Abstract
Purpose
We aimed to explore how patients make decisions regarding use of preimplantation genetic testing for aneuploidy (PGT-A) for in vitro fertilization (IVF).
Methods
This is a cross-sectional survey at an academic medical center. Three hundred subjects initiating an IVF cycle over 8 weeks were asked to complete a validated survey to determine how they decided whether or not to pursue PGT-A. All patients were previously counseled that the primary goal of PGT-A is to maximize pregnancy rates per embryo transfer. Survey responses were compared between those who elected PGT-A and those who did not with a chi-squared or t test.
Results
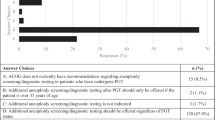
Of 191 subjects who completed the survey, 117 (61%) planned PGT-A, while 74 (39%) did not. Among those who decided to undergo PGT-A, 56% stated their primary reason was to have a healthy baby, while 18% chose PGT-A to reduce the incidence of birth defects, and 16% aimed to decrease the risk of miscarriage. Patients who decided not to pursue PGT-A stated they prioritized avoiding the scenario in which they might have no embryos to transfer (36%) or reducing cost (31%). Both groups rated physicians as the single most important source of information in their decision-making (56% vs 68%, p = NS).
Conclusions
Patients who chose to undergo PGT-A have different priorities from those who do not. Many patients planning PGT-A do so for reasons that are not evidence-based. While patients cite physicians as their primary source of information in the decision-making process, rationales for selecting PGT-A are inconsistent with physician counseling.


Similar content being viewed by others
References
De Rycke M, Goossens V, Kokkali G, Meijer-Hoogeveen M, Coonen E, Moutou C. ESHRE PGD Consortium data collection XIV-XV: cycles from January 2011 to December 2012 with pregnancy follow-up to October 2013. Hum Reprod. 2017;32(10):1974–94.
Gleicher N, Barad DH. A review of, and commentary on, the ongoing second clinical introduction of preimplantation genetic screening (PGS) to routine IVF practice. J Assist Reprod Genet. 2012;29(11):1159–66.
Mastenbroek S, Repping S. Preimplantation genetic screening: back to the future. Hum Reprod. 2014;29(9):1846–50.
Paulson RJ. Every last baby out of every last egg: the appropriate goal for fertility treatment in women older than 40 years. Fertil Steril. 2016;105:1443–4.
Yang Z, Liu J, Collins GS, Salem SA, Liu X, Lyle SS, et al. Selection of single blastocysts for fresh transfer via standard morphology assessment alone and with array CGH for good prognosis IVF patients: results from a randomized pilot study. Mol Cytogenet. 2012;5:24.
Scott RT, Upham KM, Forman EJ, Hong KH, Scott KL, Taylor D, et al. Blastocyst biopsy with comprehensive chromosome screening and fresh embryo transfer significantly increases in vitro fertilization implantation and delivery rates: a randomized controlled trial. Fertil Steril. 2013;100:697–703.
Practice Committee of the American Society for Reproductive Medicine. The use of preimplantation genetic testing for aneuploidy (PGT-A): a committee opinion. Fertil Steril. 2018;109:429–36.
Geraedts J, Sermon K. Preimplantation genetic screening 2.0: the theory. Mol Hum Reprod. 2016;22(8):839–44.
Capalbo A, Treff NR, Cimadomo D, Tao X, Upham K, Ubaldi FM, et al. Comparison of array comparative genomic hybridization and quantitative real-time PCR-based aneuploidy screening of blastocyst biopsies. Eur J Hum Genet. 2015;l23:901–6.
Fiorentino F, Bono S, Biricik A, Nuccitelli A, Cotroneo E, Cottone G, et al. Application of next-generation sequencing technology for comprehensive aneuploidy screening of blastocysts in clinical preimplantation genetic screening cycles. Hum Reprod. 2014;29(12):2802–13.
Stiggelbout AM, Van der Weijden T, De Wit MPT, Frosch D, Legare F, Montori VM, et al. Shared decision making: really putting patients at the centre of healthcare. BMJ. 2012;344:e256. https://doi.org/10.1136/bmj.e256.
Sermon K, Capalbo A, Cohen J, Coonen E, De Rycke M, De Vos A, et al. The why, the how and the when of PGS 2.0: current practices and expert opinions of fertility specialists, molecular biologists, and embryologists. Mol Hum Reprod. 2016;22(8):845–57.
Godwin Y. Do they listen? A review of information retained by patients following consent for reduction mammoplasty. Br J Plast Surg. 2000;53:121–5.
Turner P, Williams C. Informed consent: patients listen and read, but what information do they retain? N Z Med J. 2001;115(1164):U218.
Naini P, Lewis J, Rajanna K, Weir AB 3rd. Evaluation of a method to improve the consent process: improved data retention with stagnant comprehension. J Cancer Educ. 2013;28(1):38–42.
Langdon IJ, Hardin R, Learmonth ID. Informed consent for total hip arthroplasty: does a written information sheet improve recall by patients? Ann R Coll Surg Engl. 2001;84(6):404–8.
Ruiz JG, Andrade AD, Anam R, Lisigurski M, Karanam C, Sharit J. Computer-based programmed instruction did not improve the knowledge retention of medication instructions of individuals with type 2 diabetes mellitus. Diabetes Educ. 2014;40(1):77–88.
Anderson JL, Dodman S, Kopelman M, Fleming A. Patient information recall in a rheumatology clinic. Rheumatol Rehabil. 1979;18:244–55.
Bennett LR, Wiweko B, Bell L, Shafira N, Pangestu M, Adayana IB, et al. Reproductive knowledge and patient education needs among Indonesian women infertility patients attending three fertility clinics. Patient Educ Couns. 2015;98(3):364–9.
Ley P. Memory for medical information. Br J Soc Clin Psychol. 1979;18:245–55.
Hassold T, Hunt P. To err (meiotically) is human: the genesis of human aneuploidy. Nat Rev Genet. 2001;2:280–91.
Murugappan G, Shahine LK, Perfetto CO, Hickok LR, Lathi RB. Intent to treat analysis of in vitro fertilization and preimplantation genetic screening versus expectant management in patients with recurrent pregnancy loss. Hum Reprod. 2016;31:1668–74.
Cedars MI. Fresh versus frozen: initial transfer or cumulative cycle results: how do we interpret results and design studies? Fertil Steril. 2016;106(2):251–6.
Forman EJ, Hong KH, Ferry KM, Tao X, Taylor D, Levy B, et al. In vitro fertilization with single euploid blastocyst transfer: a randomized controlled trial. Fertil Steril. 2013;100:100–7.
Treff NR, Ferry KM, Zhao T, Su J, Forman EJ, Scott RT. Cleavage stage embryo biopsy significantly impairs embryonic reproductive potential while blastocyst biopsy does not: a novel paired analysis of cotransferred biopsied and non-biopsied sibling embryos. Fertil Steril. 2011;96:52.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the UCSF Committee on Human Research.
Rights and permissions
About this article
Cite this article
Quinn, M.M., Juarez-Hernandez, F., Dunn, M. et al. Decision-making surrounding the use of preimplantation genetic testing for aneuploidy reveals misunderstanding regarding its benefit. J Assist Reprod Genet 35, 2155–2159 (2018). https://doi.org/10.1007/s10815-018-1337-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-018-1337-8