Abstract
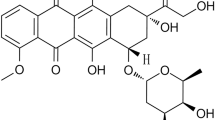
Bot III neurotoxin is the most lethal α neurotoxin purified from Buthus occitanus tunetanus scorpion venom. This toxin binds to the voltage-gated sodium channel of excitable cells and blocks its inactivation, inducing an increased release of neurotransmitters (acetylcholine and catecholamines). This study aims to elucidate the involvement of cholinergic and adrenergic receptors in pathogenesis and inflammatory response triggered by this toxin. Injection of Bot III to animals induces an increase of peroxidase activities, an imbalance of oxidative status, tissue damages in lung parenchyma, and myocardium correlated with metabolic disorders. The pretreatment with nicotine (nicotinic receptor agonist) or atropine (muscarinic receptor antagonist) protected the animals from almost all disorders caused by Bot III toxin, especially the immunological alterations. Bisoprolol administration (selective β1 adrenergic receptor antagonist) was also efficient in the protection of animals, mainly on tissue damage. Propranolol (non-selective adrenergic receptor antagonist) showed less effect. These results suggest that both cholinergic and adrenergic receptors are activated in the cardiopulmonary manifestations induced by Bot III. Indeed, the muscarinic receptor appears to be more involved than the nicotinic one, and the β1 adrenergic receptor seems to dominate the β2 receptor. These results showed also that the activation of nicotinic receptor leads to a significant protection of animals against Bot III toxin effect. These findings supply a supplementary data leading to better understanding of the mechanism triggered by scorpionic neurotoxins and suggest the use of drugs targeting these receptors, especially the nicotinic one in order to counteract the inflammatory response observed in scorpion envenomation.






Similar content being viewed by others
Abbreviations
- Ach:
-
Acetyl-choline
- Bot III toxin:
-
Neurotoxin purified from Buthus occitanus tunetanus scorpion venom
- mAch-R:
-
Muscarinic receptor
- nAch-R:
-
Nicotinic receptor
References
Gueron, M., and R. Ilia. 1996. Non-cardiogenic pulmonary oedema after scorpion envenomation: a true entity? Toxicon 34(4): 393–395.
Sofer, S., et al. 1996. Interleukin-6 release following scorpion sting in children. Toxicon 34(3): 389–392.
Hammoudi-Triki, D., et al. 2007. Toxicokinetic and toxicodynamic analyses of Androctonus australis hector venom in rats: optimization of antivenom therapy. Toxicology and applied pharmacology 218(3): 205–214.
Martin-Eauclaire, M.-F., et al. 1999. Les toxines des venins de scorpion. Annales de l’Institut Pasteur. 10: 207–222. Elsevier: France.
Martin, M., and H. Rochat. 1984. Purification of thirteen toxins active on mice from the venom of the North African scorpion Buthus occitanus tunetanus. Toxicon 22(2): 279–291.
Martin, M., and H. Rochat. 1986. Large scale purification of toxins from the venom of the scorpion Androctonus australis Hector. Toxicon 24(11): 1131–1139.
Bougis, P.E., H. Rochat, and L.A. Smith. 1989. Precursors of Androctonus australis scorpion neurotoxins. Structures of precursors, processing outcomes, and expression of a functional recombinant toxin II. Journal of Biological Chemistry 264(32): 19259–19265.
Benkhadir, K., et al. 2004. Molecular cloning and functional expression of the alpha-scorpion toxin BotIII: pivotal role of the C-terminal region for its interaction with voltage-dependent sodium channels. Peptides 25(2): 151–161.
Yarom, R., M. Gueron, and K. Braun. 1970. Scorpion venom cardiomyopathy. Pathobiology 35(1–3): 114–117.
Freire-Maia, L., and I.M. de Matos. 1993. Heparin or a PAF antagonist (BN-52021) prevents the acute pulmonary edema induced by Tityus serrulatus scorpion venom in the rat. Toxicon 31(9): 1207–1210.
Ismail, M. 1995. The scorpion envenoming syndrome. Toxicon 33(7): 825–858.
de Davila, C.A.M., et al. 2002. Sympathetic nervous system activation, antivenin administration and cardiovascular manifestations of scorpion envenomation. Toxicon 40(9): 1339–1346.
Van Oosterhout, A., et al. 1996. Role of interleukin-5 and substance P in development of airway hyperreactivity to histamine in guinea-pigs. European Respiratory Journal 9(3): 493–499.
Bertazzi, D.T., et al. 2003. Effect of Tityus serrulatus scorpion venom and its major toxin, TsTX-I, on the complement system in vivo. Toxicon 41(4): 501–508.
Ergün, Y., et al. 2011. Evaluation of nitrite/nitrate levels in relation to oxidative stress parameters in liver cirrhosis. Clinics and Research in Hepatology and Gastroenterology 35(4): 303–308.
Ohkawa, H., N. Ohishi, and K. Yagi. 1979. Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Analytical Biochemistry 95(2): 351–358.
Aebi, H. 1984. [13] Catalase in vitro. Methods in Enzymology 105: 121–126.
Sami-Merah, S., et al. 2008. Combination of two antibody fragments F (ab’) 2/Fab: An alternative for scorpion envenoming treatment. International Immunopharmacology 8(10): 1386–1394.
Raouraoua-Boukari, R., et al. 2012. Immunomodulation of the inflammatory response induced by Androctonus australis hector neurotoxins: biomarker interactions. Neuroimmunomodulation 19(2): 103–110.
Adi-Bessalem, S., et al. 2012. Lung immunoreactivity and airway inflammation: Their assessment after scorpion envenomation. Inflammation 35(2): 501–508.
Bekkari, N., M.-F. Martin-Eauclaire, and F. Laraba-Djebari. 2015. Complement system and immunological mediators: Their involvements in the induced inflammatory process by Androctonus australis hector venom and its toxic components. Experimental and Toxicologic Pathology 67: 389.
Dousset, E., et al. 2005. Evidence that free radical generation occurs during scorpion envenomation. Comparative Biochemistry and Physiology Part C: Toxicology & Pharmacology 140(2): 221–226.
Folkerts, G., et al. 2001. Reactive nitrogen and oxygen species in airway inflammation. European Journal of Pharmacology 429(1): 251–262.
Endo, S., et al. 1996. Nitrite/nitrate oxide (NOx) and cytokine levels in patients with septic shock. Research Communications in Molecular Pathology and Pharmacology 91(3): 347–356.
Meki, A.Z. and Mohey El-Deen. 1998. Serum interleukin-1B, IL-6. Nitric oxide and alpha1-antitrypsin in scorpion envenomed children. Toxicon 36: 1851–1859.
Hamdi-chérif, M., et al. 2009. Cancers liés au tabac dans la wilaya de Sétif (Algérie): incidence, tendance, survie et prévention 1986–2005. Revue d’Épidémiologie et de Santé Publique 57: S29.
Uchiyama, M., and M. Mihara. 1978. Determination of malonaldehyde precursor in tissues by thiobarbituric acid test. Analytical Biochemistry 86(1): 271–278.
Dhuley, J.N. 1998. Effect of ashwagandha on lipid peroxidation in stress-induced animals. Journal of Ethnopharmacology 60(2): 173–178.
Cho, S.-Y., et al. 2002. Alternation of hepatic antioxidant enzyme activities and lipid profile in streptozotocin-induced diabetic rats by supplementation of dandelion water extract. Clinica Chimica Acta 317(1): 109–117.
Adi-Bessalem, S., D. Hammoudi-Triki, and F. Laraba-Djebari. 2008. Pathophysiological effects of Androctonus australis hector scorpion venom: tissue damages and inflammatory response. Experimental and Toxicologic Pathology 60(4): 373–380.
Fatani, A., et al. 2006. Protective effects of the antioxidant Ginkgo biloba extract and the protease inhibitor aprotinin against Leiurus quinquestriatus venom-induced tissue damage in rats. Journal of Venomous Animals and Toxins including Tropical Diseases 12(2): 255–275.
Daisley, H., D. Alexander, and P. Pitt-Miller. 1999. Acute myocarditis following Tityus trinitatis envenoming: morphological and pathophysiological characteristics. Toxicon 37(1): 159–165.
Neumann, S., et al. 2007. The non-neuronal cholinergic system in peripheral blood cells: effects of nicotinic and muscarinic receptor antagonists on phagocytosis, respiratory burst and migration. Life Sciences 80(24): 2361–2364.
Whaley, K., D. Lappin, and T. Barkas. 1981. C2 synthesis by human monocytes is modulated by a nicotinic cholinergic receptor.
Mita, Y., et al. 1996. Induction of muscarinic receptor subtypes in monocytic/macrophagic cells differentiated from EoL-1 cells. European Journal of Pharmacology 297(1): 121–127.
Iho, S., et al. 2003. Nicotine induces human neutrophils to produce IL-8 through the generation of peroxynitrite and subsequent activation of NF-kB. Journal of Leukocyte Biology 74(5): 942–951.
Profita, M., et al. 2005. Muscarinic receptors, leukotriene B4 production and neutrophilic inflammation in COPD patients. Allergy 60(11): 1361–1369.
Saareks, V., et al. 1993. Nicotine and cotinine modulate eicosanoid production in human leukocytes and platelet rich plasma. European Journal of Pharmacology: Environmental Toxicology and Pharmacology 248(4): 345–349.
Wang, H., et al. 2004. Cholinergic agonists inhibit HMGB1 release and improve survival in experimental sepsis. Nature Medicine 10(11): 1216–1221.
Pavlov, V.A., and K.J. Tracey. 2005. The cholinergic anti-inflammatory pathway. Brain, Behavior, and Immunity 19(6): 493–499.
Koyama, S., S.I. Rennard, and R.A. Robbins. 1992. Acetylcholine stimulates bronchial epithelial cells to release neutrophil and monocyte chemotactic activity. American Journal of Physiology-Lung Cellular and Molecular Physiology 262(4): L466–L471.
Sato, E., et al. 1998. Acetylcholine stimulates alveolar macrophages to release inflammatory cell chemotactic activity. American Journal of Physiology-Lung Cellular and Molecular Physiology 274(6): L970–L979.
Aronstam, R. and P. Patil. 2009. Muscarinic receptors: autonomic neurons. Encyclopedia of neuroscience. 1141–1149. Oxford: 4th Academic Press.
Kavelaars, A., et al. 1997. β 2-Adrenergic activation enhances interleukin-8 production by human monocytes. Journal of Neuroimmunology 77(2): 211–216.
Ghazal, A., et al. 1975. Pharmacological studies of scorpion (Androctonus amoreuxi Aud. & Sav.) venom. Toxicon 13(4): 253–254.
Ismail, M., et al. 1980. Pharmacokinetics of 125 I-labelled venom from the scorpion Androctonus amoreuxi, Aud. and Sav. Toxicon 18(3): 301–308.
Azevedo, A., et al. 1983. Cardiovascular and respiratory effects induced by a purified scorpion toxin (tityustoxin) in unanesthetized rats. Toxicon 21(6): 753–759.
Amaral, C.F.S., et al. 1994. Scorpion sting-induced pulmonary oedema: evidence of increased alveolocapillary membrane permeability. Toxicon 32(8): 999–1003.
Zheng, M., et al. 2005. Emerging concepts and therapeutic implications of β-adrenergic receptor subtype signaling. Pharmacology & Therapeutics 108(3): 257–268.
Bernstein, D., G. Fajardo, and M. Zhao. 2011. The role of β-adrenergic receptors in heart failure: differential regulation of cardiotoxicity and cardioprotection. Progress in Pediatric Cardiology 31(1): 35–38.
Zhu, W.-Z., et al. 2003. Linkage of β1-adrenergic stimulation to apoptotic heart cell death through protein kinase A–independent activation of Ca2+/calmodulin kinase II. Journal of Clinical Investigation 111(5): 617.
Zhu, W., et al. 2005. The Enigma of β2-Adrenergic Receptor Gi Signaling in the Heart The Good, the Bad, and the Ugly. Circulation Research 97(6): 507–509.
Hoffmann, C., et al. 2004. Comparative pharmacology of human β-adrenergic receptor subtypes—characterization of stably transfected receptors in CHO cells. Naunyn-Schmiedeberg’s Archives of Pharmacology 369(2): 151–159.
Communal, C., et al. 1999. Opposing Effects of β1-and β2-Adrenergic Receptors on Cardiac Myocyte Apoptosis Role of a Pertussis Toxin–Sensitive G Protein. Circulation 100(22): 2210–2212.
Zhu, W.-Z., et al. 2001. Dual modulation of cell survival and cell death by β2-adrenergic signaling in adult mouse cardiac myocytes. Proceedings of the National Academy of Sciences 98(4): 1607–1612.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The experimental protocol was carried out according to the European Community rules of the Ethical Committee for Animal Welfare.
Rights and permissions
About this article
Cite this article
Nakib, I., Martin-Eauclaire, MF. & Laraba-Djebari, F. Involvement of Cholinergic and Adrenergic Receptors in Pathogenesis and Inflammatory Response Induced by Alpha-Neurotoxin Bot III of Scorpion Venom. Inflammation 39, 1670–1680 (2016). https://doi.org/10.1007/s10753-016-0401-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-016-0401-8