Abstract
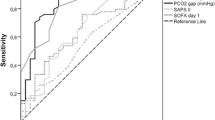
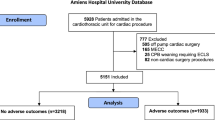
Alteration of tissue perfusion is a main contributor of organ dysfunction. In cardiac surgery, the importance of organ dysfunction is associated with worse outcome. Central venous-arterial difference in CO2 tension (ΔCO2) has been proposed as a global marker of the adequacy of tissue perfusion in shock states. We hypothesized that ΔCO2 could be increased in case of postoperative organ failure or worse outcome. In this monocentric retrospective cohort study, we retrieved, from our database, 220 consecutive patients admitted in intensive care after an elective cardiac surgery. Four time points were formed: ICU admission, and 6, 24 and 48 h after. A ΔCO2 below 6 mmHg defined the normal range values. The SOFA score, intensive care unit and hospital length of stay, hospital and 6-month mortality rate were recorded. We compared patient with low ΔCO2 (<6 mmHg) and high ΔCO2 (≥6 mmHg). We included 55 (25 %) and 165 patients in low and high ΔCO2 groups, respectively. The SOFA score, the hospital and 6 months mortality rate were higher in patients with low ΔCO2. Surprisingly, we did not find results previously published in other surgical settings. In cardiac surgery, ΔCO2 has a low predictive value of outcome.


Similar content being viewed by others
References
Shoemaker WC, Appel PL, Kram HB. Role of oxygen debt in the development of organ failure sepsis, and death in high-risk surgical patients. Chest. 1992;102(1):208–15.
Patila T, Kukkonen S, Vento A, Pettila V, Suojaranta-Ylinen R. Relation of the Sequential Organ Failure Assessment score to morbidity and mortality after cardiac surgery. Ann Thorac Surg. 2006;82(6):2072–8.
Dres M, Monnet X, Teboul JL. Hemodynamic management of cardiovascular failure by using PCO(2) venous-arterial difference. J Clin Monit Comput. 2012;26(5):367–74. doi:10.1007/s10877-012-9381-x.
Danin PE, Siegenthaler N, Levraut J, Bernardin G, Dellamonica J, Bendjelid K. Monitoring CO2 in shock states. J Clin Monit Comput. 2015;29(5):591–600. doi:10.1007/s10877-014-9638-7.
Cuschieri J, Rivers EP, Donnino MW, Katilius M, Jacobsen G, Nguyen HB, Pamukov N, Horst HM. Central venous-arterial carbon dioxide difference as an indicator of cardiac index. Intensive Care Med. 2005;31(6):818–22.
Lamia B, Monnet X, Teboul JL. Meaning of arterio-venous PCO2 difference in circulatory shock. Minerva Anestesiol. 2006;72(6):597–604.
Vallet B, Teboul JL, Cain S, Curtis S. Venoarterial CO(2) difference during regional ischemic or hypoxic hypoxia. J Appl Physiol. 2000;89(4):1317–21.
Futier E, Robin E, Jabaudon M, Guerin R, Petit A, Bazin JE, Constantin JM, Vallet B. Central venous O(2) saturation and venous-to-arterial CO(2) difference as complementary tools for goal-directed therapy during high-risk surgery. Crit Care. 2010;14(5):R193. doi:10.1186/cc9310.
Robin E, Futier E, Pires O, Fleyfel M, Tavernier B, Lebuffe G, Vallet B. Central venous-to-arterial carbon dioxide difference as a prognostic tool in high-risk surgical patients. Crit Care. 2015;19:227. doi:10.1186/s13054-015-0917-6.
Ariza M, Gothard JW, Macnaughton P, Hooper J, Morgan CJ, Evans TW. Blood lactate and mixed venous-arterial PCO2 gradient as indices of poor peripheral perfusion following cardiopulmonary bypass surgery. Intensive Care Med. 1991;17(6):320–4.
Jakob SM, Ruokonen E, Takala J. Assessment of the adequacy of systemic and regional perfusion after cardiac surgery. Br J Anaesth. 2000;84(5):571–7.
Lebuffe G, Decoene C, Pol A, Prat A, Vallet B. Regional capnometry with air-automated tonometry detects circulatory failure earlier than conventional hemodynamics after cardiac surgery. Anesth Analg. 1999;89(5):1084–90.
Polonen P, Ruokonen E, Hippelainen M, Poyhonen M, Takala J. A prospective, randomized study of goal-oriented hemodynamic therapy in cardiac surgical patients. Anesth Analg. 2000;90(5):1052–9.
Ruokonen E, Soini HO, Parviainen I, Kosonen P, Takala J. Venoarterial CO2 gradient after cardiac surgery: relation to systemic and regional perfusion and oxygen transport. Shock. 1997;8(5):335–40.
Takami Y, Masumoto H. Mixed venous-arterial CO2 tension gradient after cardiopulmonary bypass. Asian Cardiovasc Thorac Ann. 2005;13(3):255–60.
Cavaliere F, Martinelli L, Guarneri S, Varano C, Rossi M, Schiavello R. Arterial-venous PCO2 gradient in early postoperative hours following myocardial revascularization. J Cardiovasc Surg (Torino). 1996;37(5):499–503.
Vallee F, Vallet B, Mathe O, Parraguette J, Mari A, Silva S, Samii K, Fourcade O, Genestal M. Central venous-to-arterial carbon dioxide difference: an additional target for goal-directed therapy in septic shock? Intensive Care Med. 2008;34(12):2218–25.
Hein OV, Birnbaum J, Wernecke K, England M, Konertz W, Spies C. Prolonged intensive care unit stay in cardiac surgery: risk factors and long-term-survival. Ann Thorac Surg. 2006;81(3):880–5. doi:10.1016/j.athoracsur.2005.09.077.
De Backer D, Dubois MJ, Schmartz D, Koch M, Ducart A, Barvais L, Vincent JL. Microcirculatory alterations in cardiac surgery: effects of cardiopulmonary bypass and anesthesia. Ann Thorac Surg. 2009;88(5):1396–403.
De Somer F. End-organ protection in cardiac surgery. Minerva Anestesiol. 2013;79(3):285–93.
Goepfert MS, Richter HP, Zu Eulenburg C, Gruetzmacher J, Rafflenbeul E, Roeher K, von Sandersleben A, Diedrichs S, Reichenspurner H, Goetz AE, Reuter DA. Individually optimized hemodynamic therapy reduces complications and length of stay in the intensive care unit: a prospective, randomized controlled trial. Anesthesiology. 2013;119(4):824–36. doi:10.1097/ALN.0b013e31829bd770.
Morel J, Bouchet JB, Vola M, Beraud AM, Clerc M, Awad S, Auboyer C, Molliex S. Tissue near infra red spectroscopy change is not correlated with patients’ outcome in elective cardiac surgery. Acta Anaesthesiol Scand. 2014;58(7):835–42. doi:10.1111/aas.12329.
Teboul JL, Mercat A, Lenique F, Berton C, Richard C. Value of the venous-arterial PCO2 gradient to reflect the oxygen supply to demand in humans: effects of dobutamine. Crit Care Med. 1998;26(6):1007–10.
Ralley FE, Wynands JE, Ramsay JG, Carli F, MacSullivan R. The effects of shivering on oxygen consumption and carbon dioxide production in patients rewarming from hypothermic cardiopulmonary bypass. Can J Anaesth. 1988;35(4):332–7. doi:10.1007/bf03010851.
De Blasi RA, Tonelli E, Arcioni R, Mercieri M, Cigognetti L, Romano R, Pinto G. In vivo effects on human skeletal muscle oxygen delivery and metabolism of cardiopulmonary bypass and perioperative hemodilution. Intensive Care Med. 2012;38(3):413–21. doi:10.1007/s00134-011-2404-0.
Perz S, Uhlig T, Kohl M, Bredle DL, Reinhart K, Bauer M, Kortgen A. Low and “supranormal” central venous oxygen saturation and markers of tissue hypoxia in cardiac surgery patients: a prospective observational study. Intensive Care Med. 2011;37(1):52–9. doi:10.1007/s00134-010-1980-8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None declared.
Rights and permissions
About this article
Cite this article
Morel, J., Grand, N., Axiotis, G. et al. High veno-arterial carbon dioxide gradient is not predictive of worst outcome after an elective cardiac surgery: a retrospective cohort study. J Clin Monit Comput 30, 783–789 (2016). https://doi.org/10.1007/s10877-016-9855-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-016-9855-3