Abstract
Purpose
Insufficient sleep is not well studied in developing countries. We assessed sleep duration among adults in Lebanon and examined its potential predictors and relationship with subjective sleep insufficiency, daytime fatigue, and weekday sleep debt.
Methods
This cross-sectional study included 501 adults (mean age 45.2 (SD15.2) years, 64% females) from the community in Beirut and Mount Lebanon. Socio-demographic, lifestyle and health characteristics, subjective sleep insufficiency, daytime fatigue, and weekday sleep debt (weekend vs. weekdays sleep duration) were compared between individuals who reported sleeping < 6:00, 6–7:59(reference), or ≥ 8:00 h/night. Symptoms and predictors of sleep duration were assessed using logistic regression.
Results
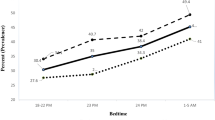
Thirty-nine percent of participants reported sleeping < 6 h/night while 15% reported sleeping ≥ 8:00 h/night. Age (OR = 1.16/year, 95% CI [1.02–1.33]) and female sex (OR = 1.71, 95% CI [1.14–2.58]) were significant predictors of short sleep (< 6:00 h/night) in multivariable adjusted analyses. Compared to referent (6:00–7:59 h/night) and long sleepers (≥ 8:00 h/night), short sleepers were significantly more likely to report subjective sleep insufficiency (OR = 3.00, 95% CI [2:00–4.48], and OR = 4.52, 95% CI [2.41–8.51]; respectively) and daytime fatigue (OR = 1.53, 95% CI [1.04–2.24], and OR = 1.83, 95% CI [1.06–2.04]; respectively). Compared to long weekdays sleepers, short and referent weekdays sleepers were more likely to sleep longer on weekend (OR = 2.47, 95% CI [1.18–5.15], and OR = 4.16, 95% CI [2.03–8.5]; respectively).
Conclusions
Short sleep is highly prevalent in this urban cohort from a low- to medium-income country especially among women and older adults, and is associated with subjective sleep insufficiency, daytime fatigue, and weekday sleep debt. The socio-cultural determinants of sleep duration need to be studied across different populations to better evaluate the causes and implications of short sleep.
Similar content being viewed by others
References
Jackson CL, Redline S, Emmons KM (2015) Sleep as a potential fundamental contributor to disparities in cardiovascular health. Annu Rev Public Health 36:417–440 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4736723/
Knutson KL (2010) Sleep duration and cardiometabolic risk: a review of the epidemiologic evidence. Best Pract Res Clin Endocrinol Metab 24:731–743 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3011978/
Grandner MA, Patel NP, Gehrman PR, Perlis ML, Pack AI (2010) Problems associated with short sleep: bridging the gap between laboratory and epidemiological studies. Sleep Med Rev 14:239–247
Leproult R, Deliens G, Gilson M, Peigneux P (2015) Beneficial impact of sleep extension on fasting insulin sensitivity in adults with habitual sleep restriction. Sleep 38:707–715 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4402666/
Haack M, Serrador J, Cohen D, Simpson N, Meier-Ewert H, Mullington JM (2013) Increasing sleep duration to lower beat-to-beat blood pressure: a pilot study. J Sleep Res 22:295–304 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3582793/
Holliday EG, Magee CA, Kritharides L, Banks E, Attia J (2013) Short sleep duration is associated with risk of future diabetes but not cardiovascular disease: a prospective study and meta-analysis. PLoS One 8:e82305 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3840027/
Hale L, Do DP (2007) Racial differences in self-reports of sleep duration in a population-based study. Sleep 30:1096–1103 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1978399/
Grandner MA, Williams NJ, Knutson KL, Roberts D, Jean-Louis G (2016) Sleep disparity, race/ethnicity, and socioeconomic position. Sleep Med 18:7–18 https://www.ncbi.nlm.nih.gov/pubmed/26431755
Groeger JA, Zijlstra F, Dijk DJ (2004) Sleep quantity, sleep difficulties and their perceived consequences in a representative sample of some 2000 British adults. J Sleep Res 13:359–371 https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1365-2869.2004.00418.x
Ursin R, Bjorvatn B, Holsten F (2005) Sleep duration, subjective sleep need, and sleep habits of 40-to 45-year-olds in the Hordaland Health Study. Sleep 28:1260–1269 https://pdfs.semanticscholar.org/1c2e/5f66b8efab48a71e9c5178fdb06d17025f37.pdf
Assaad S, Costanian C, Haddad G, Tannous F (2014) Sleep patterns and disorders among university students in Lebanon. J Res Health Sci 14:198–204 http://jrhs.umsha.ac.ir/index.php/JRHS/article/view/1485/html
Kabrita CS, Hajjar-Muça TA, Duffy JF (2014) Predictors of poor sleep quality among Lebanese university students: association between evening typology, lifestyle behaviors, and sleep habits. Nat Sci Sleep 6:11 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3894960/
Nasreddine L, Tamim H, Itani L, Nasrallah MP, Isma’eel H, Nakhoul NF, Abou-Rizk J, Naja F (2107) A minimally processed dietary pattern is associated with lower odds of metabolic syndrome among Lebanese adults. Public Health Nutr 21:160–171. https://doi.org/10.1017/S1368980017002130
Quan SF, Howard BV, Iber C, Kiley JP, Nieto FJ, O'Connor GT, Rapoport DM, Redline S, Robbins J, Samet JM, Wahl PW (1997) The sleep heart health study: design, rationale, and methods. Sleep 20:1077–1085 https://www.ncbi.nlm.nih.gov/pubmed/9493915
Saleh AB, Ahmad MA, Awadalla NJ (2011) Development of Arabic version of Berlin questionnaire to identify obstructive sleep apnea at risk patients. Ann Thorac Med 6:212–216 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3183638/
Gottlieb DJ, Punjabi NM, Newman AB, Resnick HE, Redline S, Baldwin CM, Nieto FJ (2005) Association of sleep time with diabetes mellitus and impaired glucose tolerance. Arch Intern Med 165:863–867 https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/486518
Arora T, Chen MZ, Cooper AR, Andrews RC, Taheri S (2016) The impact of sleep debt on excess adiposity and insulin sensitivity in patients with early type 2 diabetes mellitus. J Clin Sleep Med 12:673–680 https://europepmc.org/backend/ptpmcrender.fcgi?accid=PMC4865553&blobtype=pdf
Nasreddine L, Hwalla N, Sibai A, Hamzé M, Parent-Massin D (2002) Food consumption patterns in an adult urban population in Beirut, Lebanon. Toxicol Lett 127:29–41 https://www.cambridge.org/core/services/aop-cambridge-core/content/view/1515E29F50FD6C9D07AA4A8E96B54702/S1368980006000383a.pdf/food_consumption_patterns_in_an_adult_urban_population_in_beirut_lebanon.pdf
International Physical Activity Questionnaire (IPAQ). (2005) Guidelines for data processing and analysis of the international physical activity questionnaire (IPAQ) - short form. https://Users/ln10/Downloads/GuidelinesforDataProcessingandAnalysisoftheInternationalPhysicalActivityQuestionnaireIPAQShortandLongForms%20(1).pdf. Accessed 1 Dec 2018
Ikehara S, Iso H, Date C, Kikuchi S, Watanabe Y, Wada Y, Inaba Y, Tamakoshi A, JACC Study Group (2009) Association of sleep duration with mortality from cardiovascular disease and other causes for Japanese men and women: the JACC study. Sleep 32:295–230 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2647783/
Cai H, Shu X-O, Xiang Y-B, Yang G, Li H, Ji BT, Gao J, Gao YT, Zheng W (2015) Sleep duration and mortality: a prospective study of 113,138 middle-aged and elderly Chinese men and women. Sleep 38:529–536 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4355892/
Kim J-H, Kim KR, Cho KH et al (2013) The association between sleep duration and self-rated health in the Korean general population. J Clin Sleep Med 9:1057 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3778177/
Ahmed AE, Al-Jahdali F, AlALwan A et al (2017) Prevalence of sleep duration among Saudi adults. Saudi Med J 38:276. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5387904/–283
El Masri A, Kolt GS, Astell-Burt T et al (2017) Lifestyle behaviours of Lebanese-Australians: cross-sectional findings from the 45 and up study. PLoS One 12:e0181217 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5509310/
Karam EG, Mneimneh ZN, Dimassi H, Fayyad JA, Karam AN, Nasser SC, Chatterji S, Kessler RC (2008) Lifetime prevalence of mental disorders in Lebanon: first onset, treatment, and exposure to war. PLoS Med 5:e61 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2276523/
Chandola T, Ferrie JE, Perski A, Akbaraly T, Marmot MG (2010) The effect of short sleep duration on coronary heart disease risk is greatest among those with sleep disturbance: a prospective study from the Whitehall II cohort. Sleep 33:739–744 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2880242/
Nunes J, Jean-Louis G, Zizi F, Casimir GJ, von Gizycki H, Brown CD, McFarlane SI (2008) Sleep duration among black and white Americans: results of the National Health Interview Survey. J Natl Med Assoc 100:317–322 https://linkinghub.elsevier.com/retrieve/pii/S0027-9684(15)31244-X
Patel SR, Malhotra A, Gottlieb DJ, White DP, Hu FB (2006) Correlates of long sleep duration. Sleep 29:881–889 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3500381/
Grandner MA, Kripke DF, Naidoo N, Langer RD (2010) Relationships among dietary nutrients and subjective sleep, objective sleep, and napping in women. Sleep Med 11:180–184
Matthews KA, Patel SR, Pantesco EJ, Buysse DJ, Kamarck TW, Lee L, Hall MH (2018) Similarities and differences in estimates of sleep duration by polysomnography, actigraphy, diary, and self-reported habitual sleep in a community sample. Sleep Health 4:96–103 https://linkinghub.elsevier.com/retrieve/pii/S2352-7218(17)30224-3
Lockley SW, Skene DJ, Arendt J (1999) Comparison between subjective and actigraphic measurement of sleep and sleep rhythms. J Sleep Res 8:175–183 https://onlinelibrary.wiley.com/doi/epdf/10.1046/j.1365-2869.1999.00155.x
Patel SR, Ayas NT, Malhotra MR, White DP, Schernhammer ES, Speizer FE, Stampfer MJ, Hu FB (2004) A prospective study of sleep duration and mortality risk in women. Sleep 27:440–444 http://livebetterlife.net/wp-content/uploads/2013/09/270310.pdf
Tabar P. Immigration and Human Development: Evidence from Lebanon. United Nations Development Programme, Human Development Reports. Research Paper 2009/35. August 2009. https://mpra.ub.uni-muenchen.de/19219/1/MPRA_paper_19219.pdf. Accessed 1 Dec 2018
Le Borgne E, Jacobs TJ. (2016) Lebanon: Promoting Poverty Reduction and Shared Prosperity. World Bank Group. http://documents.worldbank.org/curated/en/951911467995104328/pdf/103201-REPLACEMNT-PUBLIC-Lebanon-SCD-Le-Borgne-and-Jacobs-2016.pdf. Accessed 1 Dec 2018
Acknowledgments
We acknowledge the contribution of the following volunteer students under the Medical Research Volunteer Program (MRVP) at the American University of Beirut: Michael Dagher, Abdulhamid Sabih, Lama Assi, Muhieddine Laban, Hisham Wehbe, Alaa Osta, Carine Baassiri, and Ali Jaber. Moreover, we would like to thank Juliana Breidy, Patricia Moghames, Joanna Bou Rizk, Christelle Cordahi, Zeinab Awada, Aya Noubani, Lara Itani, and Mohamad Medawar for their contribution in data collection.
Funding
This work was funded by the medical practice plan grants at the American University of Beirut and the Lebanese National Council for Scientific Research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chami, H.A., Ghandour, B., Isma’eel, H. et al. Sleepless in Beirut: sleep duration and associated subjective sleep insufficiency, daytime fatigue, and sleep debt in an urban environment. Sleep Breath 24, 357–367 (2020). https://doi.org/10.1007/s11325-019-01833-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-019-01833-3