Abstract
Purpose
Drug-induced sleep endoscopy (DISE) has been poorly explored as an examination to assess positive airway pressure (PAP) therapy in patients with obstructive sleep apnea (OSA). The present study aimed to identify by DISE possible characteristics related to low compliance with PAP therapy due to respiratory complaints.
Methods
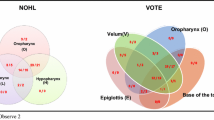
Patients using PAP for OSA underwent DISE in two conditions: (1) baseline (without PAP) and (2) PAP (with the same mask and airway pressure used at home). We compared patients reporting low compliance to PAP due to respiratory complaints to those well-adapted to therapy. VOTE classification (assessment of velopharynx, oropharynx, tongue base, and epiglottis) and TOTAL VOTE score (the sum of VOTE scores at each anatomical site) were assessed. ROC curve analyzed the accuracy of TOTAL VOTE to predict low compliance due to persistent pharyngeal obstruction in both conditions.
Results
Of 19 patients enrolled, all presented multilevel pharyngeal obstruction at baseline condition, with no difference between groups at this study point. When PAP was added, the median VOTE value was higher in the epiglottis (P value=0.02) and tended to be higher at the velum and tongue base in the poorly adapted group; TOTAL VOTE score was also significantly increased in patients with low compliance (P value<0.001). ROC curve demonstrated that patients with TOTAL VOTE scored 2.5 or more during DISE with PAP presented a 4.6-fold higher risk for low compliance with PAP therapy due to pharyngeal obstruction (AUC: 0.88±0.07; P value<0.01; sensitivity: 77%; specificity: 83%).
Conclusions
Adding PAP during a DISE examination may help to predict persistent pharyngeal obstruction during PAP therapy.






Similar content being viewed by others
References
Kushida CA, Littner MR, Hirshkowitz M, Morgenthaler TI, Alessi CA, Bailey D, Boehlecke B, Brown TM, Coleman J Jr, Friedman L, Kapen S, Kapur VK, Kramer M, Lee-Chiong T, Owens J, Pancer JP, Swick TJ, Wise MS, American Academy of Sleep Medicine (2006) Practice parameters for the use of continuous and bilevel positive airway pressure devices to treat adult patients with sleep-related breathing disorders. Sleep 29(3):375–380. https://doi.org/10.1093/sleep/29.3.375
Kushida CA, Nichols DA, Holmes TH, Quan SF, Walsh JK, Gottlieb DJ, Simon RD Jr, Guilleminault C, White DP, Goodwin JL, Schweitzer PK, Leary EB, Hyde PR, Hirshkowitz M, Green S, McEvoy LK, Chan C, Gevins A, Kay GG, Bloch DA, Crabtree T, Dement WC (2012) Effects of continuous positive airway pressure on neurocognitive function in obstructive sleep apnea patients: the apnea positive pressure long-term efficacy study (APPLES). Sleep 35(12):1593–1602. https://doi.org/10.5665/sleep.2226
Queiroz DL, Yui MS, Braga AA et al (2014) Adherence of obstructive sleep apnea syndrome patients to continuous positive airway pressure in a public service. Braz J Otorhinolaryngol 80(2):126–130. https://doi.org/10.5935/1808-8694.20140027
Avellan-Hietanen H, Brander P, Bachour A (2019) Symptoms during CPAP therapy are the major reason for contacting the sleep unit between two routine contacts. J Clin Sleep Med 15(1):47–53. https://doi.org/10.5664/jcsm.7568
Borel JC, Tamisier R, Dias-Domingos S, Sapene M, Martin F, Stach B, Grillet Y, Muir JF, Levy P, Series F, Pepin JL, on behalf of the Scientific Council of The Sleep Registry of the French Federation of Pneumology (OSFP) (2013) Type of mask may impact on continuous positive airway pressure adherence in apneic patients. PLoS One 8(5):e64382. https://doi.org/10.1371/journal.pone.0064382
Vroegop AV, Vanderveken OM, Boudewyns AN, Scholman J, Saldien V, Wouters K, Braem MJ, van de Heyning PH, Hamans E (2014) Drug-induced sleep endoscopy in sleep-disordered breathing: report on 1,249 cases. Laryngoscope 124(3):797–802. https://doi.org/10.1002/lary.24479
Vanderveken OM, Maurer JT, Hohenhorst W, Hamans E, Lin HS, Vroegop AV, Anders C, de Vries N, van de Heyning PH (2013) Evaluation of drug-induced sleep endoscopy as a patient selection tool for implanted upper airway stimulation for obstructive sleep apnea. J Clin Sleep Med 9(5):433–438. https://doi.org/10.5664/jcsm.2658
Kezirian EJ (2011) Nonresponders to pharyngeal surgery for obstructive sleep apnea: insights from drug-induced sleep endoscopy. Laryngoscope 121(6):1320–1326. https://doi.org/10.1002/lary.21749
Eichler C, Sommer JU, Stuck BA, Hörmann K, Maurer JT (2013) Does drug-induced sleep endoscopy change the treatment concept of patients with snoring and obstructive sleep apnea? Sleep Breath 17(1):63–68. https://doi.org/10.1007/s11325-012-0647-9
Vroegop AV, Vanderveken OM, Dieltjens M et al (2013) Sleep endoscopy with simulation bite for prediction of oral appliance treatment outcome. J Sleep Res 22(3):348–355. https://doi.org/10.1111/jsr.12008
De Vito A, Carrasco Llatas M, Ravesloot MJ et al (2018) European position paper on drug-induced sleep endoscopy: 2017 update. Clin Otolaryngol 43(6):1541–1552. https://doi.org/10.1111/coa.13213
Rabelo FA, Küpper DS, Sander HH, Fernandes RM, Valera FC (2013) Polysomnographic evaluation of propofol-induced sleep in patients with respiratory sleep disorders and controls. Laryngoscope 123(9):2300–2305. https://doi.org/10.1002/lary.23664
Kezirian EJ, Hohenhorst W, de Vries N (2011) Drug-induced sleep endoscopy: the VOTE classification. Eur Arch Otorhinolaryngol 268(8):1233–1236. https://doi.org/10.1007/s00405-011-1633-8
Yui MS, Tominaga Q, Lopes BCP, Eckeli AL, Rabelo FAW, Küpper DS, Valera FCP (2020) Nasal vs. oronasal mask during PAP treatment: a comparative DISE study. Sleep Breath 24(3):1129–1136. https://doi.org/10.1007/s11325-019-01976-3
Shimohata T, Tomita M, Nakayama H, Aizawa N, Ozawa T, Nishizawa M (2011) Floppy epiglottis as a contraindication of CPAP in patients with multiple system atrophy. Neurology 76(21):1841–1842. https://doi.org/10.1212/WNL.0b013e31821ccd07
Hybášková J, Jor O, Novák V, Zeleník K, Matoušek P, Komínek P (2016) Drug-induced sleep endoscopy changes the treatment concept in patients with obstructive sleep apnoea. Biomed Res Int 2016:6583216–6583215. https://doi.org/10.1155/2016/6583216
Freiser ME, Schell AE, Soose RJ (2020) DISE-PAP: a method for troubleshooting residual AHI elevation despite positive pressure therapy. J Clin Sleep Med 16(4):631–633. https://doi.org/10.5664/jcsm.8240
Kastoer C, Benoist LBL, Dieltjens M, Torensma B, de Vries LH, Vonk PE, Ravesloot MJL, de Vries N (2018) Comparison of upper airway collapse patterns and its clinical significance: drug-induced sleep endoscopy in patients without obstructive sleep apnea, positional and non-positional obstructive sleep apnea. Sleep Breath 22(4):939–948. https://doi.org/10.1007/s11325-018-1702-y
Andersen AP, Alving J, Lildholdt T, Wulff CH (1987) Obstructive sleep apnea initiated by a lax epiglottis. A contraindication for continuous positive airway pressure. Chest 91(4):621–623. https://doi.org/10.1378/chest.91.4.621
Verse T, Pirsig W (1999) Age-related changes in the epiglottis causing failure of nasal continuous positive airway pressure therapy. J Laryngol Otol 113(11):1022–1025. https://doi.org/10.1017/s0022215100145888
Schorr F, Genta PR, Gregório MG, Danzi-Soares NJ, Lorenzi-Filho G (2012) Continuous positive airway pressure delivered by oronasal mask may not be effective for obstructive sleep apnoea. Eur Respir J 40(2):503–505. https://doi.org/10.1183/09031936.00145111
De Beer D, Chambers N (2003) Double trouble: prolapsing epiglottis and unexpected dual pathology in an infant. Paediatr Anaesth 13(5):448–452. https://doi.org/10.1046/j.1460-9592.2003.00980.x
Torre C, Camacho M, Liu SY, Huon LK, Capasso R (2016) Epiglottis collapse in adult obstructive sleep apnea: a systematic review. Laryngoscope 126(2):515–523. https://doi.org/10.1002/lary.25589
Kastoer C, Op de Beeck S, Dom M et al (2020) Drug-induced sleep endoscopy upper airway collapse patterns and maxillomandibular advancement. Laryngoscope 130(4):E268–E274. https://doi.org/10.1002/lary.28022
Torre C, Liu SY, Kushida CA, Nekhendzy V, Huon LK, Capasso R (2017) Impact of continuous positive airway pressure in patients with obstructive sleep apnea during drug-induced sleep endoscopy. Clin Otolaryngol 42(6):1218–1223. https://doi.org/10.1111/coa.12851
Schwab RJ, Pack AI, Gupta KB, Metzger LJ, Oh E, Getsy JE, Hoffman EA, Gefter WB (1996) Upper airway and soft tissue structural changes induced by CPAP in normal subjects. Am J Respir Crit Care Med 154(4 Pt 1):1106–1116. https://doi.org/10.1164/ajrccm.154.4.888761
Andrade RG, Piccin VS, Nascimento JA, Viana FM, Genta PR, Lorenzi-Filho G (2014) Impact of the type of mask on the effectiveness of and adherence to continuous positive airway pressure treatment for obstructive sleep apnea. J Bras Pneumol 40(6):658–668. https://doi.org/10.1590/S1806-37132014000600010
Acknowledgements
This clinical trial has been registered at http://www.ensaiosclinicos.gov.br/rg/RBR-9wdkjh under the number RBR-9wdkjh
This study has been funded by FAPESP—São Paulo Research Foundation (grant number 2012/10006-3, specific for the study), CNPq (grant scholarship to FCPV), and CAPES (grant scholarship to MSY).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yui, M.S., Tominaga, Q., Lopes, B.C.P. et al. Can drug-induced sleep endoscopy (DISE) predict compliance with positive airway pressure therapy? A pilot study. Sleep Breath 26, 109–116 (2022). https://doi.org/10.1007/s11325-021-02360-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-021-02360-w