Abstract
Anesthesia information management systems (AIMS) are sophisticated hardware and software technology solutions that can provide electronic feedback to anesthesia providers. This feedback can be tailored to provide clinical decision support (CDS) to aid clinicians with patient care processes, documentation compliance, and resource utilization. We conducted a systematic review of peer-reviewed articles on near real-time and point-of-care CDS within AIMS using the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols. Studies were identified by searches of the electronic databases Medline and EMBASE. Two reviewers screened studies based on title, abstract, and full text. Studies that were similar in intervention and desired outcome were grouped into CDS categories. Three reviewers graded the evidence within each category. The final analysis included 25 articles on CDS as implemented within AIMS. CDS categories included perioperative antibiotic prophylaxis, post-operative nausea and vomiting prophylaxis, vital sign monitors and alarms, glucose management, blood pressure management, ventilator management, clinical documentation, and resource utilization. Of these categories, the reviewers graded perioperative antibiotic prophylaxis and clinical documentation as having strong evidence per the peer reviewed literature. There is strong evidence for the inclusion of near real-time and point-of-care CDS in AIMS to enhance compliance with perioperative antibiotic prophylaxis and clinical documentation. Additional research is needed in many other areas of AIMS-based CDS.
Similar content being viewed by others
1 Introduction
Anesthesia information management systems (AIMS) originated in the 1980s as simple, computer-based intraoperative record keepers to complement or replace paper documentation of a patient’s anesthetic [1]. The core function of AIMS remains the generation of an automated electronic record of the patient’s physiological data that allows for manual notation of events such as medication administration [2]. AIMS have since evolved into sophisticated hardware and software systems that are either a stand-alone product or a module within a hospital’s electronic health record (EHR) system that shares the same underlying database as the EHR and is designed to present a specialty-specific view of the data relevant to perioperative requirements. Both types of AIMS offer features that enable anesthesia providers to record, view, and share patient information across the entire perioperative continuum [3].
AIMS have been shown to enhance the quality and safety of patient care, and clinical decision support (CDS) is one of the factors that has contributed to these benefits [4, 5]. CDS systems provide clinicians with patient-specific assessments or recommendations to assist with clinical decision-making [6]. CDS has become increasingly integrated into AIMS, and CDS can typically be categorized into one or more types: process of care (e.g. improving adherence to clinical protocols and guidelines) and administrative and resource management (e.g. documentation and billing) [7, 8].
Systematic reviews have shown how CDS that is embedded within hospitals’ EHRs can improve clinical performance, resource utilization and patient care [9, 10]. Most of the recent reviews on CDS and AIMS have been narrative rather than systematic in nature [11–14]. A recent comprehensive review of CDS in AIMS included non-AIMS CDS and did not mention search queries, systematic review guidelines, or articles published after 2014 [15, 16]. Thus, we used the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) [17, 18] to conduct a focused, up-to-date systematic review of peer-reviewed articles on near real-time and point-of-care CDS in AIMS.
2 Methods
2.1 Eligibility criteria
The selection criteria included studies of CDS specifically built within AIMS (not EHRs) that were published in English in peer-reviewed journals between January 1, 2000 and December 31, 2015. The interventions sought included any implementations of CDS resulting in an improvement in process of care or administrative and resource management. In the process of care category, the outcome measures sought included adherence to established clinical protocols and guidelines. In the category of administrative and resource management, the outcome measures sought included billing, medication and procedure documentation. Review articles and case reports were excluded from analysis.
2.2 Information sources
Studies were identified using searches of the electronic databases Medline and EMBASE.
2.3 Search strategy
One reviewer [AFS] and a Health Sciences Librarian [SEM] with expertise in systematic review searching created the Medline and EMBASE search queries listed in the “Appendix”.
The Medical Subject Heading (MeSH) terms used for the Medline search included the following: “integrated advanced information management systems”, “information management”, “hospital information systems”, “decision support systems, clinical”, electronic health records”, “decision support techniques”, “anesthesia”, and “medical record systems, computerized”. Non-MeSH keywords and phrases were combined with the MeSH terms, and included “anesthesia information management” as well as wildcard phrases such as “post-anesthes*” and “anesthes*”. Inclusion filters were applied for human subjects, the English language, presence of an abstract, and publication dates between January 1, 2000 and December 31, 2015. Exclusion filters included case reports and reviews.
The EMBASE search query consisted of the keywords “information system”, “information management”, “anesthesia information management system”, “electronic medical record”, “electronic health record”, “ehr”, “emr”, “decision support system” and “clinical decision support”. Inclusion filters were applied for the English language and publication dates between January 1, 2000 and December 31, 2015. An exclusion filter for Medline results was applied.
The Medline and EMBASE results were combined into a Microsoft Excel spreadsheet that included each study’s title, authors, date of publication, and journal information. Duplicates were removed. Two reviewers [AFS, JMT] screened the article titles for relevance to CDS in AIMS and used each article’s title to decide whether to accept, reject, or mark for further review. The two reviewers then screened the abstracts of all articles that were marked “accept” or “further review” in order to either accept or reject each remaining article. Another reviewer [AML] adjudicated any conflicts between the two reviewers. The full electronic versions of the articles marked “accept” were then obtained via institutional library access or by contacting the article’s contact author directly. The full articles were reviewed for inclusion of AIMS CDS with near-real-time alerts delivered to anesthesia providers at the point of care or via pagers or text messaging to supervising anesthesiologists; review articles, articles describing the use of checklists and other decision aids, and articles on utilizing AIMS data to drive post hoc emails and pages were removed at this step.
The data items extracted included the type of CDS alert, the behavior category, the message modality, and the outcome of the intervention. The measured outcomes in the reviewed studies included compliance rate with a care process or clinical protocol, vital sign monitoring and alert utilization rates, postoperative nausea and vomiting (PONV), and documentation completeness and compliance.
Because the study designs, interventions, and reported outcome measures varied significantly, we focused on qualitative synthesis rather than meta-analysis. If studies were sufficiently homogeneous in terms of intervention and desired outcome, then the studies were allocated into one group (e.g. perioperative antibiotic prophylaxis). Three reviewers [AFS, JMT, and AML] graded the studies using a scale based on the Grading of Recommendations Assessment, Development and Evaluation working group methodology [19]. For each category, the evidence was graded as “weak”, “moderate”, or “strong” based on the following: quality of evidence, study design (prospective versus retrospective), and number of participating study centers; majority vote determined the strength of the evidence.
3 Results
3.1 Study selection
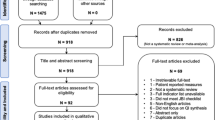
The analysis included 25 articles (Table 1). The Medline search query returned 847 articles and the EMBASE search query returned 162 articles for a combined total of 1009 articles in the initial sample; an additional article was identified while reviewing the Medline search results (Fig. 1). The review of article titles eliminated 944 articles, leaving 65 articles. During the review of article abstracts, 35 articles were removed, while 6 articles were eliminated after review of the full article text.
3.2 Perioperative antibiotic prophylaxis: initial dosing and re-dosing
Prophylactic antibiotic (PA) administration 1–2 h before surgical incision has been shown to reduce the risk of wound infection [20]. Five studies showed that CDS in AIMS was associated with significant improvements in the administration and/or re-dosing of perioperative antibiotic prophylaxis. Schwann et al. prospectively examined the effects of PA administration CDS point-of-care electronic prompts over 2 consecutive 6-month periods; the alerts increased PA administration compliance by 32 % and were associated with a 0.4 % absolute risk reduction in the incidence of surgical site infections (SSIs) [21]. Nair et al. showed that real-time CDS reminders improved PA rates to >99 % (compared to a baseline of 90 % with paper records) over a 6-month period [22]. Wax et al. described the impact of a visual interactive electronic CDS reminder on documented PA administration within 60 min before surgical procedure starting time (82.9 % during 8 months before CDS vs. 89.1 % during 10 months after CDS, p < 0.01) [23].
Antibiotics must be re-dosed at regular intervals during lengthy surgical cases in order to maintain efficacy [24]. St. Jacques et al. reported that the use of a basic AIMS reminder system increased the appropriate PA re-dosing rate from 20 to 58 % (p < 0.001) [25], while Nair et al. described similar PA re-dosing rates with basic AIMS reminders (62.5 ± 1.6 %) that were improved with real-time CDS (83.9 ± 3.4 %) (p < 0.001) [26].
Thus, there were five studies (most of which were prospective in design) from various settings that demonstrated strong evidence to support including AIMS CDS for PA administration and re-dosing in order to achieve significantly higher rates of PA compliance (three “strong” votes).
3.3 Postoperative nausea and vomiting prophylaxis
Postoperative nausea and vomiting (PONV) is one of the most common complaints following surgery and a considerable cause of dissatisfaction with recovery from anesthesia; thus, anesthesiologists will often administer prophylactic antiemetic medications to patients to reduce the likelihood of PONV [27]. Kappen et al. randomized anesthesiologists to exposure to a CDS tool—automated risk calculations for PONV—and found that the anesthesiologists exposed to the PONV prediction model administered more prophylactic antiemetic medications [rate ratio, 2.0; 95 % confidence interval (CI), 1.6–2.4]; however, a significant reduction in PONV incidence was not observed [28]. However, when the same group added a specific therapeutic recommendation (directive approach), the increase in PONV prophylaxis led to a reduction in PONV (odds ratio 0.60, 95 % CI 0.43–0.83), with an even greater reduction in PONV in high-risk patients (odds ratio 0.45, 95 % CI 0.28–0.72) [29]. In contrast, Kooij et al. implemented AIMS-based CDS reminders using a simplified PONV risk score that increased PONV guideline adherence from 38 % of high-risk patients to 73 % [30]; this change in practice was associated with a decrease in PONV from 32 to 23 % (p = 0.01) in a general surgical population [31]. The same group showed that withdrawal of the PONV CDS support resulted in a decrease in adherence to PONV prophylaxis recommendations 6 weeks after discontinuation of CDS (79 vs. 41 %, p < 0.001) [32].
There is moderate evidence to support a recommendation for PONV CDS in AIMS (two “moderate” votes, one “weak” vote). The available research is limited to two research groups, yet both groups showed a positive patient outcome (reduction in PONV) after implementation of PONV CDS.
3.4 Management of vital sign monitors and alarms
The American Society of Anesthesiology has set standards and guidelines for monitoring vital signs that includes standard basic anesthetic monitors and alarms [33]. Vital sign monitor alarms are disabled routinely during cardiopulmonary bypass (CPB), as the lack of pulsatile flow would cause the pulse oximeter alarm and other alarms to fire continuously. Eden et al. [34] developed an algorithm to identify separation from CPB by the return of pulsatile flow and implemented an AIMS-based CDS reminder to remind the user to reactivate the vital sign monitor alarms. The rate of alarm reactivation increased significantly in the post-implementation phase (from 22 to 63 %) [34].
Nair et al. implemented an AIMS CDS alert to notify the anesthesia provider if non-invasive blood pressure (NIBP) measurements had not been taken in the last 7 min. There was a significant reduction in the occurrence of extended NIBP gaps (>15 min) and the mean gap duration declined from 23.1 ± 2.0 to 18.6 ± 1.1 min (p < 0.001) [35]. Ehrenfeld et al. [36] conducted a prospective multicenter study where automated AIMS CDS tools were installed at two of the three centers to provide near real-time alerts to anesthesia providers of NIBP gaps; the incidence of gaps was reduced significantly (2.72 ± 0.60 % vs. 1.54 ± 0.19 %, p < 0.0001). In contrast, Epstein and Dexter described an AIMS CDS hypoxemia alert to send text pages to supervising anesthesiologists, but found that the system had low utility, as nearly all of the hypoxemic episodes were resolved before arrival of the anesthesiologist to the operating room [37].
There is relatively weak evidence (one study) to support AIMS CDS to remind anesthesia providers to enable vital sign monitor alarms after CPB (three “weak” votes). There is moderate evidence (two studies, one of which was a prospective multicenter study) to support AIMS CDS to remind anesthesia providers to obtain NIBP readings (two “moderate” votes, one “strong” vote). There is weak evidence (one retrospective study) against implementing AIMS CDS to alert clinicians of intraoperative hypoxemic episodes via text pages (three “weak” votes).
3.5 Intraoperative glucose management
Perioperative glycemic management is important to avoid complications from hyperglycemia and hypoglycemia, particularly in diabetic patients [38]. Nair et al. implemented an AIMS-based real-time CDS reminder to anesthesia providers to follow an institutional glucose management protocol. While compliance with the protocol (i.e. hourly glucose measurement and correct insulin doses) improved significantly, the AIMS CDS reminder did not improve mean glucose levels or other glycemic management parameters [39]. The authors postulated that this discrepancy existed because of a tendency for providers to adopt permissive hyperglycemia for fear of hypoglycemia under anesthesia, and an overall poor rate of compliance (24.2 %) with correct insulin doses even with the use of the CDS tool.
There is relatively weak evidence (one study) to support AIMS CDS for intraoperative blood glucose management for improved protocol compliance, and weak evidence that patient outcome measures are unaffected (three “weak” votes).
3.6 Intraoperative blood pressure management
Intraoperative hypertension and hypotension are associated with an increase in morbidity and mortality [40]. Nair et al. implemented AIMS-based near real-time notification of scenarios contributing to hypotension and hypertension. The CDS alert was associated with a reduction in the duration and frequency of hypotension with high concentrations of inhaled anesthetic (Δ = −0.26 % [CI −0.38 to −0.11 %], p < 0.001); the effect of the alert on anesthesia providers’ management of hypertension was significant but less than the management of hypotension [41]. In contrast, Panjasawatwong et al. [42] conducted a prospective randomized study of an AIMS alert for critically low systolic blood pressure and found that the additional warning did not reduce the duration of hypotension or hospitalization.
There is weak evidence (one study showing a reduction in hypotension, one study showing no effect) regarding the use of CDS in AIMS to manage intraoperative hypotension and hypertension (three “weak” votes).
3.7 Intraoperative ventilator management
Low tidal volume (Vt) ventilation has been shown to reduce mortality in acute lung injury (ALI) patients in the intensive care unit; however, anesthesiologists do not routinely use low tidal volume ventilation in the operating room [43]. Blum et al. [44] conducted a randomized controlled trial using an AIMS CDS alert that notified anesthesiologists via hospital pager that a patient had lab values that were associated with ALI and showed a clinically significant reduction in mean Vt from 508 to 458 mL (p = 0.033).
There is weak evidence (one study, one center) to support the use of CDS in AIMS to notify anesthesiologists of lab values that are associated with ALI to decrease tidal volumes (three “weak” votes).
3.8 Documentation compliance
The core function of AIMS remains recordkeeping, and many researchers have built AIMS CDS to enhance anesthesia providers’ compliance with documentation requirements. Choi et al. [45] showed a significant improvement in documentation compliance over a four-year period after implementing an AIMS with a custom-made anesthesia script for a specific or common surgical procedure. McCarty et al. described a significant increase in complete airway management documentation using real-time airway documentation guide CDS in the AIMS as part of a process improvement methodology [46]. Freundlich et al. [47] conducted a 3-year randomized trial and found that alerting anesthesia providers to documentation errors via automated pages resulted in improved documentation (baseline 33 %, post-intervention 87 %, p < 0.001). Nair et al. [48] used an AIMS CDS alert to notify anesthesia providers to document beta-blocker drug administration and improved documentation compliance from 60.5 to 94.6 % (p < 0.001). Sandberg et al. [49] implemented an automated AIMS-based paging system to remind providers to document patient allergy data and saw a compliance improvement from 70 to 92 % after initiating the alerts. Kheterpal et al. [50] showed an increase in arterial catheter documentation from 75 to 88 % after implementing an AIMS-based pager reminder.
There is strong evidence (multiple centers and prospective studies) that implementing AIMS CDS alerts can improve documentation completeness and compliance (three “strong” votes).
3.9 Resource conservation and utilization
High fresh gas flows (FGFs) can cause the wastage of expensive inhalational anesthetic to the scavenging system of an anesthesia machine [51]. Nair et al. [52] implemented real-time AIMS-based notification of high FGFs to anesthesia providers and saw the mean (±standard deviation) FGFs reduced from 2.10 ± 1.12 L/min during baseline to 1.60 ± 1.01 L/min when the CDS intervention was instituted (p < 0.001).
There is weak evidence (one study) supporting the use of AIMS CDS to manage FGFs during anesthesia (three “weak” votes).
4 Discussion
There is strong evidence for the inclusion of near real-time and point-of-care CDS in AIMS to enhance perioperative antibiotic prophylaxis compliance as well as documentation compliance and completeness. The other categories of AIMS CDS consisted mostly of limited (“weak”) evidence, typically because of a lack of studies and not the quality of the data.
In a few studies, reminders were associated with a more significant effect on desired provider behavior when the reminders were based on real-time CDS instead of predetermined time intervals. This may be due to better integration of CDS into the clinical workflow as well as improving the relevance and timeliness of the clinical messages [53, 54] This observation reinforces the importance of remembering the five “rights” of CDS, which consist of delivering the right information, to the right person, in the right intervention format, through the right channel, at the right time in workflow [55].
The published evidence for near real-time, point-of-care CDS in AIMS is promising yet limited despite the proliferation of AIMS in U.S. academic anesthesia departments (approximately 75 % by the end of 2014) [56]. In fact, the 25 articles analyzed in this review originated from only ten medical centers, perhaps because the necessary skill and experience to develop research platforms for CDS is not widely disseminated among anesthesiology practices. If this is indeed the case, then one solution may be to emphasize the incorporation of advanced clinical informatics training such as fellowships into more academic anesthesiology departments. The paucity of near real-time, point-of-care AIMS CDS articles may also be due to the challenges associated with conducting and publishing these studies, which are often based on quasi-experimental pre- and post-intervention design. Two concerns about this study design include the absence of randomization and unknown interceding events that might affect providers’ behavior during the study period, as well as the possibility of clustering events as a function of time [16]. One potential solution is to randomize the delivery of the CDS alert to generate both control and intervention groups [42].
Acute patient care—management of an anesthetic, providing care in an emergency department or an intensive care unit—involves a series of decision-action cycles that are intended to improve outcome. Decisions appear to improve when there is both situation awareness—which is defined as “the perception of elements of the environment within a volume of time and space, the comprehension of their meaning and the projection of their status in the near future [57]”—and option awareness, meaning that the array of available actions is also in view and in mind [58]. Both situation awareness (e.g., reliably obtaining blood pressures measurements at prescribed intervals) and option awareness (e.g., if the patient is hypotensive, then consider fluids, pressor medications, position change, etc.) must be present so that a firm basis exists for computed decision support. Furthermore, when measuring the performance of CDS with regard to achieving certain outcomes, one must keep in mind the strength of the evidence and clarity of the definitions that underlie the clinical behavior that CDS attempts to reinforce. For example, when studying anesthesia providers’ behavior when managing hypotension, a researcher must first identify, in operational terms, what exactly is hypotension that is sufficiently severe to be harmful yet not severe enough to be self-evident without requiring CDS. These terms and definitions vary across research studies, potentially affecting their generalizability and complicating comparisons between studies.
When reviewing CDS literature, it is important also to recognize the distinct difference between process measures and outcome measures. A CDS system is, by definition, intended to promote adherence to optimal processes, yet a wide chasm exists between showing increased adherence and demonstrating improved patient-focused outcomes. For example, in the two PONV CDS studies by Kappen et al. [28, 29], there was a difference between improving antiemetic dosing rates via CDS and producing an actual reduction in PONV. Furthermore, every CDS implementation involves adding reminders, alarms, and signals that clinicians will likely view as intrusive unless those additions demonstrably and favorably affect meaningful outcomes. Every AIMS CDS alarm, reminder and signal comes at the risk of inducing alert fatigue, which can occur when interruptive alerts distract the clinician from more clinically relevant alerts. This “signal-to-noise” concern has been studied extensively in EHR CDS [59], yet only one study [42] in this review addressed the risk of alert fatigue [60].
This study had several limitations. First, while the search queries were designed to be broadly inclusive, relevant studies might have been missed; indeed, we included one relevant article that we retrieved independently of our search queries. Second, the PRISMA-P guidelines mandate categorization, and while three reviewers performed the analysis, the grading remained largely arbitrary. With very few exceptions (such as CDS for antibiotic administration), much of the existing literature is based upon published experience with custom (or at least highly customized) proprietary AIMS and CDS systems. This may be due to regulatory implications if these symptoms were to prompt clinical interventions as compared to completion of documentation. Thus, a “weak” grade is less meaningful given this limitation to the application of CDS in AIMS despite the proliferation of AIMS; these matters may be too complex at this time to lend themselves to being graded meaningfully as “weak” or “strong” as the PRISMA-P guidelines require. Third, while we did not include context-sensitive checklists, the idea of CDS being capable of affecting outcomes by offering relevant checklists is also worthy of investigation (rather than telling providers explicitly what actions to perform, it might be helpful to present a checklist of relevant information); we plan to analyze such studies in a future review.
The evidence is substantial that CDS alerts help documentation compliance and perioperative antibiotic timing, but many questions remain. By what criteria should current AIMS be evaluated? Can AIMS-based point-of-care CDS alerts reduce perioperative medication errors and improve not only the timing of antibiotic administration but also drug dosing and allergy recognition [61]? To what extent does each new AIMS CDS alert raise the risk of inducing alert fatigue? Virtually all present-day AIMS have the core functionality of anesthetic record keeping combined with the ability to implement basic CDS. Real-time and near real-time CDS can be challenging for institutions to implement depending on their AIMS system [16]; however, as seen in the current study, tangible benefits can be realized even with basic CDS prompts and reminders. When evaluating AIMS systems, the extent to which CDS can be implemented and produce meaningful, measurable, and positive outcomes should be a priority. Patient safety is an all-encompassing challenge that requires knowledge and skills in multiple areas, including human factors and systems engineering, which is the application of knowledge about human characteristics, capabilities [physical, emotional, and intellectual], and limitations to the design and implementation of tools, devices, processes, and systems [62]. Situation awareness, option awareness, and human factors engineering are important factors to consider when selecting an AIMS, as is how well the AIMS CDS fits into clinicians’ workflow processes, which can have significant effects on patient safety and outcomes [63]. Future studies of AIMS CDS should consider and analyze the impact that new alerts may have on clinicians’ attention to established alerts. Despite the challenges that are associated with conducting studies of AIMS-based CDS, such research is necessary to improve patient safety, expand our understanding of which AIMS CDS tools are effective and worthwhile, and to ensure that future AIMS development and implementation are based on high-quality evidence from multiple centers.
References
Peters RM. Interactive microcomputer for acquisition of patient information. J Clin Monit. 1989;5:266–9.
Stonemetz J. Anesthesia information management systems marketplace and current vendors. Anesthesiol Clin. 2011;29:367–75.
Ehrenfeld JM, Rehman MA. Anesthesia information management systems: a review of functionality and installation considerations. J Clin Monit Comput. 2011;25:71–9.
Wanderer JP, Sandberg WS, Ehrenfeld JM. Real-time alerts and reminders using information systems. Anesthesiol Clin. 2011;29:389–96.
Kadry B, Feaster WW, Macario A, Ehrenfeld JM. Anesthesia information management systems: past, present, and future of anesthesia records. Mt Sinai J Med. 2012;79:154–65.
Hunt DL, Haynes RB, Hanna SE, Smith K. Effects of computer-based clinical decision support systems on physician performance and patient outcomes: a systematic review. JAMA. 1998;280:1339–46.
Chau A, Ehrenfeld JM. Using real-time clinical decision support to improve performance on perioperative quality and process measures. Anesthesiol Clin. 2011;29:57–69.
Spring SF, Sandberg WS, Anupama S, Walsh JL, Driscoll WD, Raines DE. Automated documentation error detection and notification improves anesthesia billing performance. Anesthesiology. 2007;106:157–63.
Kawamoto K, Houlihan CA, Balas EA, Lobach DF. Improving clinical practice using clinical decision support systems: a systematic review of trials to identify features critical to success. BMJ. 2005;330:765.
Garg AX, Adhikari NK, McDonald H, Rosas-Arellano MP, Devereaux PJ, Beyene J, Sam J, Haynes RB. Effects of computerized clinical decision support systems on practitioner performance and patient outcomes: a systematic review. JAMA. 2005;293:1223–38.
Wanderer JP, Ehrenfeld JM. Clinical decision support for perioperative information management systems. Semin Cardiothorac Vasc Anesth. 2013;17:288–93.
Stabile M, Cooper L. Review article: the evolving role of information technology in perioperative patient safety. Can J Anaesth. 2013;60:119–26.
Gálvez JA, Rothman BS, Doyle CA, Morgan S, Simpao AF, Rehman MA. A narrative review of meaningful use and anesthesia information management systems. Anesth Analg. 2015;121:693–706.
Vakharia SB, Rinehart J. Using anesthesia AIMS data in quality management. Int Anesthesiol Clin. 2014;52:42–52.
Zanetti G, Flanagan HL Jr, Cohn LH, Giardina R, Platt R. Improvement of intraoperative antibiotic prophylaxis in prolonged cardiac surgery by automated alerts in the operating room. Infect Control Hosp Epidemiol. 2003;24:13–6.
Epstein RH, Dexter F, Patel N. Influencing anesthesia provider behavior using anesthesia information management system data for near real-time alerts and post hoc reports. Anesth Analg. 2015;121:678–92.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1.
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA, the PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;349:g7647.
Guyatt GH, Oxman AD, Vist G, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schünemann HJ, for the GRADE Working Group. Rating quality of evidence and strength of recommendations GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–6.
Classen DC, Evans RS, Pestotnik SL, Horn SD, Menlove RL, Burke JP. The timing of prophylactic administration of antibiotics and the risk of surgical-wound infection. N Engl J Med. 1992;326:281–6.
Schwann NM, Bretz KA, Eid S, Burger T, Fry D, Ackler F, Evans P, Romancheck D, Beck M, Ardire AJ, Lukens H, McLoughlin TM. Point-of-care electronic prompts: an effective means of increasing compliance, demonstrating quality, and improving outcome. Anesth Analg. 2011;113:869–76.
Nair BG, Newman SF, Peterson GN, Wu WY, Schwid HA. Feedback mechanisms including real-time electronic alerts to achieve near 100% timely prophylactic antibiotic administration in surgical cases. Anesth Analg. 2010;111:1293–300.
Wax DB, Beilin Y, Levin M, Chadha N, Krol M, Reich DL. The effect of an interactive visual reminder in an anesthesia information management system on timeliness of prophylactic antibiotic administration. Anesth Analg. 2007;104:1462–6.
Zanetti G, Giardina R, Platt R. Intraoperative redosing of cefazolin and risk for surgical site infection in cardiac surgery. Emerg Infect Dis. 2001;7:828–31.
St Jacques P, Sanders N, Patel N, Talbot TR, Deshpande JK, Higgins M. Improving timely surgical antibiotic prophylaxis redosing administration using computerized record prompts. Surg Infect (Larchmt). 2005;6:215–21.
Nair BG, Newman SF, Peterson GN, Schwid HA. Automated electronic reminders to improve redosing of antibiotics during surgical cases: comparison of two approaches. Surg Infect (Larchmt). 2011;12:57–63.
Kranke P, Eberhart LH. Possibilities and limitations in the pharmacological management of postoperative nausea and vomiting. Eur J Anaesthesiol. 2011;28:758–65.
Kappen TH, Moons KG, van Wolfswinkel L, Kalkman CJ, Vergouwe Y, van Klei WA. Impact of risk assessments on prophylactic antiemetic prescription and the incidence of postoperative nausea and vomiting: a cluster-randomized trial. Anesthesiology. 2014;120:343–54.
Kappen TH, Vergouwe Y, van Wolfswinkel L, Kalkman CJ, Moons KG, van Klei WA. Impact of adding therapeutic recommendations to risk assessments from a prediction model for postoperative nausea and vomiting. Br J Anaesth. 2015;114:252–60.
Kooij FO, Klok T, Hollmann MW, Kal JE. Decision support increases guideline adherence for prescribing postoperative nausea and vomiting prophylaxis. Anesth Analg. 2008;106:893–8.
Kooij FO, Vos N, Siebenga P, Klok T, Hollmann MW, Kal JE. Automated reminders decrease postoperative nausea and vomiting incidence in a general surgical population. Br J Anaesth. 2012;108:961–5.
Kooij FO, Klok T, Hollmann MW, Kal JE. Automated reminders increase adherence to guidelines for administration of prophylaxis for postoperative nausea and vomiting. Eur J Anaesthesiol. 2010;27:187–91.
American Society of Anesthesiologists Standards for Basic Anesthetic Monitoring. http://www.asahq.org/~/media/sites/asahq/files/public/resources/standards-guidelines/standards-for-basic-anesthetic-monitoring.pdf. Last Accessed 19 April 2016.
Eden A, Pizov R, Toderis L, Kantor G, Perel A. The impact of an electronic reminder on the use of alarms after separation from cardiopulmonary bypass. Anesth Analg. 2009;108:1203–8.
Nair BG, Horibe M, Newman SF, Wu WY, Schwid HA. Near real-time notification of gaps in cuff blood pressure recordings for improved patient monitoring. J Clin Monit Comput. 2013;27:265–71.
Ehrenfeld JM, Epstein RH, Bader S, Kheterpal S, Sandberg WS. Automatic notifications mediated by anesthesia information management systems reduce the frequency of prolonged gaps in blood pressure documentation. Anesth Analg. 2011;113:356–63.
Epstein RH, Dexter F. Implications of resolved hypoxemia on the utility of desaturation alerts sent from an anesthesia decision support system to supervising anesthesiologists. Anesth Analg. 2012;115:929–33.
Sudhakaran S, Surani SR. Guidelines for perioperative management of the diabetic patient. Surg Res Pract. 2015;2015:284063.
Nair BG, Grunzweig K, Peterson GN, Horibe M, Neradilek MB, Newman SF, Van Norman G, Schwid HA, Hao W, Hirsch IB, Patchen Dellinger E. Intraoperative blood glucose management: impact of a real-time decision support system on adherence to institutional protocol. J Clin Monit Comput. 2015. doi:10.1007/s10877-015-9718-3.
Monk TG, Bronsert MR, Henderson WG, Mangione MP, Sum-Ping ST, Bentt DR, Nguyen JD, Richman JS, Meguid RA, Hammermeister KE. Association between intraoperative hypotension and hypertension and 30-day postoperative mortality in noncardiac surgery. Anesthesiology. 2015;123:307–19.
Nair BG, Horibe M, Newman SF, Wu WY, Peterson GN, Schwid HA. Anesthesia information management system-based near real-time decision support to manage intraoperative hypotension and hypertension. Anesth Analg. 2014;118:206–14.
Panjasawatwong K, Sessler DI, Stapelfeldt WH, Mayers DB, Mascha EJ, Yang D, Kurz A. A randomized trial of a supplemental alarm for critically low systolic blood pressure. Anesth Analg. 2015;121:1500–7.
Blum JM. A description of intraoperative ventilator management in patients with acute lung injury and the use of lung protective ventilation strategies. Anesthesiology. 2011;115:75–82.
Blum JM, Stentz MJ, Maile MD, Jewell E, Raghavendran K, Engoren M, Ehrenfeld JM. Automated alerting and recommendations for the management of patients with preexisting hypoxia and potential acute lung injury: a pilot study. Anesthesiology. 2013;119:295–302.
Choi CK, Saberito D, Tyagaraj C, Tyagaraj K. Organizational performance and regulatory compliance as measured by clinical pertinence indicators before and after implementation of Anesthesia information management system (AIMS). J Med Syst. 2014;38:5.
McCarty LK, Saddawi-Konefka D, Gargan LM, Driscoll WD, Walsh JL, Peterfreund RA. Application of process improvement principles to increase the frequency of complete airway management documentation. Anesthesiology. 2014;121:1166–74.
Freundlich RE, Barnet CS, Mathis MR, Shanks AM, Tremper KK, Kheterpal S. A randomized trial of automated electronic alerts demonstrating improved reimbursable anesthesia time documentation. J Clin Anesth. 2013;25:110–4.
Nair BG, Peterson GN, Newman SF, Wu WY, Kolios-Morris V, Schwid HA. Improving documentation of a beta-blocker quality measure through an anesthesia information management system and real-time notification of documentation errors. Jt Comm J Qual Patient Saf. 2012;38:283–8.
Sandberg WS, Sandberg EH, Seim AR, Anupama S, Ehrenfeld JM, Spring SF, Walsh JL. Real-time checking of electronic anesthesia records for documentation errors and automatically text messaging clinicians improves quality of documentation. Anesth Analg. 2008;106:192–201.
Kheterpal S, Gupta R, Blum JM, Tremper KK, O’Reilly M, Kazanjian PE. Electronic reminders improve procedure documentation compliance and professional fee reimbursement. Anesth Analg. 2007;104:592–7.
Dexter F, Maguire D, Epstein RH. Observational study of anaesthetists’ fresh gas flow rates during anesthesia with desflurane, isoflurane and sevoflurane. Anaesth Intensive Care. 2011;39:460–4.
Nair BG, Peterson GN, Neradilek MB, Newman SF, Huang EY, Schwid HA. Reducing wastage of inhalation anesthetics using real-time decision support to notify of excessive fresh gas flow. Anesthesiology. 2013;118:874–84.
Moja L, Liberati EG, Galuppo L, Gorli M, Maraldi M, Nanni O, Rigon G, Ruggieri P, Ruggiero F, Scaratti G, Vaona A, Kwag KH. Barriers and facilitators to the uptake of computerized clinical decision support systems in specialty hospitals: protocol for a qualitative cross-sectional study. Implement Sci. 2014;9:105.
Moxey A, Robertson J, Newby D, Hains I, Williamson M, Pearson SA. Computerized clinical decision support for prescribing: provision does not guarantee uptake. J Am Med Inform Assoc. 2010;17:25–33.
Osheroff JA. Improving medication use and outcomes with clinical decision support: a step-by-step guide. Chicago: The Healthcare Information and Management Systems Society; 2009.
Stol IS, Ehrenfeld JM, Epstein RH. Technology diffusion of anesthesia information management systems into academic anesthesia departments in the United States. Anesth Analg. 2014;118:644–50.
Endsley MR. Design and evaluation for situation awareness enhancement. In: Proceedings of the human factors society 32nd annual meeting; 1988. pp. 97–101.
Schulz CM, Endsley MR, Kochs EF, Gelb AW, Wagner KJ. Situation awareness in anesthesia: concept and research. Anesthesiology. 2013;118:729–42.
Phansalkar S, van der Sijs H, Tucker AD, Desai AA, Bell DS, Teich JM, Middleton B, Bates DW. Drug-drug interactions that should be non-interruptive in order to reduce alert fatigue in electronic health records. J Am Med Inform Assoc. 2013;20:489–93.
McDaniel RB, Burlison JD, Baker DK, Hasan M, Robertson J, Hartford C, Howard SC, Sablauer A, Hoffman JM. Alert dwell time: introduction of a measure to evaluate interruptive clinical decision support alerts. J Am Med Inform Assoc. 2016;23:138–41.
Nanji KC, Patel A, Shaikh S, Seger DL, Bates DW. Evaluation of perioperative medication errors and adverse drug events. Anesthesiology. 2016;124:25–34.
Weinger MB, Gaba DM. Human factors engineering in patient safety. Anesthesiology. 2014;120:801–6.
Carayan P, Wood KE. Patient safety: the role of human factors and systems engineering. Stud Health Technol Inform. 2010;153:23–46.
Authors’ contribution
A.F.S., J.M.T., A.M.L., J.A.G., S.E.M., and M.A.K. contributed substantially to the conception and design of this review, drafted the article and revised it critically for important intellectual content, approved of the final version to be published, and agree to be accountable for all aspects of the work thereby ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding
This work was supported only by departmental resources.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Allan F. Simpao is on the associate editorial board for Anesthesiology, a U.S. anesthesia journal. Jorge A. Galvez is on the associate editorial board for Anesthesiology, a U.S. anesthesia journal. Microsoft provided funds for the development for Pedi Crisis, an app that Dr. Galvez developed. All funding was applied to software development costs; Dr. Galvez did not receive monetary compensation or support from Microsoft for the app development. The remaining authors declare that they have no conflict of interest.
Appendix
Appendix
1.1 Medline search query
Search ((((((anesthesia OR anaesthesia OR anesthesiology OR anesthesiologist* OR anaesthesiologist* OR anaesthesiology OR periop* OR PACU OR post-anesthes* OR post-anaesthes* OR postanaesthes* OR postanesthes* AND (information AND manag*) AND decision*))) AND ( “2000/01/01”[PDat]: “2015/12/31”[PDat]) AND English[lang]))) OR ((((((((((((((((((((((integrated advanced information management systems[MeSH Terms]) OR Information Management[MeSH Terms]) OR “anesthesia information management”) OR “electronic health records”) OR Medical Records Systems, Computerized[MeSH Terms]) OR Hospital Information Systems[MeSH Terms]) OR decision support systems, clinical[MeSH Terms]) OR decision support techniques[MeSH Terms]))) AND (((anesthesia* OR anaesthesia* OR anesthesiologist* OR anaesthesiologist* OR anesthesia[MeSH Terms]))))) AND (“2000/01/01”[PDat]: “2015/12/31”[PDat]))) NOT “case reports”[Publication Type]) NOT “review”[Publication Type]) AND hasabstract[text] AND Humans[Mesh] AND English[lang]))))))
1.2 EMBASE search query
No. | Results | Query |
|---|---|---|
#12 | 162 | #8 OR #9 AND [embase]/lim NOT [medline]/lim AND [english]/lim |
#11 | 162 | #8 OR #9 AND [embase]/lim NOT [medline]/lim |
#10 | 506 | #8 OR #9 |
#9 | 6 | #1 AND #2 AND #3 AND (anesthes*:ti OR anesthes*:ab) AND decision*:ti AND [embase]/lim |
#8 | 506 | #1 AND #2 AND #3 AND decision*:ti AND [english]/lim AND [2000–2015]/py |
#7 | 6 | #1 AND #2 AND #3 AND (anesthes*:ti OR anesthes*:ab) AND decision*:ti |
#6 | 1747 | #1 AND #2 AND #3 AND [english]/lim AND [2000-2015]/py |
#5 | 1768 | #1 AND #2 AND #3 AND [english]/lim |
#4 | 1790 | #1 AND #2 AND #3 |
#3 | 15,751 | ‘decision support system’/exp OR ‘clinical decision support’ |
#2 | 108,258 | ‘electronic medical record’/exp OR ‘electronic medical record’ OR ‘electronic health record’ OR ehr* or emr* |
#1 | 120,669 | ‘information system’/exp OR ‘information management’ OR ‘anesthesia information management system’ |
Rights and permissions
About this article
Cite this article
Simpao, A.F., Tan, J.M., Lingappan, A.M. et al. A systematic review of near real-time and point-of-care clinical decision support in anesthesia information management systems. J Clin Monit Comput 31, 885–894 (2017). https://doi.org/10.1007/s10877-016-9921-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-016-9921-x