Abstract
Background
The long-term effectiveness of Roux-en-Y gastric bypass (RYGB) and single-anastomosis duodeno-ileostomy with sleeve gastrectomy (SADI-S) is unknown.
Purpose
Compare the long-term outcomes.
Setting
Single private institute, USA.
Materials and Methods
Data from 1254 patients who underwent primary RYGB or SADI-S were used for a retrospective matched cohort. Data were obtained by matching every RYGB patient to a SADI-S patient of the same sex, body mass index (BMI), and weight. Only patients out 5 years and had at least one > 5-year follow-up visit were included.
Results
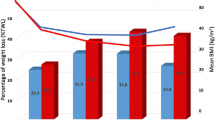
The matched cohort included 61 RYGB and 61 SADI-S patients. There was no statistical, demographic difference between the two groups. At 5 years, a 100% follow-up was available in each group. The intraoperative outcomes were significantly better with SADI-S. The 30-day readmission, reoperation, emergency department (ED) visits, and complication rates were statistically similar between the two groups. The long-term complication rates, Clavien-Dindo grade IIIb complications, and number of patients with more than one complication were significantly lower with SADI-S. Weight loss was significantly greater in the SADI-S group at 5 years. The long-term weight-loss failure rate was significantly higher in the RYGB group. The SADI-S procedure was associated with fewer reintervention through 6 years (14.7% patients vs. 39.3% patients, p = 0.001). Conversion or reversal of the procedure was required only in the RYGB group. There also was no significant difference in nutritional outcomes between the two procedures.
Conclusions
This study showed that problems, including long-term complications, reinterventions, weight-loss failure, and conversion, were more often associated with RYGB than with SADI-S. The SADI-S may be considered one of the viable alternatives to RYGB.
Similar content being viewed by others
References
Mason EE, Ito C. Gastric bypass in obesity. Surg Clin North Am. 1967;47(6):1345–51. https://doi.org/10.1016/s0039-6109(16)38384-0.
English WJ, DeMaria EJ, Hutter MM, et al. American Society for Metabolic and Bariatric Surgery 2018 estimate of metabolic and bariatric procedures performed in the United States. Surg Obes Relat Dis. 2020;16(4):457–63.
English WJ, DeMaria EJ, Brethauer SA, et al. American Society for Metabolic and Bariatric Surgery estimation of metabolic and bariatric procedures performed in the United States in 2016. Surg Obes Relat Dis. 2018;14(3):259–63. https://doi.org/10.1016/j.soard.2017.12.013.
Surve A, Cottam D, Medlin W, et al. Long-term outcomes of primary single-anastomosis duodeno-ileal bypass with sleeve gastrectomy (SADI-S). Surg Obes Relat Dis. 2020;31:S1550–7289(20)30422–6. https://doi.org/10.1016/j.soard.2020.07.019.
Sánchez-Pernaute A, Rubio MÁ, Cabrerizo L, et al. Single-anastomosis duodenoileal bypass with sleeve gastrectomy (SADI-S) for obese diabetic patients. Surg Obes Relat Dis. 2015;11(5):1092–8.
Surve A, Cottam D, Zaveri H, et al. Single anastomosis duodeno-ileostomy. In: Nguyen N, Brethauer S, Morton J, Ponce J, Rosenthal R, editors. The ASMBS textbook of bariatric surgery. Cham: Springer; 2020.
Surve A, Cottam D, Sanchez-Pernaute A, et al. The incidence of complications associated with loop duodeno-ileostomy after single-anastomosis duodenal switch procedures among 1328 patients: a multicenter experience. Surg Obes Relat Dis. 2018;14(5):594–601. https://doi.org/10.1016/j.soard.2018.01.020.
Surve A, Zaveri H, Cottam D, et al. A retrospective comparison of biliopancreatic diversion with duodenal switch with single anastomosis duodenal switch (SIPS-stomach intestinal pylorus sparing surgery) at a single institution with two year follow-up. Surg Obes Relat Dis. 2017;13(3):415–22.
Surve A, Zaveri H, Cottam D, et al. Mid-term outcomes of gastric bypass weight loss failure to duodenal switch. Surg Obes Relat Dis. 2016;12(9):1663–70.
Surve A, Zaveri H, Cottam D. A step-by-step surgical technique video with two reported cases of common channel lengthening in patients with previous stomach intestinal pylorus sparing surgery to treat chronic diarrhea. Surg Obes Relat Dis. 2017;13(4):706–9.
Surve A, Zaveri H, Cottam D. Retrograde filling of the afferent limb as a cause of chronic nausea after single anastomosis loop duodenal switch. Surg Obes Relat Dis. 2016;12(4):e39–42.
Surve A, Zaveri H, Cottam D, et al. Laparoscopic stomach intestinal pylorus-sparing surgery as a revisional option after failed adjustable gastric banding: a report of 27 cases with 36-month follow-up. Surg Obes Relat Dis. 2018;14(8):1139–48. https://doi.org/10.1016/j.soard.2018.05.001.
Surve A, Zaveri H, Cottam D. A safer and simpler technique of duodenal dissection and transection of the duodenal bulb for duodenal switch. Surg Obes Relat Dis. 2016;12(4):923–4.
Surve A, Cottam D, Horsley B. Internal hernia following primary laparoscopic SADI-S: the first reported case. Obes Surg. 2020;30(5):2066–8. https://doi.org/10.1007/s11695-020-04444-0.
Mitzman B, Cottam D, Goriparthi R, et al. Stomach intestinal pylorus sparing (SIPS) surgery for morbid obesity: retrospective analyses of our preliminary experience. Obes Surg. 2016;26(9):2098–104.
Sánchez-Pernaute A, Rubio MA, Pérez-Aguirre E, et al. Single-anastomosis duodenoileal bypass with sleeve gastrectomy: metabolic improvement and weight loss in first 100 patients. Surg Obes Relat Dis. 2013;9:731–5.
Neichoy BT, Schniederjan B, Cottam DR, et al. Stomach intestinal pylorus-sparing surgery for morbid obesity. JSLS. 2018;22(1):e2017.00063.
Moon RC, Kirkpatrick V, Gaskins L, et al. Safety and effectiveness of single- versus double-anastomosis duodenal switch at a single institution. Surg Obes Relat Dis. 2019;15(2):245–52.
Nelson L, Moon RC, Teixeira AF, et al. Safety and effectiveness of single anastomosis duodenal switch procedure: preliminary results from a single institution. Arq Bras Cir Dig. 2016;29(Suppl 1):80–4.
Enochs P, Bull J, Surve A, et al. Comparative analysis of the single-anastomosis duodenal-ileal bypass with sleeve gastrectomy (SADI-S) to established bariatric procedures: an assessment of 2-year postoperative data illustrating weight loss, type 2 diabetes, and nutritional status in a single US center. Surg Obes Relat Dis. 2020;16(1):24–33. https://doi.org/10.1016/j.soard.2019.10.008.
Surve A, Rao R, Cottam D, et al. Early outcomes of primary SADI-S: an Australian experience. Obes Surg. 2020;30:1429–36. https://doi.org/10.1007/s11695-019-04312-6.
Brown WA, Ooi G, Higa K, et al. Single anastomosis duodenal-ileal bypass with sleeve gastrectomy/one anastomosis duodenal switch (SADI-S/OADS) IFSO position statement. Obes Surg. 2018;28(5):1207–16. https://doi.org/10.1007/s11695-018-3201-4.
Kallies K, Rogers AM, American Society for Metabolic and Bariatric Surgery Clinical Issues Committee. American Society for Metabolic and Bariatric Surgery updated statement on single-anastomosis duodenal switch. Surg Obes Relat Dis. 2020;16(7):825–30. https://doi.org/10.1016/j.soard.2020.03.020.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13. https://doi.org/10.1097/01.sla.0000133083.54934.ae.
Li RA, Liu L, Arterburn D, et al. Five-year longitudinal cohort study of reinterventions after sleeve gastrectomy and Roux-en-Y gastric bypass [published online ahead of print, 2019 Jun 7]. Ann Surg. 2019. https://doi.org/10.1097/SLA.0000000000003401, https://doi.org/10.1097/SLA.0000000000003401.
Higa K, Ho T, Tercero F, et al. Laparoscopic Roux-en-Y gastric bypass: 10-year follow-up. Surg Obes Relat Dis. 2011;7(4):516–25. https://doi.org/10.1016/j.soard.2010.10.019.
Kothari SN, Borgert AJ, Kallies KJ, et al. Long-term (>10-year) outcomes after laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2017;13(6):972–8. https://doi.org/10.1016/j.soard.2016.12.011.
Sugerman HJ, Wolfe LG, Sica DA, et al. Diabetes and hypertension in severe obesity and effects of gastric bypass-induced weight loss. Ann Surg. 2003;237(6):751–8. https://doi.org/10.1097/01.SLA.0000071560.76194.11.
Obeid NR, Malick W, Concors SJ, et al. Long-term outcomes after Roux-en-Y gastric bypass: 10- to 13-year data. Surg Obes Relat Dis. 2016;12(1):11–20. https://doi.org/10.1016/j.soard.2015.04.011.
Angrisani L, Cutolo PP, Formisano G, et al. Laparoscopic adjustable gastric banding versus Roux-en-Y gastric bypass: 10-year results of a prospective, randomized trial. Surg Obes Relat Dis. 2013;9(3):405–13. https://doi.org/10.1016/j.soard.2012.11.011.
O'Brien PE, Hindle A, Brennan L, et al. Long-term outcomes after bariatric surgery: a systematic review and meta-analysis of weight loss at 10 or more years for all bariatric procedures and a single-centre review of 20-year outcomes after adjustable gastric banding. Obes Surg. 2019;29(1):3–14. https://doi.org/10.1007/s11695-018-3525-0.
Nergaard BJ, Leifsson BG, Hedenbro J, et al. Gastric bypass with long alimentary limb or long pancreato-biliary limb--long-term results on weight loss, resolution of co-morbidities and metabolic parameters. Obes Surg. 2014;24(10):1595–602. https://doi.org/10.1007/s11695-014-1245-7.
Christou NV, Look D, Maclean LD. Weight gain after short- and long-limb gastric bypass in patients followed for longer than 10 years. Ann Surg. 2006;244(5):734–40. https://doi.org/10.1097/01.sla.0000217592.04061.d5.
Edholm D, Svensson F, Näslund I, et al. Long-term results 11 years after primary gastric bypass in 384 patients. Surg Obes Relat Dis. 2013;9(5):708–13. https://doi.org/10.1016/j.soard.2012.02.011.
Suter M, Donadini A, Romy S, et al. Laparoscopic Roux-en-Y gastric bypass: significant long-term weight loss, improvement of obesity-related comorbidities and quality of life. Ann Surg. 2011;254(2):267–73. https://doi.org/10.1097/SLA.0b013e3182263b66.
Park JY, Song D, Kim YJ. Causes and outcomes of revisional bariatric surgery: initial experience at a single center. Ann Surg Treat Res. 2014;86(6):295–301. https://doi.org/10.4174/astr.2014.86.6.295.
Behrns K, Smith C, Kelly K, et al. Reoperative bariatric surgery—lessons learned to improve patient selection and results. Ann Surg. 1993;218:646–53.
Author information
Authors and Affiliations
Contributions
Amit Surve: conceived and designed the analysis, collected the data, performed the analysis, and wrote and revised the manuscript.
Daniel Cottam: primary operating surgery and reviewed the manuscript.
Christina Richards: primary or assisting surgeon.
Walter Medlin: assisting surgeon.
Legrand Belnap: assisting surgeon.
Corresponding author
Ethics declarations
Conflict of Interest
Daniel Cottam, the corresponding author of this report, is part of the speaker bureau for Medtronic and has been awarded a research grant by Medtronic for the study of duodenal switch and reports personal fees and other from Medtronic and GI Windows, outside the submitted work. All other authors have no conflicts of interest to declare.
Ethical Approval
For this type of study, formal consent is not required.
Informed Consent
Does not apply.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Surve, A., Cottam, D., Richards, C. et al. A Matched Cohort Comparison of Long-term Outcomes of Roux-en-Y Gastric Bypass (RYGB) Versus Single-Anastomosis Duodeno-ileostomy with Sleeve Gastrectomy (SADI-S). OBES SURG 31, 1438–1448 (2021). https://doi.org/10.1007/s11695-020-05131-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-05131-w