: B2019-052; Date: 2019-02-28), and informed consent was obtained from all patients for being included in the study.
Additional information
Associate Editor Craig M. Stolen oversaw the review of this article
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
ESM 1
(DOC 115 kb)
Rights and permissions
About this article
Cite this article
Dai, C., Chen, Z., Qian, J. et al. Red Cell Distribution Width as a Marker of Periprocedural Myocardial Infarction in Patients with Elective Percutaneous Coronary Intervention. J. of Cardiovasc. Trans. Res. 14, 449–456 (2021). https://doi.org/10.1007/s12265-020-10073-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12265-020-10073-w