Abstract
Purpose
This study aims to evaluate if gender influences the sleep duration perception in adults referred for polysomnography (PSG).
Methods
A cross-sectional study was undertaken from December 2019 to January 2021. Total sleep time was objectively assessed from the overnight PSG and subjectively estimated. The sleep perception index (SPI) was defined by the ratio of subjective and objective values. Diagnosis of obstructive sleep apnea (OSA) was based on an apnea–hypopnea index ≥ 5.0/h. Insomnia was defined by the presence of one or more specific complaints: difficulty falling asleep, difficulty maintaining sleep, and/or waking up earlier than desired. The association between continuous variables and SPI was assessed by linear regression analysis.
Results
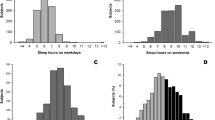
This study enrolled 2,004 outpatients (56% men) who were grouped into four subsamples: controls (n = 139), insomnia (n = 154), OSA (n = 912), and insomnia comorbid with OSA [COMISA] (n = 799). In women, the median SPI differed among groups and ranged from 89 to 102% (p = 0.001); while in men, it ranged from 90% to 99% (p = 0.007). However, no gender-related SPI value differences emerged within each of the subgroups: controls (p = 0.907), insomnia (p = 0.830), OSA (p = 0.070), and COMISA (p = 0.547). The presence of insomnia (β, − 0.101, p < 0.001) or OSA (β, − 0.082, p = 0.001), but not gender (β, − 0.017, p = 0.612), were independent predictors of the SPI.
Conclusion
In a clinical referral cohort, no evidence of sex dimorphism emerged for SPI irrespective of the underlying sleep diagnosis.


Similar content being viewed by others
Data availability
Not applicable.
References
Benjafield AV, Ayas NT, Eastwood PR, Heinzer R, Ip MSM, Morrell MJ, Nunez CM, Patel SR, Penzel T, Pépin JL, Peppard PE, Sinha S, Tufik S, Valentine K, Malhotra A (2019) Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med 7(8):687–698
Patel SR (2019) Obstructive sleep apnea. Ann Intern Med 171(11):ITC81–ITC96
Zhang Y, Ren R, Lei F, Zhou J, Zhang J, Wing YK, Sanford LD, Tang X (2019) Worldwide and regional prevalence rates of co-occurrence of insomnia and insomnia symptoms with obstructive sleep apnea: a systematic review and meta-analysis. Sleep Med Rev 45:1–17
Sateia MJ (2014) International classification of sleep disorders-third edition: highlights and modifications. Chest 146(5):1387–1394
Taylor DJ, Mallory LJ, Lichstein KL, Durrence HH, Riedel BW, Bush AJ (2007) Comorbidity of chronic insomnia with medical problems. Sleep 30(2):213–218
Li M, Zhang XW, Hou WS, Tang ZY (2014) Insomnia and risk of cardiovascular disease: a meta-analysis of cohort studies. Int J Cardiol 176(3):1044–1047
Sweetman AM, Lack LC, Catcheside PG, Antic NA, Chai-Coetzer CL, Smith SS, Douglas JA, McEvoy RD (2017) Developing a successful treatment for co-morbid insomnia and sleep apnoea. Sleep Med Rev 33:28–38
Daley M, Morin CM, LeBlanc M, Grégoire JP, Savard J (2009) The economic burden of insomnia: direct and indirect costs for individuals with insomnia syndrome, insomnia symptoms, and good sleepers. Sleep 32(1):55–64
Schiza SE, Bouloukaki I (2020) Does gender matter: sex-specific aspects of symptoms, outcome, and therapy of obstructive sleep apnea. Curr Opin Pulm Med 26(6):642–649
Zhang Z, Cheng J, Yang W, Zou H, Su C, Miao J (2020) Gender differences in clinical manifestations and polysomnographic findings in Chinese patients with obstructive sleep apnea. Sleep Breath 24(3):1019–1026
Basoglu OK, Tasbakan MS (2018) Gender differences in clinical and polysomnographic features of obstructive sleep apnea: a clinical study of 2827 patients. Sleep Breath 22(1):241–249
Van Eycken S, Neu D, Newell J, Kornreich C, Mairesse O (2020) Sex-related differences in sleep-related PSG parameters and daytime complaints in a clinical population. Nat Sci Sleep 12:161–171
Erdemir Işık M, Gülbay B, Çiftci F, Acıcan T (2020) Polysomnographic, demographic and clinic differences between male and female obstructive sleep apnea patients. Tuberk Toraks 68(4):361–370
Bouloukaki I, Mermigkis C, Markakis M, Pataka A, Alexaki I, Ermidou C, Moniaki V, Mauroudi E, Michelakis S, Schiza SE (2019) Cardiovascular effect and symptom profile of obstructive sleep apnea: does sex matter? J Clin Sleep Med 15(12):1737–1745
Zeng LN, Zong QQ, Yang Y, Zhang L, Xiang YF, Ng CH, Chen LG, Xiang YT (2020) Gender difference in the prevalence of insomnia: a meta-analysis of observational studies. Front Psychiatry 11:577429
Chen LJ, Steptoe A, Chen YH, Ku PW, Lin CH (2017) Physical activity, smoking, and the incidence of clinically diagnosed insomnia. Sleep Med 30:189–194
Lallukka T, Sares-Jäske L, Kronholm E, Sääksjärvi K, Lundqvist A, Partonen T, Rahkonen O, Knekt P (2012) Sociodemographic and socioeconomic differences in sleep duration and insomnia-related symptoms in Finnish adults. BMC Public Health 12:565
Angst J, Gamma A, Gastpar M, Lépine JP, Mendlewicz J, Tylee A, Depression Research in European Society Study (2002) Gender differences in depression. Epidemiological findings from the European DEPRES I and II studies. Eur Arch Psychiatry Clin Neurosci 252(5):201–209
Asher M, Aderka IM (2018) Gender differences in social anxiety disorder. J Clin Psychol 74(10):1730–1741
Bianchi MT, Williams KL, McKinney S, Ellenbogen JM (2013) The subjective-objective mismatch in sleep perception among those with insomnia and sleep apnea. J Sleep Res 22(5):557–568
Choi SJ, Suh S, Ong J, Joo EY (2016) Sleep misperception in chronic insomnia patients with obstructive sleep apnea syndrome: implications for clinical assessment. J Clin Sleep Med 12(11):1517–1525
Schinkelshoek MS, de Wit K, Bruggink V, Fronczek R, Lammers GJ (2020) Daytime sleep state misperception in a tertiary sleep centre population. Sleep Med 69:78–84
Pinto LR Jr, Pinto MC, Goulart LI, Truksinas E, Rossi MV, Morin CM, Tufik S (2009) Sleep perception in insomniacs, sleep-disordered breathing patients, and healthy volunteers–an important biologic parameter of sleep. Sleep Med 10(8):865–868
Trimmel K, Eder HG, Böck M, Stefanic-Kejik A, Klösch G, Seidel S (2021) The (mis)perception of sleep: factors influencing the discrepancy between self-reported and objective sleep parameters. J Clin Sleep Med 2021 Jan 4. https://doi.org/10.5664/jcsm.9086
Duarte RLM, Mendes BA, Oliveira-E-Sá TS, Magalhães-da-Silveira FJ, Gozal D (2020) Perception of sleep duration in adult patients with suspected obstructive sleep apnea. PLoS One 15(8):e0238083
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14(6):540–545
Berry RB, Budhiraja R, Gottlieb DJ, Gozal D, Iber C, Kapur VK, Marcus CL, Mehra R, Parthasarathy S, Quan SF, Redline S, Strohl KP, Davidson Ward SL, Tangredi MM, American Academy of Sleep Medicine (2012) Rules for scoring respiratory events in sleep: update of the 2007 AASM manual for the scoring of sleep and associated events. Deliberations of the sleep apnea definitions task force of the American academy of sleep medicine. J Clin Sleep Med 8(5):597–619
Edinger JD, Fins AI (1995) The distribution and clinical significance of sleep time misperceptions among insomniacs. Sleep 18(4):232–239
Voderholzer U, Al-Shajlawi A, Weske G, Feige B, Riemann D (2003) Are there gender differences in objective and subjective sleep measures? A study of insomniacs and healthy controls. Depress Anxiety 17(3):162–172
Kalak N, Brand S, Beck J, Holsboer-Trachsler E, Wollmer MA (2015) Association between subjective actual sleep duration, subjective sleep need, age, body mass index, and gender in a large sample of young adults. Neuropsychiatr Dis Treat 11:107–113
Author information
Authors and Affiliations
Contributions
Study design, RLMD; data collection, RLMD; data analysis, RLMD; study supervision, FJMS and DG; manuscript writing, RLMD; and critical revisions for important intellectual content, FJMS and DG. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was previously approved by the Research Ethics Committee of the Federal University of Rio de Janeiro. Informed consent was obtained from all individuals included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Duarte, R.L.M., Magalhães-da-Silveira, F.J. & Gozal, D. Gender-related sleep duration perception in a Brazilian sleep clinic cohort. Sleep Breath 26, 641–647 (2022). https://doi.org/10.1007/s11325-021-02438-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-021-02438-5