Abstract
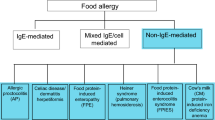
Food allergy, a commonly increasing problem worldwide, defined as an adverse immune response to food. A variety of immune-related effector cells such as mast cells, eosinophils, neutrophils, and T cells are involved in food-related allergic responses categorized as IgE mediated, non-IgE mediated, and mixed (IgE and non-IgE) depending upon underlying immunological mechanisms. The dietary antigens mainly target the gastrointestinal tract including pancreas that gets inflamed due to food allergy and leads acute pancreatitis. Reports indicate several food proteins induce pancreatitis; however, detailed underlying mechanism of food-induced pancreatitis is unexplored. The aim of the review is to understand and update the current scenario of food-induced pancreatitis. A comprehensive literature search of relevant research articles has been performed through PubMed, and articles were chosen based on their relevance to food allergen-mediated pancreatitis. Several cases in the literature indicate that acute pancreatitis has been provoked after the consumption of mustard, milk, egg, banana, fish, and kiwi fruits. Food-induced pancreatitis is an ignored and unexplored area of research. The review highlights the significance of food in the development of pancreatitis and draws the attention of physicians and scientists to consider food allergies as a possible cause for initiation of pancreatitis pathogenesis.

Similar content being viewed by others
References
Stone KD, Prussin C, Metcalfe DD. IgE, mast cells, basophils, and eosinophils. J Allergy Clin Immunol. 2010;125:S73–S80.
Shukla A, Mishra A, Venkateshaiah SU, Manhoar M, Mahadevappa CP, Mishra A. Elements involved in promoting eosinophilic gastrointestinal disorders. J Genet Syndr Gene Ther. 2015;6:265.
Verma AK, Manohar M, Venkateshaiah SU, Blecker U, Collins MH, Mishra A. Role of vasoactive intestinal peptide in promoting the pathogenesis of eosinophilic esophagitis (EoE). Cell Mol Gastroenterol Hepatol. 2017. doi:10.1016/j.jcmgh.2017.09.006.
Verma AK, Manohar M, Venkateshaiah SU, Mishra A. Endocrine cells derived chemokine vasoactive intestinal polypeptide (VIP) in allergic diseases. Cytokine Growth Factor Rev. 2017. doi:10.1016/j.cytogfr.2017.09.002.
Kattan J. The prevalence and natural history of food allergy. Curr Allergy Asthma Rep. 2016;16:47.
Żukiewicz-Sobczak WA, Wróblewska P, Adamczuk P, Kopczyński P. Causes, symptoms and prevention of food allergy. Postepy Dermatol Alergol. 2013;30:113–116.
Boden SR, Wesley Burks A. Anaphylaxis: a history with emphasis on food allergy. Immunol Rev. 2011;242:247–257.
Wolfe JL, Aceves SS. Gastrointestinal manifestations of food allergies. Pediatr Clin North Am. 2011;58:389–405.
Verma AK, Kumar S, Das M, Dwivedi PD. A comprehensive review of legume allergy. Clin Rev Allergy Immunol. 2013;45:30–46.
Inamura H, Kashiwase Y, Morioka J, Kurosawa M. Acute pancreatitis possibly caused by allergy to bananas. J Investig Allergol Clin Immunol. 2005;15:222–224.
Flejou JF, Potet F, Bernades P. Eosinophilic pancreatitis: a rare manifestation of digestive allergy? Gastroenterol Clin Biol. 1989;13:731–733.
Matteo A, Sarles H. Is food allergy a cause of acute pancreatitis? Pancreas. 1990;5:234–237.
de Diego Lorenzo A, Robles Fornieles J, Herrero López T, Cos Arregui E. Acute pancreatitis associated with milk allergy. Int J Pancreatol. 1992;12:319–321.
Iwata F, Odajima Y. Acute pancreatitis associated with food allergy. Eur J Pediatr. 1997;156:506.
Manohar M, Verma AK, Venkateshaiah SU, Sanders NL, Mishra A. Pathogenic mechanisms of pancreatitis. World J Gastrointest Pharmacol Ther. 2017;8:10–25.
Chowdhury P, Gupta P. Pathophysiology of alcoholic pancreatitis: an overview. World J Gastroenterol. 2006;12:7421–7427.
Manohar M, Verma A, Venkateshaiah SU, Sanders NL, Mishra A. Chronic pancreatitis associated acute respiratory failure. MOJ Immunol. 2017;5:1–7.
Yadav D, Lowenfels AB. The epidemiology of pancreatitis and pancreatic cancer. Gastroenterology. 2013;144:1252–1261.
Yang AL, Vadhavkar S, Singh G, Omary MB. Epidemiology of alcohol-related liver and pancreatic disease in the United States. Arch Intern Med. 2008;168:649–656.
Hirota M, Shimosegawa T, Masamune A, et al. The sixth nationwide epidemiological survey of chronic pancreatitis in Japan. Pancreatology. 2012;12:79–84.
Couvelaire R, Bargeton D. Quelques résultats expérimentaux sur la génèse des oedèmes aigus et des hémorragies pancréatiques. Les pancréatites anaphylactiques. CR Soc Biol. 1933;11:1435–1437.
Carrilllo T, Agustín M, Gusmán TM, Vilardell VU, Goiri IM. Pancreatitis aguda como complicación de anaphilaxia por mostaza. Rev Esp Alergol Immunol Clin. 1987;2:388–390.
Suzuki S, Homma T, Kurokawa M, et al. Eosinophilic gastroenteritis due to cow’s milk allergy presenting with acute pancreatitis. Int Arch Allergy Immunol. 2012;158:75–82.
Tse KY, Christiansen SC. Eosinophilic gastroenteritis due to egg allergy presenting as acute pancreatitis. Allergy Rhinol. 2015;6:80–81.
Pellegrino K, D’Urbano LE, Artesani MC, et al. Severe reaction in a child with asymptomatic codfish allergy: food challenge reactivating recurrent pancreatitis. Ital J Pediatr. 2012;38:16.
Gastaminza G, Bernaola G, Camino ME. Acute pancreatitis caused by allergy to kiwi fruit. Allergy. 1998;53:1104–1105.
Oskarsson V, Sadr-Azodi O, Orsini N, Andrén-Sandberg Å, Wolk A. High dietary glycemic load increases the risk of non-gallstone-related acute pancreatitis: a prospective cohort study. Clin Gastroenterol Hepatol. 2014;12:676–682.
Setiawan VW, Pandol SJ, Porcel J, et al. Dietary factors reduce risk of acute pancreatitis in a large multiethnic cohort. Clin Gastroenterol Hepatol. 2017;15:257e3–265e3.
Oskarsson V, Sadr-Azodi O, Orsini N, Andrén-Sandberg Å, Wolk A. Vegetables, fruit and risk of non-gallstone-related acute pancreatitis: a population-based prospective cohort study. Gut. 2013;62:1187–1192.
Oskarsson V, Orsini N, Sadr-Azodi O, Wolk A. Fish consumption and risk of non-gallstone-related acute pancreatitis: a prospective cohort study. Am J Clin Nutr. 2015;101:72–78.
Ho MH, Wong WH, Chang C. Clinical spectrum of food allergies: a comprehensive review. Clin Rev Allergy Immunol. 2014;46:225–240.
Beausoleil JL, Fiedler J, Spergel JM. Food intolerance and childhood asthma: what is the link? Paediatr Drugs. 2007;9:157–163.
Bihouee T, Bouchaud G, Chesne J, et al. Food allergy enhances allergic asthma in mice. Respir Res. 2014;15:142.
Brandt EB, Scribner TA, Akei HS, Rothenberg ME. Experimental gastrointestinal allergy enhances pulmonary responses to specific and unrelated allergens. J Allergy Clin Immunol. 2006;118:420–427.
Cho KA, Suh JW, Sohn JH, et al. IL-33 induces Th17-mediated airway inflammation via mast cells in ovalbumin-challenged mice. Am J Physiol Lung Cell Mol Physiol. 2012;302:L429–L440.
Bihouée T, Bouchaud G, Chesné J, et al. Food allergy enhances allergic asthma in mice. Respir Res. 2014;15:142.
Tariq SM, Matthews SM, Hakim EA, Arshad SH. Egg allergy in infancy predicts respiratory allergic disease by 4 years of age. Pediatr Allergy Immunol. 2000;11:162–167.
James JM, Bernhisel-Broadbent J, Sampson HA. Respiratory reactions provoked by double-blind food challenges in children. Am J Respir Crit Care Med. 1994;149:59–64.
Torpier G, Colombel JF, Mathieu-Chandelier C, et al. Eosinophilic gastroenteritis: ultrastructural evidence for a selective release of eosinophil major basic protein. Clin Exp Immunol. 1988;74:404–408.
Mishra A, Hogan SP, Lee JJ, Foster PS, Rothenberg ME. Fundamental signals that regulate eosinophil homing to the gastrointestinal tract. J Clin Invest. 1999;103:1719–1727.
Uppal V, Kreiger P, Kutsch E. Eosinophilic gastroenteritis and colitis: a comprehensive review. Clin Rev Allergy Immunol. 2016;50:175–188.
Khan S, Orenstein SR. Eosinophilic gastroenteritis: epidemiology, diagnosis and management. Paediatr Drugs. 2002;4:563–570.
Alfadda AA, Storr MA, Shaffer EA. Eosinophilic colitis: epidemiology, clinical features, and current management. Ther Adv Gastroenterol. 2011;4:301–309.
Jaffe JS, James SP, Mullins GE, Braun-Elwert L, Lubensky I, Metcalfe DD. Evidence for an abnormal profile of interleukin-4 (IL-4), IL-5, and gamma-interferon (gamma-IFN) in peripheral blood T cells from patients with allergic eosinophilic gastroenteritis. J Clin Immunol. 1994;14:299–309.
el Mouzan MI, al Quorain AA, Anim JT. Cow’s-milk-induced erosive gastritis in an infant. J Pediatr Gastroenterol Nutr. 1990;10:111–113.
Bischoff SC. Food allergy and eosinophilic gastroenteritis and colitis. Curr Opin Allergy Clin Immunol. 2010;10:238–245.
Valle-Dorado MG, Santana-Gómez CE, Orozco-Suárez SA, Rocha L. The mast cell stabilizer sodium cromoglycate reduces histamine release and status epilepticus-induced neuronal damage in the rat hippocampus. Neuropharmacology. 2015;92:49–55.
Vazquez Rodriguez JJ, Soleto Sáez E, Sánchez Vega J, López Serrano MC, Cerdán Vallejo A. Pancreatitis and eosinophilic gastroenteritis. Int Surg. 1973;58:415–419.
Caglar E, Karismaz K, Dobrucali A. A case of eosinophilic gastroenteritis mimicking gastric lymphoma associated with pancreatitis due to duodenal involvement. Turk J Gastroenterol. 2012;23:585–589.
Goyal H, Smith B, Bayer C, Rutherford C, Shelnut D. Differences in severity and outcomes between hypertriglyceridemia and alcohol-induced pancreatitis. N Am J Med Sci. 2016;8:82–87.
Braganza JM, Dormandy TL. Micronutrient therapy for chronic pancreatitis: rationale and impact. JOP. 2010;11:99–112.
Esposito I, Friess H, Kappeler A, et al. Mast cell distribution and activation in chronic pancreatitis. Hum Pathol. 2001;32:1174–1183.
Kweon MN, Yamamoto M, Kajiki M, Takahashi I, Kiyono H. Systemically derived large intestinal CD4(+) Th2 cells play a central role in STAT6-mediated allergic diarrhea. J Clin Invest. 2000;106:199–206.
Metcalfe DD, Peavy RD, Gilfillan AM. Mechanisms of mast cell signaling in anaphylaxis. J Allergy Clin Immunol. 2009;124:639–646 (quiz 647–8).
Knol EF. Requirements for effective IgE cross-linking on mast cells and basophils. Mol Nutr Food Res. 2006;50:620–624.
Raithel M, Dormann H, Harsch IA, et al. Immunoglobulin E production in chronic pancreatitis. Eur J Gastroenterol Hepatol. 2003;15:801–807.
Raithel M, Dormann H, Farnbacher M, Weidenhiller M, Hahn EG, Schneider HT. Stimulation of immunoglobulin E formation in chronic pancreatitis by alcohol drinking and exocrine pancreatic insufficiency. Z Gastroenterol. 2001;39:269–276.
Jyonouchi H. Non-IgE mediated food allergy—update of recent progress in mucosal immunity. Inflamm Allergy Drug Targets. 2012;11:382–396.
Caubet JC, Szajewska H, Shamir R, Nowak-Węgrzyn A. Non IgE-mediated gastrointestinal food allergies in children. Pediatr Allergy Immunol. 2017;28:6–17. doi:10.1111/pai.12659.
Tian L, Fu P, Dong X, Qi J, Zhu H. Eosinophilic pancreatitis: three case reports and literature review. Mol Clin Oncol. 2016;4:559–562.
Kumar S, Verma A, Das M, Dwivedi PD. Allergenic diversity among plant and animal food proteins. Food Rev Int. 2011;28:277–298.
Manohar M, Verma A, Venkateshaiah SU, Mishra A. Immunological responses involved in promoting acute and chronic pancreatitis. J Clin Immunol Res. 2017;1:1–8.
Wouters MM, Vicario M, Santos J. The role of mast cells in functional GI disorders. Gut. 2016;65:155–168.
Galli SJ, Grimbaldeston M, Tsai M. Immunomodulatory mast cells: negative, as well as positive, regulators of immunity. Nat Rev Immunol. 2008;8:478–486.
Kraneveld AD, Sagar S, Garssen J, Folkerts G. The two faces of mast cells in food allergy and allergic asthma: the possible concept of Yin Yang. Biochim Biophys Acta. 2012;1822:93–99.
Braganza JM. Mast cell: pivotal player in lethal acute pancreatitis. QJM. 2000;93:469–476.
Hoogerwerf WA, Gondesen K, Xiao SY, Winston JH, Willis WD, Pasricha PJ. The role of mast cells in the pathogenesis of pain in chronic pancreatitis. BMC Gastroenterol. 2005;5:8.
Dib M, Zhao X, Wang XD, Andersson R. Role of mast cells in the development of pancreatitis-induced multiple organ dysfunction. Br J Surg. 2002;89:172–178.
Masato Y, Uchida K, Ikemune M, et al. The role of basophil via TLR signaling in patients with type 1 autoimmune pancreatitis. Pancreatology. 2016;16:S40.
Stellato C, Collins P, Ponath PD, et al. Production of the novel C-C chemokine MCP-4 by airway cells and comparison of its biological activity to other C-C chemokines. J Clin Invest. 1997;99:926–936.
Maeshima A, Murakami H, Sadakata H, et al. Eosinophilic gastroenteritis presenting with acute pancreatitis. J Med. 1997;28:265–272.
Manohar M, Verma AK, Venkateshaiah SU, Mishra A. Role of eosinophils in the initiation and progression of pancreatitis pathogenesis. Am J Physiol Gastrointest Liver Physiol. 2017. doi:10.1152/ajpgi.00210.2017.
Wallaert B, Gosset P, Lamblin C, Garcia G, Perez T, Tonnel AB. Airway neutrophil inflammation in nonasthmatic patients with food allergy. Allergy. 2002;57:405–410.
Merza M, Hartman H, Rahman M, et al. Neutrophil extracellular traps induce trypsin activation, inflammation, and tissue damage in mice with severe acute pancreatitis. Gastroenterology. 2015;149:1920e8–1931e8.
Yang ZW, Meng XX, Xu P. Central role of neutrophil in the pathogenesis of severe acute pancreatitis. J Cell Mol Med. 2015;19:2513–2520
Munoz-Cano R, Picado C, Valero A, Bartra J. Mechanisms of anaphylaxis beyond IgE. J Investig Allergol Clin Immunol. 2016;26:73–82 (quiz 2p following 83).
Hahn J, Knopf J, Maueröder C, Kienhöfer D, Leppkes M, Herrmann M. Neutrophils and neutrophil extracellular traps orchestrate initiation and resolution of inflammation. Clin Exp Rheumatol. 2016;34:6–8.
Demols A, Le Moine O, Desalle F, Quertinmont E, Van Laethem JL, Devière J. CD4(+)T cells play an important role in acute experimental pancreatitis in mice. Gastroenterology. 2000;118:582–590.
Vonlaufen A, Apte MV, Imhof BA, Frossard JL. The role of inflammatory and parenchymal cells in acute pancreatitis. J Pathol. 2007;213:239–248.
Yamada T, Hashimoto T, Sogawa M, et al. Role of T cells in development of chronic pancreatitis in male Wistar Bonn/Kobori rats: effects of tacrolimus. Am J Physiol Gastrointest Liver Physiol. 2001;281:G1397–G1404.
Frossard JL, Kwak B, Chanson M, Morel P, Hadengue A, Mach F. Cd40 ligand-deficient mice are protected against cerulein-induced acute pancreatitis and pancreatitis-associated lung injury. Gastroenterology. 2001;121:184–194.
Palomares O. The role of regulatory T cells in IgE-mediated food allergy. J Investig Allergol Clin Immunol. 2013;23:371–382 (quiz 2 p preceding 382).
Eigenmann PA, Frossard CP. The T lymphocyte in food-allergy disorders. Curr Opin Allergy Clin Immunol. 2003;3:199–203.
Acknowledgments
Dr. Mishra is the Endowed Schlieder Chair; therefore, authors thank Edward G. Schlieder Educational Foundation for the support.
Funding
Funding was provided by National Institutes of Health (R01 AI080581).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Manohar, M., Verma, A.K., Upparahalli Venkateshaiah, S. et al. Food-Induced Acute Pancreatitis. Dig Dis Sci 62, 3287–3297 (2017). https://doi.org/10.1007/s10620-017-4817-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-017-4817-2