Abstract
Purpose
Upper airway stimulation (UAS) is an innovative treatment for patients with obstructive sleep apnea (OSA). UAS titrations are performed 3 months after activation of the device to optimize its effectiveness. In general, these titrations are performed during an in-laboratory overnight polysomnography (PSG). However, overnight titrations are expensive and can be logistically challenging because they are labor-intensive which causes shortage of sleep technicians available for night shifts. In addition, recently, overnight PSGs were postponed and canceled due to the COVID-19 pandemic. We aimed to assess the feasibility of a daytime PSG to perform titration of UAS therapy as an alternative for a conventional overnight PSG.
Methods
We performed a prospective single-center observational cohort study. Patients were included when planned for UAS titration; this was approximately 6 months after UAS activation. Data on sleep architecture, patient experience, and respiratory outcomes were collected to evaluate the feasibility. An overnight follow-up PSG 12 months after implantation was used to compare sleep architecture and therapy response.
Results
Of 23 patients, four were excluded from analysis because of technical issues during PSG. Even though patients slept significantly shorter during the daytime PSG, this was enough time to complete the titration successfully with 30-min sleep in final therapeutic settings in 84% of the patients. Patients (94%) had a positive experience with the daytime titration. Respiratory outcomes were significantly reduced during titration and were maintained at the 12-month follow-up.
Conclusion
Daytime titrations are a valuable alternative for conventional overnight titrations. Our findings suggest the implementation of daytime titrations as standard of care. This will contribute to easier logistics and better work circumstances for sleep technicians without jeopardizing titration quality.
Similar content being viewed by others
Introduction
Continuous positive airway pressure (CPAP) is the gold standard therapy for patients with moderate to severe obstructive sleep apnea (OSA), proven to be highly effective in reducing complaints and comorbidities [1,2,3]. Despite its high efficacy, many patients are unable to tolerate treatment with CPAP.
An alternative treatment for a specific group of patients is hypoglossal nerve stimulation (HNS; Inspire® Medical Systems, Inc.), also referred to as upper airway stimulation (UAS). The protrusion fibers of the hypoglossal are stimulated by using unilateral simulation, mainly innervating tongue protrusion. The neurostimulator delivers electrical stimulating pulses to the hypoglossal nerve through the stimulation lead; the stimulating pulses are synchronized with ventilation detected by the sensing lead. This ensures the patency of the upper airway. UAS therapy has demonstrated a significant improvement in OSA outcomes, good therapy adherence, and high patient satisfaction [4, 5].
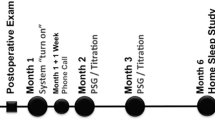
Patients are eligible for UAS device implantation when strict selection criteria are met [6]. In general, 4 to 6 weeks after implantation the UAS device is activated with standard settings. The device will be slowly up-titrated at home until patient’s symptoms such as decreased sleep quality, daytime sleepiness, and snoring have improved. An in-lab overnight titration polysomnography (PSG) is subsequently performed once patients are accustomed to the stimulation and subjective symptoms have improved. The main purpose of the titration is to establish a comfortable but effective device setting to maintain upper airway patency during sleep. This titration is performed by a trained sleep technician. During this titration, the UAS device settings are optimized and titrated until respiratory events are normalized. Electrode configuration, stimulation amplitude, and stimulation pulse width and rate can be adjusted. The final settings should minimize the occurrence of obstructive events and should not cause arousals [7].
Traditionally titrations were performed in-lab and overnight which is logistically challenging and expensive. They are mainly labor-intensive because sleep technicians have to be available during the night. Another havoc presented itself during the COVID-19 pandemic. Sleep laboratories were often imposed to resign overnight hospital beds due to shortages. As a result, overnight sleep studies were often postponed resulting in long waiting lists. Also the growing amount of patients with UAS device asks for a more accessible way to perform titrations.
An alternative for an overnight titration is a daytime titration. Several studies have investigated the role of a daytime PSG in diagnosing OSA, concluding that a daytime PSG is a viable and effective alternative [8,9,10]. Other studies have investigated the role of a daytime PSG in CPAP titrations, concluding that a daytime PSG is a useful tool for CPAP titration [11,12,13,14]. To date, the role of a daytime PSG in UAS titration has not yet been investigated.
A daytime PSG might be a valuable alternative for an overnight PSG to perform titration in the context of UAS optimization. The benefit of a daytime PSG for titration is that sleep technicians do not have to work during the night and sleep studies will not have to be postponed due to bed and staff shortage. The aim of this study is to assess the feasibility of a daytime PSG to perform titration of UAS therapy in patients with OSA. Effect on sleep architecture, titration success and practicality, and patients’ experience with daytime titration was evaluated. Secondarily, respiratory outcomes from UAS therapy during titration were evaluated and compared to the outcomes after 12 months of therapy use.
Materials and methods
Study participants
We performed a prospective single-center observational cohort study including OSA patients with UAS therapy. Yearly about 35 patients with severe OSA receive UAS implantation at the Department of Otorhinolaryngology/Head and Neck Surgery in OLVG Hospital, Amsterdam, the Netherlands [15]. Patients were included from September 2019 to January 2021 if they were scheduled for a standard in-lab PSG for titration which was approximately 3 months after device activation. They were included if they were 18 years or older and were able to speak, read, and write in Dutch. Instead of the standard overnight in-lab PSG, a daytime in-lab PSG was used to perform titration.
Patients were admitted the night prior to their daytime titration PSG and were instructed not to sleep. The following morning the patients were asked to document caffeine, nicotine, or alcohol consumption during the night. Other questions included their experience with UAS and sleep quality during the past months at home. The UAS device system was checked and subsequently all components were applied to perform the PSG. At 08:00 a.m., patients were asked to go to sleep. Patients slept in a soundproof room with no daylight. The PSG was observed by a sleep technician, who at the same time performed the titration. The sleep technician checked if all sleep stages were reached while the optimization process took place.
Sleep architecture data from the daytime titration was compared to the 12-month PSG (which is standard of care) after implantation. The latter was performed either at home or in-lab with the device switched on.
Effectiveness of UAS was investigated comparing respiratory outcomes between the pre-operative PSG and the 12-month PSG, as described above. The therapeutic AHI achieved during the daytime titration was also compared to the AHI measured during the 12-month follow-up PSG.
Patient experience with the daytime titration was asked during a follow-up appointment a week after titration.
Ethical considerations
This study was conducted with approval of the local advisory committee for scientific research of the OLVG Hospital, Amsterdam, the Netherlands. To protect personal information, all data of participants were collected and stored encoded. All participants signed an informed consent.
Polysomnography
A standard polysomnography (SOMNOscreenTM, SOMNOmedics GmbH, Randersacker, Germany) was performed in all patients. To determine the stages of sleep, an electroencephalogram (F3, F4, C3, C4, M1, M2, O1, O2), electro-oculogram, and electromyogram of the submental muscle were obtained. Nasal airflow was measured by a nasal cannula/pressure transducer inserted in the opening of the nostrils. An oronasal thermal flow sensor was used to determine the difference between the temperatures of exhaled and ambient air to estimate airflow and detect mouth breathing. Arterial blood oxyhemoglobin was recorded with the use of a finger pulse oximeter. Thoracoabdominal excursions were measured qualitatively by respiratory effort belts placed over the rib cage and abdomen. Body position was determined by a position sensor, which differentiates between the upright, left side, right side, prone, and supine position. Limb movements were detected with an anterior tibial electromyogram with surface electrodes. Electrocardiography was performed to score cardiac events and snore sensor was applied for occurrence of snoring.
Scoring
The sleep stages were scored manually by an experienced sleep investigator in 30-s epochs according to the American Academy of Sleep Medicine (AASM, scoring manual version 2.6, 2020) scoring manual, with N3 representing slow wave sleep. Both daytime PSG and follow-up PSG were scored by the same sleep technician and neurosomnologist, and the scoring was not blinded.
Titration
The main purpose of titration was to optimize the UAS device settings until respiratory events were eliminated or reduced to a clinically satisfactory level. The sleep technician paid attention to several titration parameters such as amplitude, polarity, and stimulation duration. The sleep technician started the UAS therapy once the patient was in consolidated sleep and the individual start delay of the UAS device had expired. The stimulation level started with 0.2-V amplitude below the functional threshold and was therefore unlikely to provoke an arousal. The stimulation setting was increased with 0.1-V or 0.2-V amplitude when four or more serial obstructive events or loud ambiguous snoring occurred. The patient was observed in all non-rapid eye movement (NREM) sleep stages and REM sleep, preferably containing REM sleep in supine position, for optimal titration settings. The titration was finished when the patient had slept for 30 min straight with the final settings, ideally with an apnea–hypopnea index (AHI) < 5. Preferably this 30 min contained rapid eye movement (REM) sleep and sleep in supine position. When this was not achieved, the sleep technician ended the titration when the patient had slept through at least 2 full sleep cycles. The calculated AHI was the AHI with optimal therapeutic settings.
Statistical analysis
Statistical analysis was performed using SPSS (version 24, SPSS Inc., Chicago, IL). Quantitative data are reported as mean and standard deviation (SD) or as median and Q1–Q3 when not normally distributed. Qualitative variables are reported as frequencies and percentages. The Shapiro–Wilk test was used to determine whether the continuous variables were normally distributed. When the Statistic W was > 0.90, the data was considered normally distributed. Baseline characteristics and PSG parameters were analyzed by using descriptive statistics. A p value of < 0.05 was considered to prove statistical significance.
Results
Baseline characteristics
Of 23 patients receiving UAS implantation, four patients were excluded due to technical problems during the daytime PSG. Two patients had technical interruptions because of software failure; therefore, it was not possible to register sufficient continuous sleep. The other two patients had connection problems with the implanted pulse generator (IPG) and therefore awakened frequently, giving unreliable results. Excluded patients are shown in Appendix Table 5.
In total, 19 patients were included for statistical analysis. Thus far, fourteen completed their 12-month follow-up overnight PSG. The majority of the patients was male (84%); at the time of titration, the mean age was 57 ± 11 years with a mean BMI of 27.2 ± 2.4 kg/m2. Based on baseline PSG data, the mean pre-operative AHI was 41.2 ± 10.8 events per hour. The baseline patient characteristics are shown in Table 1. The median time between device activation and titration was 6 months and the median device usage was 48 [42.0; 54.0] h a week before titration.
Effect on sleep architecture
A comparison of daytime PSG to overnight PSG sleep architecture is shown in Table 2. Patients slept 3.4 ± 1.0 h during the daytime PSG; this was significantly shorter than during overnight PSG (6.8 ± 1.0 h) (p < 0.001). Sleep efficiency was comparable: 80.3% [65.7; 90.4] during daytime and 85.2% [84.0; 90.8] during overnight PSG (p = 0.177). Sleep latency was significantly shorter during the daytime PSG (3.0 [1.1; 10.0] min) than during overnight PSG (7.6 [5.8; 17.0] min). No significant differences were found regarding sleep stages N2 and N3 (p = 0.107, p = 0.103). During the daytime PSG, significantly more N1 sleep was found (7.8 [6.1; 13.2] % of TST) than during the overnight PSG (4.5 [2.2; 5.0] % of TST) (p = 0.003). Significantly less REM sleep occurred during the daytime PSG (12.9 ± 8.1% of TST) than during overnight PSG (24.7 ± 7.7% of TST) (p = 0.007). Two patients did not have any REM sleep during the daytime PSG. The median amount of sleep cycles during the daytime PSG was three complete cycles compared to the overnight PSG with a median of four complete cycles.
Success and practicality of daytime titration
The outcomes of the (pre-) daytime titration in terms of feasibility are shown in Table 3. The majority of patients was able to stay awake after midnight until the start of the daytime PSG. In total, two patients slept after midnight with a maximum of 150 min. Eighty-four percent of the patients were able to sleep 30 min in the final UAS device settings. Device polarity settings or amplitude voltage were changed in 47.4% of the patients following the titration. The exact changes in setting and stimulation amplitude in voltage for every patient are presented in Appendix Table 6.
Subjective patient experience
Almost all patients (94%) had a positive experience with the daytime titration; one patient experienced discomfort from the titration (Fig. 1). The majority of patients (88.2%) did not suffer from tiredness 3 days after titration and could pick up their normal sleeping habits without any problems. Four patients (24%) took a daytime nap the day after titration.
Titration and follow-up outcome
The median AHI decreased significantly (p = 0.001) from baseline with 40.4 [34.6; 46.9] events per hour to 9.0 [3.3; 17.0] events per hour during titration. At the 12-month follow-up, the AHI was 12.2 [6.7; 24.9] events per hour, not significantly different from the titration AHI (p = 0.158). There was also a statistically significant reduction of AI, RDI, ODI, arousal index, lowest saturation, and time slept with SpO2 < 90%, as shown in Table 4. The ODI (3% and 4%) during titration was not significantly different from the follow-up ODI (respectively p = 0.272 and p = 0.875). Time slept in supine position did not differ significantly between baseline, titration, and follow-up.
Discussion
This single-center prospective study is the first study to demonstrate that a daytime PSG to perform titration is a feasible alternative for a conventional overnight titration for OSA patients with UAS therapy. Even though patients slept significantly shorter during the daytime PSG, this was enough time to complete the titration successfully with 30-min sleep in final therapeutic settings in 84% of the patients. Furthermore, 94% of the patients had a positive experience with the daytime titration and did not experience any discomfort. Respiratory OSA outcomes were significantly reduced during titration and were maintained at the 12-month follow-up.
To the best of our knowledge, no other study has investigated the role of daytime PSG for titration of UAS. A few studies have already proven that daytime PSG is an appropriate procedure for titration of CPAP [8, 11, 12, 14, 16]. The American Academy of Sleep Medicine (AASM) clinical practice guideline states that a CPAP titration should be carried out for at least 3 h during NREM and REM sleep in supine position. [17] This is comparable to our study where patients averagely slept 3.4 ± 1.0 h while all sleep stages were observed including REM in supine position in final settings in 31.6% of the patients.
To ensure patients were able to sleep during the daytime PSG, they were asked to stay awake the night before the titration. A concern might be that overnight sleep deprivation in OSA patients alters sleep architecture and AHI results. For example, Persson and Svanborg observed an increase of AHI in OSA patients after sleep deprivation, suggesting that daytime studies are not suitable to determine the severity of OSA [18]. In our study, however, the daytime PSG was used to titrate the UAS therapy. Our results show that there are no significant differences between the AHI at the 12-month follow-up (12.0 [6.7; 24.9]) and the titration AHI (9.0 [3.3; 17.0]) (p = 0.158). This means that the optimal settings found during titration were effective even with a possible altered AHI at the time of titration. On the other hand, a significantly shorter period of REM sleep was found during the daytime PSG of 12.9 ± 8.1 compared to 24.7 ± 7.7 overnight PSG (% of TST) (p = 0.007). Since it is known that during REM sleep oxygen desaturation is more severe than during NREM sleep in patients with OSA, this could have underestimated the OSA severity during titration [19]. Again our results at the 12-month follow-up showed no significant difference and therefore, this argument had no influence on our titration. Also, the supine body position often increases the severity of apneas during therapy. Our study did not correct for the effect of body position during the daytime PSG. However, no significant differences were found for % TST in supine position between baseline, titration, and follow-up PSG.
This study in not without limitations. Yearly approximately 35 patients with OSA are recruited for UAS therapy in the OLVG Hospital and we were able to include 23 patients in this study [15]. The small sample size and the 5 patients who did not yet complete their 12-month follow-up should be taken into consideration when interpreting the results. Some differences might be significant when larger studies are performed. Ideally we would have compared the daytime titration PSG to an overnight titration PSG. Unfortunately, this was not feasible during this pilot study. Due to the fact that during the pre-op PSG patients are suffering from untreated OSA, we opted to compare both sleep architecture and respiratory outcomes with the 12-month follow-up PSG. Furthermore, we did not prohibit patients to consume caffeine the night before the daytime PSG. This might have influenced the sleep architecture but due to the group size (3 patients who consumed caffeine) we were not able to prove significant differences.
Our experience with activation and titration has developed over the past few years. We know now it pays off to be flexible and to take more time to adjust and find a therapeutic but comfortable setting for patients. Whenever patients report subjective improvements during the first few months, this implies good therapy response. The titration could then be postponed or in the future even be replaced by a PSG at home to confirm therapy response. In this study, device settings changed based on titration outcomes in 47.4% of the patients, suggesting that in all other cases the optimal settings were already found previously. Potentially this would obviate the need for titration in certain patients. A recent study by Steffen et al. assessed the use of home sleep tests for the treatment-adjustment phase of UAS. They concluded that home sleep tests had clinical advantages and were useful as a second-line titration control method under several conditions [20]. In addition, in a recently published case study, Huyett and Stagnone described the use of pulse oximetry as an addition to home titration for UAS therapy optimization before actual in-lab titration. They also concluded that certain patients could possibly directly proceed to a home sleep test instead of in-lab PSG titration [21].
When comparing sleep architecture, sleep efficiency was similar for the daytime PSG compared to the overnight follow-up PSG (p = 0.177). These results are comparable with Miyata et al. who also found no significant difference for sleep efficiency when comparing a daytime PSG with an overnight PSG for diagnosing OSA [10]. Sleep latency was significantly shorter during the daytime PSG, with 3.0 [1.1; 10.0] min compared to 7.6 [5.8; 17.0] min overnight. The overnight sleep latency is comparable with a normal sleep latency for healthy people between 50 and 64 years [22]. Sleep deprivation the night before titration might explain the shorter sleep latency during the daytime PSG [23]. No significant difference was found for N2 and N3 sleep during the daytime PSG compared to the follow-up overnight PSG. The amount of N2 and N3 sleep found in this study is similar to the study of Boulos et al. who investigated sleep architecture in healthy people between 50 and 64 years. The independent effect of OSA on sleep architecture remains unclear. Shahveisi et al. found that OSA independently has the tendency to increase N1 sleep [24]. This perhaps could explain the significant difference we found in the amount of N1 sleep during the daytime PSG (7.8 [6.1; 13.2] % of TST) compared to the overnight PSG (4.5 [2.2; 5.0] % of TST) (p = 0.003). Titration was performed during the daytime PSG meaning that therapy was not consistent resulting in occasional OSA compared to the follow-up overnight PSG where therapy was used the entire night.
We found similar results regarding respiratory outcomes with UAS therapy during titration and 12-month follow-up compared to similar larger studies. First, the results of the recently published ADHERE study show a median AHI reduction from 32.8 [23.6; 45.0] events per hour at baseline to 9.5 [4.0; 18.5] events per hour after 12 months [25]. These are similar to our results: a reduction in AHI from 40.4 [34.6; 46.9] events per hour at baseline to 12.2 [6.7; 24.9] events per hour after 12 months. In the original STAR trial, the AHI decreased from 28.2 events per hour at baseline to 8.7 events per hour at 12 months [26]. Furthermore, device usage in our study (48 [42; 54] h per week) was comparable to a similar study (47.0 [38.5; 52.0] h per week after 6 months). [20].
The growing amount of patients using UAS therapy asks for a more accessible way to perform titrations. Performing these titrations during the night makes it very labor-intensive and expensive. The technician is subsequently not available for the day shift and many sleep technicians dislike night shifts because of understandable personal circumstances. The benefit of a daytime PSG is that more titrations can be performed and sleep technicians do not have to work during the night. The implications of performing daytime PSG for titration include being able to perform more titrations with shorter waiting time and less labor-intensive work for sleep technicians. Patients experienced this daytime study as positive and were willing to repeat it in the future if necessary.
Daytime titrations are a valuable alternative for conventional overnight titrations. Our findings suggest the implementation of daytime titrations as standard of care. This will contribute to easier logistics and better work circumstances for sleep technicians without jeopardizing titration quality.
Availability of data and material
The data that support the finding of this study are available upon reasonable request.
Code availability
Not applicable.
Abbreviations
- AASM:
-
American Academy of Sleep Medicine
- AI:
-
Apnea-index
- AHI:
-
Apnea-hypopnea index
- BMI:
-
Body mass index
- CPAP:
-
Continues positive airway pressure
- DPSG:
-
Daytime polysomnography
- FU-NPSG:
-
Follow-up overnight polysomnography
- HNS:
-
Hypoglossal nerve stimulation
- IPG:
-
Implanted pulse generator
- NREM:
-
Non-rapid eye movement
- ODI:
-
Oxygen desaturation
- OSA:
-
Obstructive sleep apnea
- PSG:
-
Polysomnography
- RDI:
-
Respiratory disturbance index
- REM:
-
Rapid eye movement
- SpO2 :
-
Peripheral capillary oxygen saturation
- TST:
-
Total sleep time
- UAS:
-
Upper airway stimulation
References
Antic NA et al (2011) The effect of CPAP in normalizing daytime sleepiness, quality of life, and neurocognitive function in patients with moderate to severe OSA. Sleep 34(1):111–119
Buchner NJ et al (2007) Continuous positive airway pressure treatment of mild to moderate obstructive sleep apnea reduces cardiovascular risk. Am J Respir Crit Care Med 176(12):1274–1280
Giles TL, Lasserson TJ, Smith BH, White J, Wright J, Cates CJ (2006) Continuous positive airways pressure for obstructive sleep apnoea in adults. Cochrane Database Syst Rev. 19;(3):CD001106. https://doi.org/10.1002/14651858.CD001106.pub3
Strollo PJ Jr et al (2014) Upper-airway stimulation for obstructive sleep apnea. N Engl J Med 370(2):139–149
Boon M et al (2018) Upper airway stimulation for obstructive sleep apnea: results from the ADHERE Registry. Otolaryngol Head Neck Surg 159(2):379–385
Vonk PE, Benoist LBL, Kasius KM, van Maanen JP, Ravesloot MJL, Reesink HJ, de Vries N (2019) Stimulatie van tongzenuw bij obstructieve slaapapneu [Hypoglossal nerve stimulation for obstructive sleep apnoea; technique, indication and future prospects]. Ned Tijdschr Geneeskd. 3;163:D3286. https://pubmed.ncbi.nlm.nih.gov/31120206/
Vanderveken OM et al (2017) Development of a clinical pathway and technical aspects of upper airway stimulation therapy for obstructive sleep apnea. Front Neurosci 11:523
Mahakit P (2012) A comparative study of two-hour daytime and overnight polysomnography in high risk snorers. J Med Assoc Thai 95(Suppl 5):S17-22
Yakar F et al (2015) Role of daytime polysomnography in the diagnosis of sleep apnea syndrome. Tuberk Toraks 63(2):78–85
Miyata S et al (2007) Daytime polysomnography for early diagnosis and treatment of patients with suspected sleep-disordered breathing. Sleep Breath 11(2):109–115
Rudkowski JC, Verschelden P, Kimoff RJ (2001) Efficacy of daytime continuous positive airway pressure titration in severe obstructive sleep apnoea. Eur Respir J 18(3):535–541
Rosenthal L et al (1998) Daytime CPAP titration: a viable alternative for patients with severe obstructive sleep apnea. Chest 114(4):1056–1060
Al-Jawder S, Bahammam A (2009) Utility of daytime polysomnography for in-patients with suspected sleep-disordered breathing. Neurol Neurochir Pol 43(2):140–147
Lloberes P et al (2004) Comparison of conventional nighttime with automatic or manual daytime CPAP titration in unselected sleep apnea patients: study of the usefulness of daytime titration studies. Respir Med 98(7):619–625
Vonk PE et al (2020) Short-term results of upper airway stimulation in obstructive sleep apnoea patients: the Amsterdam experience. J Laryngol Otol 134(5):447–452
Hoekema A et al (2006) Nap-titration: an effective alternative for continuous positive airway pressure titration. Respir Med 100(4):705–713
Kushida CA et al (2008) Clinical guidelines for the manual titration of positive airway pressure in patients with obstructive sleep apnea. J Clin Sleep Med 4(2):157–171
Persson HE, Svanborg E (1996) Sleep deprivation worsens obstructive sleep apnea. Comparison between diurnal and nocturnal polysomnography. Chest 109(3):645–50
Sampol G et al (1996) Nasal continuous positive airway pressure with supplemental oxygen in coexistent sleep apnoea-hypopnoea syndrome and severe chronic obstructive pulmonary disease. Eur Respir J 9(1):111–116
Steffen A, König IR, Baptista PM, Abrams N, Jeschke S, Hasselbacher K (2020) Home Sleep Testing to Direct Upper Airway Stimulation Therapy Optimization for Sleep Apnea. Laryngoscope.131(4):E1375–E1379. https://pubmed.ncbi.nlm.nih.gov/32865831
Huyett P, Stagnone R (2020) Use of overnight pulse oximetry and a type 3 sleep study to titrate hypoglossal nerve stimulation therapy. J Clin Sleep Med 16(12):2109–2111
Boulos MI et al (2019) Normal polysomnography parameters in healthy adults: a systematic review and meta-analysis. Lancet Respir Med 7(6):533–543
Borbély AA et al (1981) Sleep deprivation: effect on sleep stages and EEG power density in man. Electroencephalogr Clin Neurophysiol 51(5):483–495
Shahveisi K et al (2018) Sleep architecture in patients with primary snoring and obstructive sleep apnea. Basic Clin Neurosci 9(2):147–156
Thaler E et al (2020) Results of the ADHERE upper airway stimulation registry and predictors of therapy efficacy. Laryngoscope 130(5):1333–1338
Woodson BT et al (2016) Three-year outcomes of cranial nerve stimulation for obstructive sleep apnea: the STAR trial. Otolaryngol Head Neck Surg 154(1):181–188
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (name of institute/committee) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was submitted to the local advisory board of scientific research (ACWO) and approved by the board of directors (IRB) of OLVG Hospital.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Bosschieter, P.F.N., Schoustra, E., de Vries, N. et al. Daytime polysomnography to perform titration for upper airway stimulation in patients with obstructive sleep apnea. Sleep Breath 26, 707–715 (2022). https://doi.org/10.1007/s11325-021-02441-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-021-02441-w