Abstract
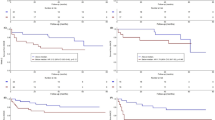
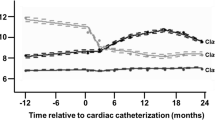
It remains unclear if the developmental trajectories of a specific inflammatory biomarker during the acute phase of ST-elevation myocardial infarction (STEMI) provide outcome prediction. By applying latent class growth modeling (LCGM), we identified three distinctive trajectories of CD14++CD16+ monocytes using serial flow cytometry assays from day 1 to day 7 of symptom onset in 96 de novo STEMI patients underwent primary percutaneous coronary intervention. Membership in the high-hump-shaped trajectory (16.8%) independently predicted adverse cardiovascular outcomes during a median follow-up of 2.5 years. Moreover, inclusion of CD14++CD16+ monocyte trajectories significantly improved area under the curve (AUC) when added to left ventricular ejection fraction-based prediction model (ΔAUC = 0.093, P = 0.013). Therefore, CD14++CD16+ monocyte trajectories during STEMI hospitalization are a novel risk factor for post-STEMI adverse outcomes. These results provide the first proof-of-principle evidence in support of the risk stratification role of LCGM-based longitudinal modeling of specific inflammatory markers during acute STEMI.





Similar content being viewed by others
Abbreviations
- BP:
-
Blood pressure
- CHD:
-
Coronary heart disease
- CI:
-
Confidence interval
- FCM:
-
Flow cytometry
- FMO:
-
Fluorescence Minus One
- HR:
-
Hazard ratio
- LCGM:
-
Latent class growth modeling
- LVEF:
-
Left ventricular ejection fraction
- MACE:
-
Major adverse cardiovascular events
- MI:
-
Myocardial infarction
- OR:
-
Odds ratio
- PCI:
-
Percutaneous coronary intervention
- ROC:
-
Receiver operator characteristic curve
- STEMI:
-
ST-elevation myocardial infarction
- WBC:
-
White blood cell
References
Frangogiannis, N. G. (2014). The inflammatory response in myocardial injury, repair, and remodelling. Nature Reviews Cardiology, 11(5), 255–265.
Seropian, I. M., Toldo, S., Van Tassell, B. W., & Abbate, A. (2014). Anti-inflammatory strategies for ventricular remodeling following ST-segment elevation acute myocardial infarction. Journal of the American College of Cardiology, 63(16), 1593–1603.
Westman, P. C., Lipinski, M. J., Luger, D., Waksman, R., Bonow, R. O., Wu, E., et al. (2016). Inflammation as a driver of adverse left ventricular remodeling after acute myocardial infarction. Journal of the American College of Cardiology, 67(17), 2050–2060.
Swirski, F. K., & Nahrendorf, M. (2013). Leukocyte behavior in atherosclerosis, myocardial infarction, and heart failure. Science, 339(6116), 161–166.
Panizzi, P., Swirski, F. K., Figueiredo, J. L., Waterman, P., Sosnovik, D. E., Aikawa, E., et al. (2010). Impaired infarct healing in atherosclerotic mice with Ly-6C(hi) monocytosis. Journal of the American College of Cardiology, 55(15), 1629–1638.
Tapp, L. D., Shantsila, E., Wrigley, B. J., Pamukcu, B., & Lip, G. Y. (2012). The CD14++CD16+ monocyte subset and monocyte-platelet interactions in patients with ST-elevation myocardial infarction. Journal of Thrombosis and Haemostasis, 10(7), 1231–1241.
Dutta, P., Courties, G., Wei, Y., Leuschner, F., Gorbatov, R., Robbins, C. S., et al. (2012). Myocardial infarction accelerates atherosclerosis. Nature, 487(7407), 325–329.
Ziegler-Heitbrock, L., Ancuta, P., Crowe, S., Dalod, M., Grau, V., Hart, D. N., et al. (2010). Nomenclature of monocytes and dendritic cells in blood. Blood, 116(16), e74–e80.
Zhou, X., Zhang, L., Ji, W. J., Yuan, F., Guo, Z. Z., Pang, B., et al. (2013). Variation in dietary salt intake induces coordinated dynamics of monocyte subsets and monocyte-platelet aggregates in humans: implications in end organ inflammation. PLoS One, 8(4), e60332.
Rogacev, K. S., Cremers, B., Zawada, A. M., Seiler, S., Binder, N., Ege, P., et al. (2012). CD14++CD16+ monocytes independently predict cardiovascular events: a cohort study of 951 patients referred for elective coronary angiography. Journal of the American College of Cardiology, 60(16), 1512–1520.
Rogacev, K. S., Seiler, S., Zawada, A. M., Reichart, B., Herath, E., Roth, D., et al. (2011). CD14++CD16+ monocytes and cardiovascular outcome in patients with chronic kidney disease. European Heart Journal, 32(1), 84–92.
Zhou, X., Liu, X. L., Ji, W. J., Liu, J. X., Guo, Z. Z., Ren, D., et al. (2016). The kinetics of circulating monocyte subsets and monocyte-platelet aggregates in the acute phase of ST-elevation myocardial infarction: associations with 2-year cardiovascular events. Medicine (Baltimore), 95(18), e3466.
Nagin, D. S., & Odgers, C. L. (2010). Group-based trajectory modeling in clinical research. Annual Review of Clinical Psychology, 6, 109–138.
Allen, N. B., Siddique, J., Wilkins, J. T., Shay, C., Lewis, C. E., Goff, D. C., et al. (2014). Blood pressure trajectories in early adulthood and subclinical atherosclerosis in middle age. JAMA, 311(5), 490–497.
Song, M., Hu, F. B., Wu, K., Must, A., Chan, A. T., Willett, W. C., et al. (2016). Trajectory of body shape in early and middle life and all cause and cause specific mortality: results from two prospective US cohort studies. BMJ, 353, i2195.
Ginhoux, F., & Jung, S. (2014). Monocytes and macrophages: developmental pathways and tissue homeostasis. Nature Reviews Immunology, 14(6), 392–404.
Lei, Q., Zhou, X., Zhou, Y. H., Mai, C. Y., Hou, M. M., Lv, L. J., et al. (2016). Prehypertension during normotensive pregnancy and postpartum clustering of cardiometabolic risk factors: a prospective cohort study. Hypertension, 68(2), 455–463.
Steg, P. G., James, S. K., Atar, D., Badano, L. P., Blomstrom-Lundqvist, C., Borger, M. A., et al. (2012). ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. European Heart Journal, 33(20), 2569–2619.
Zhou, X., Yuan, F., Ji, W. J., Guo, Z. Z., Zhang, L., Lu, R. Y., et al. (2014). High-salt intake induced visceral adipose tissue hypoxia and its association with circulating monocyte subsets in humans. Obesity (Silver Spring), 22(6), 1470–1476.
Ma, Y. C., Zuo, L., Chen, J. H., Luo, Q., Yu, X. Q., Li, Y., et al. (2006). Modified glomerular filtration rate estimating equation for Chinese patients with chronic kidney disease. J Am Soc Nephrol, 17(10), 2937–2944.
Jones, B. L., & Nagin, D. S. (2012). A note on a Stata plugin for estimating group-based trajectory models. Sociological Methods & Research, 42(4), 608–613.
Nagin, D. S. (2005). Group-based modeling of development. Cambridge: Harvard University Press.
Kagura, J., Adair, L. S., Munthali, R. J., Pettifor, J. M., & Norris, S. A. (2016). Association between early life growth and blood pressure trajectories in black south African children. Hypertension, 68(5), 1123–1131.
Theodore, R. F., Broadbent, J., Nagin, D., Ambler, A., Hogan, S., Ramrakha, S., et al. (2015). Childhood to early-midlife systolic blood pressure trajectories: early-life predictors, effect modifiers, and adult cardiovascular outcomes. Hypertension, 66(6), 1108–1115.
Niyonkuru, C., Wagner, A. K., Ozawa, H., Amin, K., Goyal, A., & Fabio, A. (2013). Group-based trajectory analysis applications for prognostic biomarker model development in severe TBI: a practical example. Journal of Neurotrauma, 30(11), 938–945.
Cole, D. R., Singian, E. B., & Katz, L. N. (1954). The long-term prognosis following myocardial infarction, and some factors which affect it. Circulation, 9(3), 321–334.
Palmerini, T., Mehran, R., Dangas, G., Nikolsky, E., Witzenbichler, B., Guagliumi, G., et al. (2011). Impact of leukocyte count on mortality and bleeding in patients with myocardial infarction undergoing primary percutaneous coronary interventions: analysis from the harmonizing outcome with revascularization and stent in acute myocardial infarction trial. Circulation, 123(24), 2829–2837 2827 p following 2837.
Chia, S., Nagurney, J. T., Brown, D. F., Raffel, O. C., Bamberg, F., Senatore, F., et al. (2009). Association of leukocyte and neutrophil counts with infarct size, left ventricular function and outcomes after percutaneous coronary intervention for ST-elevation myocardial infarction. The American Journal of Cardiology, 103(3), 333–337.
Horne, B. D., Anderson, J. L., John, J. M., Weaver, A., Bair, T. L., Jensen, K. R., et al. (2005). Which white blood cell subtypes predict increased cardiovascular risk? Journal of the American College of Cardiology, 45(10), 1638–1643.
Ammirati, E., Cannistraci, C. V., Cristell, N. A., Vecchio, V., Palini, A. G., Tornvall, P., et al. (2012). Identification and predictive value of interleukin-6+ interleukin-10+ and interleukin-6- interleukin-10+ cytokine patterns in ST-elevation acute myocardial infarction. Circulation Research, 111(10), 1336–1348.
Ruparelia, N., Godec, J., Lee, R., Chai, J. T., Dall’Armellina, E., McAndrew, D., et al. (2015). Acute myocardial infarction activates distinct inflammation and proliferation pathways in circulating monocytes, prior to recruitment, and identified through conserved transcriptional responses in mice and humans. European Heart Journal, 36(29), 1923–1934.
Zawada, A. M., Rogacev, K. S., Rotter, B., Winter, P., Marell, R. R., Fliser, D., et al. (2011). SuperSAGE evidence for CD14++CD16+ monocytes as a third monocyte subset. Blood, 118(12), e50–e61.
Italiani, P., & Boraschi, D. (2014). From monocytes to M1/M2 macrophages: phenotypical vs. functional differentiation. Frontiers in Immunology, 5, 514.
Heidt, T., Sager, H. B., Courties, G., Dutta, P., Iwamoto, Y., Zaltsman, A., et al. (2014). Chronic variable stress activates hematopoietic stem cells. Nature Medicine, 20(7), 754–758.
Wong, K. L., Tai, J. J., Wong, W. C., Han, H., Sem, X., Yeap, W. H., et al. (2011). Gene expression profiling reveals the defining features of the classical, intermediate, and nonclassical human monocyte subsets. Blood, 118(5), e16–e31.
Foster, G. A., Gower, R. M., Stanhope, K. L., Havel, P. J., Simon, S. I., & Armstrong, E. J. (2013). On-chip phenotypic analysis of inflammatory monocytes in atherogenesis and myocardial infarction. Proceedings of the National Academy of Sciences of the United States of America, 110(34), 13944–13949.
Weber, C., Shantsila, E., Hristov, M., Caligiuri, G., Guzik, T., Heine, G. H., et al. (2016). Role and analysis of monocyte subsets in cardiovascular disease. Joint consensus document of the European Society of Cardiology (ESC) Working Groups “Atherosclerosis & Vascular Biology” and “Thrombosis”. Thrombosis and Haemostasis, 116(4), 626–637.
Tallone, T., Turconi, G., Soldati, G., Pedrazzini, G., Moccetti, T., & Vassalli, G. (2011). Heterogeneity of human monocytes: an optimized four-color flow cytometry protocol for analysis of monocyte subsets. Journal of Cardiovascular Translational Research, 4(2), 211–219.
Thomas, G. D., Hamers, A. A. J., Nakao, C., Marcovecchio, P., Taylor, A. M., McSkimming, C., et al. (2017). Human blood monocyte subsets: a new gating strategy defined using cell surface markers identified by mass cytometry. Arteriosclerosis, Thrombosis, and Vascular Biology, 37(8), 1548–1558.
Funding
This work was supported by the National Natural Science Foundation of China (81570335) and Intra-mural research grants from Pingjin Hospital (FYZ201402, FYZ201605).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
This study was approved by the Ethical Committee of Pingjin Hospital and performed in accordance with the Declaration of Helsinki.
Informed Consent
Informed written consent was obtained from all participants for being included in the study.
Electronic supplementary material
ESM 1
(DOCX 489 kb)
Rights and permissions
About this article
Cite this article
Zeng, S., Yan, LF., Luo, YW. et al. Trajectories of Circulating Monocyte Subsets After ST-Elevation Myocardial Infarction During Hospitalization: Latent Class Growth Modeling for High-Risk Patient Identification. J. of Cardiovasc. Trans. Res. 11, 22–32 (2018). https://doi.org/10.1007/s12265-017-9782-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12265-017-9782-9