Abstract
Introduction
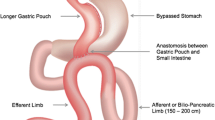
There is significant variation in practices concerning Roux-en-Y gastric bypass (RYGB) among bariatric surgeons, but there is currently a lack of robust data on the nature and extent of these variations. The purpose of this study was to understand global variations in practices concerning RYGB.
Methods
A questionnaire-based survey on Survey Monkey® was created, and the link was shared freely on various social media platforms. The link was also distributed through a personnel email network of authors.
Results
A total of 657 surgeons from 65 countries completed the survey. Crohn’s disease and liver cirrhosis were considered absolute contraindications for RYGB by 427 surgeons (64.98%) and 347 surgeons (53.30%), respectively. More than 68.5% of surgeons performed routine upper GI endoscopy while 64.17% performed routine ultrasound of abdomen preoperatively. The majority of surgeons (77.70%) used the perigastric technique for Gastric pouch creation. Approximately, 79.5% used orogastric bougie. More than 70% of the respondents did not use any staple line reinforcement routinely. Only 17.67% of surgeons measured the whole small bowel length, and the majority of surgeons (86.5%) used constant length of BP limb. Approximately, 89% used constant length of alimentary limb. Approximately, 95% of surgeons preferred antecolic bypass, and more than 86% routinely closed the Petersen defect. Marginal ulcer prophylaxis was used by the majority (91.17%). Almost 95% of surgeons recommended lifelong vitamin and mineral supplements.
Conclusion
This survey identifies global variations in practices concerning RYGB. It identifies several areas for future research and consensus building.






Similar content being viewed by others
References
Angrisani L, Santonicola A, Iovino P, et al. IFSO worldwide survey 2016: primary, endoluminal, and revisional procedures. Obes Surg. 2018;28(12):3783–94.
Griffen Jr WO, Young VL, Stevenson CC. A prospective comparison of gastric and jejunoileal bypass procedures for morbid obesity. Ann Surg. 1977;186(4):500–9.
Mahawar KK, Kumar P, Parmar C, et al. Small bowel limb lengths and Roux-en-Y gastric bypass: a systematic review. Obes Surg. 2016;26(3):660–71.
Mahawar K, Sharples AJ, Graham Y. A systematic review of the effect of gastric pouch and/or gastrojejunostomy (stoma) size on weight loss outcomes with Roux-en-Y gastric bypass. Surg Endosc. 2020;34(3):1048–60.
Madan AK, Harper JL, Tichansky DS. Techniques of laparoscopic gastric bypass: on-line survey of American Society for Bariatric Surgery practicing surgeons. Surg Obes Relat Dis. 2008;4(2):166–73.
Mahawar KK, Kular KS, Parmar C, et al. Perioperative practices concerning one anastomosis (mini) gastric bypass: a survey of 210 surgeons. Obes Surg. 2018;28(1):204–11.
Adil MT, Aminian A, Bhasker AG, et al. Perioperative practices concerning sleeve gastrectomy—a survey of 863 surgeons with a cumulative experience of 520,230 procedures. Obes Surg. 2020;30(2):483–92.
Mahawar KK, Nimeri A, Adamo M, et al. Practices concerning revisional bariatric surgery: a survey of 460 surgeons. Obes Surg. 2018;28(9):2650–60.
Mahawar KK, Himpens J, Shikora SA, et al. The first consensus statement on one anastomosis/mini gastric bypass (OAGB/MGB) using a modified Delphi approach. Obes Surg. 2018;28(2):303–12.
Gagner M, Hutchinson C, Rosenthal R. Fifth International Consensus Conference: current status of sleeve gastrectomy. Surg Obes Relat Dis. 2016;12(4):750–6.
Mahawar KK, Himpens JM, Shikora SA, et al. The first consensus statement on revisional bariatric surgery using a modified Delphi approach [published online ahead of print, 2019 Jun 19]. Surg Endosc. 2019; https://doi.org/10.1007/s00464-019-06937-1.
Singh S, Dulai PS, Zarrinpar A, et al. Obesity in IBD: epidemiology, pathogenesis, disease course and treatment outcomes. Nat Rev Gastroenterol Hepatol. 2017;14(2):110–21.
SAGES Guidelines Committee. SAGES guideline for clinical application of laparoscopic bariatric surgery. Surg Obes Relat Dis. 2009;5(3):387–405. https://doi.org/10.1016/j.soard.2009.01.010
Hudson JL, Barnes EL, Herfarth HH, et al. Bariatric surgery is a safe and effective option for patients with inflammatory bowel diseases: a case series and systematic review of the literature. Inflamm Intest Dis. 2019;3(4):173–9.
Zeni TM, Frantzides CT, Mahr C, et al. Value of preoperative upper endoscopy in patients undergoing laparoscopic gastric bypass. Obes Surg. 2006;16(2):142–6.
Schirmer B, Erenoglu C, Miller A. Flexible endoscopy in the management of patients undergoing Roux-en-Y gastric bypass. Obes Surg. 2002;12(5):634–8.
Azagury D, Dumonceau JM, Morel P, et al. Preoperative work-up in asymptomatic patients undergoing Roux-en-Y gastric bypass: is endoscopy mandatory? Obes Surg. 2006;16(10):1304–11.
Sakorafas GH, Milingos D, Peros G. Asymptomatic cholelithiasis: is cholecystectomy really needed? A critical reappraisal 15 years after the introduction of laparoscopic cholecystectomy. Dig Dis Sci. 2007;52(5):1313–25.
Attili AF, Carulli N, Roda E, et al. Epidemiology of gallstone disease in Italy: prevalence data of the Multicenter Italian Study on Cholelithiasis (M.I.COL.). Am J Epidemiol. 1995;141(2):158–65.
Muhrbeck O, Ahlberg J. Prevalence of gallstone disease in a Swedish population. Scand J Gastroenterol. 1995;30(11):1125–8.
Beckingham IJ. ABC of diseases of liver, pancreas, and biliary system. Gallstone disease. BMJ. 2001;322(7278):91–4.
Iglezias Brandao de Oliveira C, Adami Chaim E, da Silva BB. Impact of rapid weight reduction on risk of cholelithiasis after bariatric surgery. Obes Surg. 2003;13(4):625–8.
Amaral JF, Thompson WR. Gallbladder disease in the morbidly obese. Am J Surg. 1985;149(4):551–7.
Warschkow R, Tarantino I, Ukegjini K, et al. Concomitant cholecystectomy during laparoscopic Roux-en-Y gastric bypass in obese patients is not justified: a meta-analysis. Obes Surg. 2013;23(3):397–407.
Worni M, Guller U, Shah A, et al. Cholecystectomy concomitant with laparoscopic gastric bypass: a trend analysis of the nationwide inpatient sample from 2001 to 2008. Obes Surg. 2012;22(2):220–9.
Stokes CS, Gluud LL, Casper M, et al. Ursodeoxycholic acid and diets higher in fat prevent gallbladder stones during weight loss: a meta-analysis of randomized controlled trials. Clin Gastroenterol Hepatol. 2014;12(7):1090–100.e2. quiz e61
Uy MC, Talingdan-Te MC, Espinosa WZ, et al. Ursodeoxycholic acid in the prevention of gallstone formation after bariatric surgery: a meta-analysis. Obes Surg. 2008;18(12):1532–8.
Boerlage TCC, Haal S, Maurits de Brauw L, et al. Ursodeoxycholic acid for the prevention of symptomatic gallstone disease after bariatric surgery: study protocol for a randomized controlled trial (UPGRADE trial). BMC Gastroenterol. 2017;17(1):164.
Edholm D, Ottosson J, Sundbom M. Importance of pouch size in laparoscopic Roux-en-Y gastric bypass: a cohort study of 14,168 patients. Surg Endosc. 2016;30(5):2011–5.
Mahawar K, Sharples AJ, Graham Y. A systematic review of the effect of gastric pouch and/or gastrojejunostomy (stoma) size on weight loss outcomes with Roux-en-Y gastric bypass. Surg Endosc 2019.
Flanagan L. Measurement of functional pouch volume following the gastric bypass procedure. Obes Surg. 1996;6(1):38–43.
Roberts K, Duffy A, Kaufman J, et al. Size matters: gastric pouch size correlates with weight loss after laparoscopic Roux-en-Y gastric bypass. Surg Endosc. 2007;21(8):1397–402.
Topart P, Becouarn G, Ritz P. Pouch size after gastric bypass does not correlate with weight loss outcome. Obes Surg. 2011;21(9):1350–4.
Madan AK, Tichansky DS, Phillips JC. Does pouch size matter? Obes Surg. 2007;17(3):317–20.
Podnos YD, Jimenez JC, Wilson SE, et al. Complications after laparoscopic gastric bypass: a review of 3464 cases. Arch Surg. 2003;138(9):957–61.
Gonzalez R, Sarr MG, Smith CD, et al. Diagnosis and contemporary management of anastomotic leaks after gastric bypass for obesity. J Am Coll Surg. 2007;204(1):47–55.
Biertho L, Steffen R, Ricklin T, et al. Laparoscopic gastric bypass versus laparoscopic adjustable gastric banding: a comparative study of 1,200 cases. J Am Coll Surg. 2003;197(4):536–44. discussion 44-5
DeMaria EJ, Sugerman HJ, Kellum JM, et al. Results of 281 consecutive total laparoscopic Roux-en-Y gastric bypasses to treat morbid obesity. Ann Surg. 2002;235(5):640–5. discussion 5-7
Fernandez Jr AZ, DeMaria EJ, Tichansky DS, et al. Experience with over 3,000 open and laparoscopic bariatric procedures: multivariate analysis of factors related to leak and resultant mortality. Surg Endosc. 2004;18(2):193–7.
Higa KD, Ho T, Boone KB. Laparoscopic Roux-en-Y gastric bypass: technique and 3-year follow-up. J Laparoendosc Adv Surg Tech A. 2001;11(6):377–82.
Nguyen NT, Goldman C, Rosenquist CJ, et al. Laparoscopic versus open gastric bypass: a randomized study of outcomes, quality of life, and costs. Ann Surg. 2001;234(3):279–89. discussion 89-91
Papasavas PK, Hayetian FD, Caushaj PF, et al. Outcome analysis of laparoscopic Roux-en-Y gastric bypass for morbid obesity. The first 116 cases. Surg Endosc. 2002;16(12):1653–7.
Schauer PR, Ikramuddin S, Gourash W, et al. Outcomes after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Ann Surg. 2000;232(4):515–29.
Wittgrove AC, Clark GW. Laparoscopic gastric bypass, Roux-en-Y- 500 patients: technique and results, with 3-60 month follow-up. Obes Surg. 2000;10(3):233–9.
Baker RS, Foote J, Kemmeter P, et al. The science of stapling and leaks. Obes Surg. 2004;14(10):1290–8.
Sajid MS, Khatri K, Singh K, et al. Use of staple-line reinforcement in laparoscopic gastric bypass surgery: a meta-analysis. Surg Endosc. 2011;25(9):2884–91.
Yolsuriyanwong K, Ingviya T, Kongkamol C, et al. Effects of intraoperative leak testing on postoperative leak-related outcomes after primary bariatric surgery: an analysis of the MBSAQIP database. Surg Obes Relat Dis. 2019;15(9):1530–40.
Kolakowski Jr S, Kirkland ML, Schuricht AL. Routine postoperative upper gastrointestinal series after Roux-en-Y gastric bypass: determination of whether it is necessary. Arch Surg. 2007;142(10):930–4. discussion 4
Lee SD, Khouzam MN, Kellum JM, et al. Selective, versus routine, upper gastrointestinal series leads to equal morbidity and reduced hospital stay in laparoscopic gastric bypass patients. Surg Obes Relat Dis. 2007;3(4):413–6.
Doraiswamy A, Rasmussen JJ, Pierce J, et al. The utility of routine postoperative upper GI series following laparoscopic gastric bypass. Surg Endosc. 2007;21(12):2159–62.
Carter JT, Tafreshian S, Campos GM, et al. Routine upper GI series after gastric bypass does not reliably identify anastomotic leaks or predict stricture formation. Surg Endosc. 2007;21(12):2172–7.
Quartararo G, Facchiano E, Scaringi S, et al. Upper gastrointestinal series after Roux-en-Y gastric bypass for morbid obesity: effectiveness in leakage detection. A systematic review of the literature. Obes Surg. 2014;24(7):1096–101.
Singh R, Fisher BL. Sensitivity and specificity of postoperative upper GI series following gastric bypass. Obes Surg. 2003;13(1):73–5.
Leslie DB, Dorman RB, Anderson J, et al. Routine upper gastrointestinal imaging is superior to clinical signs for detecting gastrojejunal leak after laparoscopic Roux-en-Y gastric bypass. J Am Coll Surg. 2012;214(2):208–13.
Kim J, Azagury D, Eisenberg D, et al. ASMBS position statement on prevention, detection, and treatment of gastrointestinal leak after gastric bypass and sleeve gastrectomy, including the roles of imaging, surgical exploration, and nonoperative management. Surg Obes Relat Dis. 2015;11(4):739–48.
Busetto L, Dicker D, Azran C, et al. Obesity Management Task Force of the European Association for the Study of Obesity released “Practical Recommendations for the Post-Bariatric Surgery Medical Management”. Obes Surg. 2018;28(7):2117–21.
Mechanick JI, Apovian C, Brethauer S, et al. Clinical practice guidelines for the perioperative nutrition, metabolic, and nonsurgical support of patients undergoing bariatric procedures—2019 update: cosponsored by American Association of Clinical Endocrinologists/American College of Endocrinology, The Obesity Society, American Society for Metabolic & Bariatric Surgery, Obesity Medicine Association, and American Society of Anesthesiologists—executive summary. Endocr Pract. 2019;25(12):1346–59.
Ruiz-Tovar J, Vorwald P, Gonzalez-Ramirez G, et al. Impact of biliopancreatic limb length (70 cm vs 120 cm), with constant 150 cm alimentary limb, on long-term weight loss, remission of comorbidities and supplementation needs after Roux-en-Y gastric bypass: a prospective randomized clinical trial. Obes Surg. 2019;29(8):2367–72.
Shah K, Nergard BJ, Fagerland MW, et al. Distal gastric bypass: 2-m biliopancreatic limb construction with varying lengths of common channel. Surg Obes Relat Dis. 2019;15(9):1520–6.
Author information
Authors and Affiliations
Contributions
All authors have seen and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
Informed consent does not apply.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Kumar, P., Yau, HC.V., Trivedi, A. et al. Global Variations in Practices Concerning Roux-en-Y Gastric Bypass—an Online Survey of 651 Bariatric and Metabolic Surgeons with Cumulative Experience of 158,335 Procedures. OBES SURG 30, 4339–4351 (2020). https://doi.org/10.1007/s11695-020-04796-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-04796-7