Abstract
Background
The incidence of gastric cancer varies both within and among populations and can change rapidly without a corresponding decline in Helicobacter pylori prevalence. Here, we describe the changes in gastric cancer mortality in Japan in relation to age-period-cohort effects as well as the decline in H. pylori prevalence.
Methods
We used data from Japanese for men and women aged 30–94 for birth years 1875–1970 (calendar time 1950–2000) to observe the age, period and cohort effects on gastric cancer mortality rates. Additionally, we used Poisson regression to simultaneously adjust for concurrent age, period and cohort effects as well as for declining H. pylori prevalence in the Japanese population.
Results
There was an approximate 60 % decline in gastric cancer mortality between 1965 and 1995. Detailed age, period and cohort analyses and Poisson regression analysis showed these factors interact in complex ways, analyses focused on one or two of these effects, such as birth cohort without considering concurrent age and period would obscure important interactions that affected different age groups at different times to produce this composite effect.
Conclusion
The underlying complexity in population–disease dynamics requires population-specific descriptions of trends using multiple methods to provide an in-depth analysis while simultaneously allowing for necessary statistical adjustments as well as identification of interactions. More thorough descriptions of the population-specific general trends in relation to changes in the population structure (age-period-cohort) enable better prevention and health care policy planning, and further, the descriptions enable hypothesis generation regarding causes of population-specific disease patterns.
Similar content being viewed by others
Introduction
Gastric cancer is one of the long-term complications of gastric inflammation caused by chronic Helicobacter pylori infection [1–3]. The prevalence of H. pylori infection in many Western societies has been on the decline in part as a result of a marked decrease in acquisition of the infection in childhood [4].
Based on investigations of H. pylori and gastric cancer simultaneously over time, researchers have reported that generally, both gastric cancer mortality rate and H. pylori prevalence increase with age, decrease across time, and decrease with more recent birth years [5–10]. However, others have reported various patterns of H. pylori and gastric cancer that do not correspond to the general knowledge. For instance, many have observed populations in which H. pylori infection prevalence is 50 % and above in adults but gastric cancer is rare suggesting complexity in the relationship between H. pylori infection and its associated diseases [11–14]. Part of the complexity can be explained by three-way (host–bacteria–environment) interactions that govern the clinical manifestations of H. pylori infections [1]. For example, H. pylori infection primarily results in a non-atrophic pattern of gastritis associated with duodenal ulcer disease and rarely gastric cancer among individuals living in regions where fresh fruits and vegetables are available year around (i.e., Southern India or Thailand) [15]. In contrast, in regions where diets are seasonal and salt is the primary method to preserve food, infection results in rapid acquisition of atrophic gastritis and gastric cancer [15–17].
The observed heterogeneity is even more complex since the three-way, host–bacterial–environment interactions vary by population and can change rapidly over time (e.g., changes in sociopolitical structures and economic development could affect changes in the population structure such as birth rates, life expectancy, and simultaneously affect changes in sanitation, transportation and thus access to fresh vegetables and to medical care [5]. These multilevel interactions may produce unexpected trends of H. pylori and its associated diseases and emphasize the need for examining population-specific trends of both H. pylori and gastric cancer mortality while simultaneously accounting for the effects of age, period (calendar time) and birth year (cohort). Careful age, period and cohort analyses are required to describe changes in gastric cancer mortality rates across time in response to changes in H. pylori prevalence, especially since it is exceedingly difficult to tease apart correlated age-period-cohort trends in the presence of confounding by age and changes in population structure.
Even if investigators use age-adjusted, sex-adjusted and population-standardized gastric cancer mortality rates, one can only examine two of the three age-period-cohort trends at a time. Few studies have used Poisson regression to model gastric cancer mortality rates while simultaneously adjusting for all three age-period-cohort effects. To our knowledge, no study has examined gastric cancer mortality rates while adjusting for joint age-period-cohort effects as well as the contributing effects of H. pylori prevalence over time in a population.
We sought to describe age-period-cohort effects as well as declining H. pylori prevalence on gastric cancer mortality in Japan, a population setting with very complex trends of H. pylori and gastric cancer in that it has (1) one of the highest gastric cancer mortality rates in the world, (2) rapidly falling prevalence of H. pylori due to low acquisition rates in children, (3) declining gastric cancer incidence in all ages regardless of H. pylori infection, and (4) among older Japanese, gastric cancer has declined while H. pylori prevalence has remained high [8, 9, 18, 19].
We used data from the Japanese population for birth years 1875–1970, over calendar time 1950–2000, for men and women aged 30–94. Additionally, we used Poisson regression to simultaneously adjust for concurrent age-period-cohort effects in order to observe the effects of declining H. pylori prevalence (between 27 and 88 %) over this period on gastric cancer mortality rates in Japan.
Materials and Methods
The Japanese Population and Gastric Cancer Mortality Rates in Japan
Counts of the Japanese population from years 1920 to 2004 by sex and by 5-year age intervals were obtained from the Japanese Population Census and the Annual Report on Current Population Estimates [20]. Gastric cancer mortality rates in Japan from years 1950–2000 by sex and by 5-year age categories were obtained from "Cancer Statistics in Japan" reports published by the Cancer Information Services and Surveillance Division within the National Cancer Center Research Institute of Japan [20]. All data were publicly available. All gastric cancer mortality rates were standardized by age and sex to the 2000 Japanese population structure using direct standardization.
Helicobacter pylori Prevalence in Japan
We used published reports on the prevalence of H. pylori at age 20 in Japan and projected H. pylori prevalence across calendar time [21]. The published data fit a linear model of decline; thereby, we used a linear spline to impute the H. pylori prevalence at age 20 in Japan from 1895 to 1990, in 5-year time increments. Since H. pylori is most likely acquired in childhood and that prevalence increases with age and peaks at about age 20, and infection remains chronic thereafter, we assumed that the prevalence of H. pylori remains stable after age 20 at the population level for each 5-year birth cohort.
Age-Period-Cohort Trend Graphs for Gastric Cancer Mortality in Japan
To observe the age-period-cohort trends, we created sex-stratified age-period, age-cohort, and period-cohort graphs using sex-specific, age-specific, and age-adjusted standardized gastric cancer mortality rates across calendar years 1950–2000, for birth cohort years 1875–1970, and for age categories 30–34 through 90–94, where appropriate.
Poisson Regression
We used Poisson regression to obtain unadjusted and adjusted mortality rate ratios (incidence rate ratios) for gastric cancer deaths stratified by sex. Analyses were restricted to birth cohorts for whom we had more than three mortality rates for each age category across time. Although some adjacent categories could have been collapsed to present the trends, we retained 5-year age and time categories to present detailed incidence rate ratios and to facilitate discussion of summary trends. In adjusted models where both age and birth cohort year cannot be included due to collinearity, age was retained in the model since the magnitude of age effects far exceeded the effect sizes of birth cohort years. The choice of reference categories drives the resulting ratio measures and can sometimes be arbitrary. In this paper, we chose the reference categories to reflect an inflection point of the ratio curve, if there was one. For example, we chose the reference category for H. pylori prevalence at 70 % since there was a change in the slope of the rate ratios at that point [22, 23].
Results
H. pylori Prevalence
We constructed H. pylori prevalence at age 20 across calendar time in Japan using published data and linear spline (Table 1): Prevalence estimates of >80 % for calendar years 1895–1934; between 80 and 70 % for years 1935–1959; between <70 and 60 % for years 1960–1974; between <60 and 30 % for years 1975–1989; and 27 % for years 1990–1994. Spline nodes were at years 1910 and 1950, with corresponding prevalence of 80 and 60 %, respectively.
Age-Period-Cohort Trends for Gastric Cancer Mortality in Japan
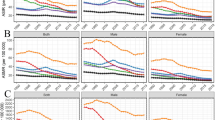
We observed the expected overall trends in gastric cancer mortality rates in the Japanese population (sex-specific age-period-cohort graphs, Figs. 1, 2a–b, 3a–b, 4a–b): an increase with age; a decrease across calendar time, and a decrease with younger birth cohorts. However, we find interactions between the various time effects that we describe next for each pairwise combination. Although women had approximately half of the gastric cancer mortality rates as men across all ages and time, they experienced very similar trends in gastric cancer mortality rates.
a Age-Period Graph: Age-specific gastric cancer mortality rates by age category and period in Japanese men, ages 30–94, years 1950–2000. b Age-Period Graph: Age-specific gastric cancer mortality rates by age category and period in Japanese women, ages 30–94, years 1950–2000. Mortality rates standardized to Japanese 2000 Census population structure by age using direct standardization
a. Age-Cohort Graph: Age-specific gastric cancer mortality rates by age and birth cohort in Japanese men, ages 30–94, birth years 1875–1970. b Age-specific gastric cancer mortality rates by age and birth cohort in Japanese women, ages 30–94, birth years 1875–1970. Mortality rates standardized to the Japanese 2000 Census population structure by age using direct standardization
a Period-Cohort Graphs: Age-specific gastric cancer mortality rates by period and birth cohort in Japanese men, years 1950–2000, birth years 1875–1970. b Age-specific gastric cancer mortality rates by period and birth cohort in Japanese women, years 1950–2000, birth years 1875–1970. Mortality rates standardized to the Japanese 2000 Census population structure by age using direct standardization
Age-Period Trends
Although there is an overall secular trend (period effect) of gastric cancer mortality rates, there is an interaction between age and period, where mortality rates across time differs by age category (Fig. 2a, b). Specifically, we identify three different trends of gastric cancer mortality rates over time across age categories: (1) Age 85–89 and 90–94, where mortality rates increase over time; (2) Age 65–69 through 80–85, where mortality rates increase and then decrease, with different slopes and different times at which changes in slopes occurred; and (3) Age 30–34 through 60–65, where mortality rates decreases over time with different slopes of decline.
Age-Cohort Trends
Figure 3a, b demonstrates a strong age effect on gastric cancer mortality rates that differs by birth year. For any given age category under 75–79, gastric cancer mortality rates decrease significantly with increasing birth year. For instance, among men aged 60–64, gastric cancer mortality rates decreased from 325/100,000 for those born in 1890 to 92/100,000 for those born in 1940. Similar relative declines were also observed for women: among women aged 60–64, gastric cancer mortality rates decreased from 158/100,000 for those born in 1890 to 33/100,000 for those born in 1940. Across age, there were similar declines in gastric cancer mortality rates (all about 75 % decline), except for the oldest age categories. Gastric cancer mortality rates among men and women in the oldest age categories either increased or declined less over increasing birth years; this could be due to differences in life expectancy as well as other competing causes of death.
Period-Cohort Trends
Similarly to the age-period trends, we show that there is an interaction between period and birth cohort, such that gastric cancer mortality rates across calendar time differ by birth cohort year (Fig. 4a, b). Here again, we identified three general trends by birth cohort from the period 1950–2000: (1) men and women born prior to 1905 had an increase and then a decrease in age-adjusted gastric cancer mortality rates across time; (2) those born between 1905 and 1935 had increases (with different slopes) across time; and (3) those born in 1940 and thereafter had slight increases to flat gastric cancer mortality rates across time.
Poisson Regression
The Effect of Age
Gastric cancer mortality rates in Japan are statistically significantly different by age and sex, even after adjusting for birth cohort year, calendar time and H. pylori prevalence at age 20 in the population over time (Table 2). In general, compared to men and women aged 30–34, those in progressively older age categories had higher gastric cancer mortality rates (men: 1.6–12 times higher; women: 1.4–4.9 times higher; p < 0.000). Men aged 65–74 had gastric cancer mortality rates 12 times higher than men aged 30–34 (p < 0.000). Women aged 65–69 and 70–74 had gastric cancer mortality rates 4.4 and 4.9 times higher, respectively, than women aged 30–34 (p < 0.000).
The Effect of Calendar Time
After adjusting for age, birth cohort year and H. pylori prevalence at age 20 in the population over time, we observed a statistically significant secular trend (period effect) in gastric cancer mortality rates in Japan (p < 0.000). Compared to gastric cancer mortality rates in years 1950–1954, there were progressive declines in rates among men every 5 years (men: rate ratios 0.96, 0.91, 0.87, 0.85, 0.82, starting with years 1965–1969). The declines in women were less in magnitude over the same period of time (Table 2).
The Effect of Birth Cohort Year
Compared to men born in years 1940–1944, men born prior to 1940 had 1.6–3.4 times higher gastric cancer mortality rates after adjusting for age, calendar time and H. pylori prevalence at age 20 over time. Men born in or after 1945 had much lower mortality rates (rate ratios 0.69–0.73) compared to those born in 1940–1944. From similarly adjusted models, we observed that women born prior to 1940 had 1.2–2.5 higher gastric cancer mortality rates than women born in 1940–1944. Women born in or after 1945 had slightly lower mortality rates (rate ratios 0.84–1.0) than those born in 1940–1944; the magnitudes of these decreases over time for increasing birth years are less than those among men.
The Effect of Population H. pylori Prevalence at Age 20
Compared to a population H. pylori prevalence of 70 %, a progressively higher prevalence is associated with higher gastric cancer mortality rates, after adjustments for age and calendar time. The gastric cancer mortality rates were 3.7 times higher among men and 2.7–2.8 times higher among women for population prevalence of 83–84 % compared to the reference prevalence of 70 % (Table 2). There was a strong inverse association between H. pylori prevalence and gastric cancer mortality rates for population prevalences between 50 and 70 % (e.g., rate ratios among men: 0.59, 0.38, 0.24, 0.11 for prevalences 68, 66, 61, 52 %, respectively); the association was an order of magnitude stronger for population prevalences below 50 % (e.g., rate ratios among men: 0.045, 0.021, 0.012 for prevalences 44, 36, and 27 %, respectively).
Discussion
Based on published reports, the established trends are as follows: Gastric cancer mortality rates in Japan (1) increase with age, (2) decrease across calendar time, and (3) decrease with progressively more recent birth years [6–10]. We show that these trends are oversimplified. We provide a more nuanced story using age-period-cohort analyses that captures important interactions of age/birth cohort with calendar time, as well as using Poisson regression, which enabled examinations of gastric cancer mortality rates while adjusting for age, period and cohort effects and for the effect of declining H. pylori prevalence. Below, we discuss our results in context of the established trends.
We observed that the effect of age on gastric cancer mortality (regression results, Table 2) is in keeping with the established trend and with our understanding of cancer in general (i.e., gastric cancer mortality rate goes up as we age, even when we condition on birth cohort, calendar time, and prevalence of H. pylori). The age-cohort graphs (Fig. 3a, b) show an interaction between age and birth cohort, such that the evidence for competing causes at older ages is strongest for the oldest cohorts.
It is well established that gastric cancer mortality has generally decreased across calendar time. We show that this decrease is an averaged age effect. We found that the decrease in mortality rate over time varies by age group: Mortality increases across time in the oldest groups; mortality increases then decreases with mid-age groups; and mortality decreases with different slopes for the youngest groups. For example, if we look at the general time trend, we find an approximately 60 % decline in gastric cancer mortality rates in Japan in all age groups from calendar year 1965–1995 (Fig. 1). However, we show that the decreases in rates were completely different across three broad age categories (>85, ages 65–85, age <65; i.e., the curves have very different slopes, see age-period graphs Fig. 2a, b). Thus, the decline actually reflects an average period effect across all age categories and birth cohorts and obscures the fact that, as shown in the graphs, there is an interaction between period and age/cohort. In the regressions model, we show that the decline of gastric cancer mortality over calendar time was only moderate, part of which is likely due to the regression model representing an average secular trend (or, period effect) across all ages and birth cohorts. As we demonstrated in both the age-period and period-cohort graphs (Figs. 2a, b, 4a, b, respectively), there is clear evidence of an interaction of calendar time with either age or cohort.
Based on published reports, we expected to find dramatic declines in gastric cancer mortality among more recent birth cohorts, for example, among those born after World War II reconstruction years in Japan. However, contrary to the established knowledge, we show that mortality rates with respect to birth cohorts mostly increases or is flat across calendar time. For cohorts born before 1905, mortality increases then decreases over time; for cohorts born between 1905 and 1935 the mortality increases—an age effect; and for cohorts born in and after 1940, the mortality rate is mostly flat (Fig. 4a, b). The regressions (the effect of birth cohort on gastric cancer mortality, Table 2) show similar results, and gastric cancer mortality rate was declining from the early 1900s until the mid-1940s and then flattened out. Japanese men and women born from 1945 onward appear to have comparable gastric cancer mortality rates, conditional on age, calendar period, and prevalence of H. pylori.
Taken together, we show evidence that the oldest age groups did not and cannot benefit from better health care and changes in diet experienced by younger generations. Gastric cancer risk is directly related to the extent and severity of atrophic gastritis [1]. For individuals in the earliest birth cohorts or the oldest age categories, extensive atrophic changes may have already been in place prior to availability of better health care or diet, whereas changes in diet and food preservation have resulted in a progressive decline in the velocity of development of atrophic changes [5, 15–17].
While it is useful to begin investigations with general population trends, researchers benefit from paying special attention when reports emerge with contradictory findings, since this phenomenon reflects underlying complexity in population–disease dynamics. In these situations, population-specific descriptions of trends using multiple methods are needed to provide a more in-depth analysis while allowing for necessary statistical adjustments as well as identification of interactions. More thorough descriptions of the population-specific trends in relation to changes in the population structure (age-period-cohort), as well as other factors, enable better prevention and health care policy planning, and further, the descriptions enable hypothesis generation regarding causes of population-specific disease patterns.
Japan broke from its feudal past in 1868 followed by attempts to establish a new political structure and to modernize the country [24]. By the mid-1970s, good sanitation and clean water were available countrywide [25]. Recently, the incidence of H. pylori infection fell rapidly in the younger subpopulations, and this trend has accelerated to where currently, H. pylori infections are rare among those under age 20 [26, 27]. Other contributing factors include progressive improvements in sanitation, diet, and food preservation, including refrigeration and year-round availability of fresh fruits and vegetables [18, 28, 29]. Improved standards of living and sanitation reduced H. pylori acquisition in children, whereas dietary changes reduced the rate of acquisition of atrophic gastritis, together leading to decreased gastric cancer.
References
Shiotani A, Cen P, Graham DY. Eradication of gastric cancer is now both possible and practical. Semin Cancer Biol. 2013;23:492–501.
Helicobacter pylori. In: Bouvard V, Baan R, Straif K, Grosse Y, Secretan B, el Ghissassi F, Benhrahim-Taliaa L, Guha N, Freeman C, Galiehet L, and Cogliano V (eds.) Biologic agents: a review of human carcinogens, vol 100B. Leon: International Agency for Research on Cancer; 2012. p. 385–435.
IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. Volume 61: Schistosomes, liver flukes and Helicobacter pylori. Lyon, France: International Agency for Research on Cancer, 1994.
Tonkic A, Tonkic M, Lehours P, Megraud F. Epidemiology and diagnosis of Helicobacter pylori infection. Helicobacter. 2012;17(Suppl 1):1–8.
Graham DY. History of Helicobacter pylori related diseases: duodenal ulcer, gastric ulcer, and gastric cancer. World J Gastroenterol. 2014;14:5191–5204.
Sonnenberg A. Differences in the birth-cohort patterns of gastric cancer and peptic ulcer. Gut. 2010;59:736–743.
Watanabe S, Tsugane S, Ohno Y. Prediction of the gastric cancer mortality in 2000 in Japan. Jpn J Cancer Res. 1988;79:439–444.
Bertuccio P, Chatenoud L, Levi F, et al. Recent patterns in gastric cancer: a global overview. Int J Cancer. 2009;125:666–673.
Inoue M, Tsugane S. Epidemiology of gastric cancer in Japan. Postgrad Med J. 2005;81:419–424.
Kamo K, Sobue T. Cancer statistics digest. Mortality trend of prostate, breast, uterus, ovary, bladder and “kidney and other urinary tract” cancer in Japan by birth cohort. Jpn J Clin Oncol. 2004;34:561–563.
Agha A, Graham DY. Evidence-based examination of the African enigma in relation to Helicobacter pylori infection. Scand J Gastroenterol. 2005;40:523–529.
Graham DY, Lu H, Yamaoka Y. African, Asian or Indian enigma, the East Asian Helicobacter pylori: facts or medical myths. J Dig Dis. 2009;10:77–84.
Ghoshal UC, Tripathi S, Ghoshal U. The Indian enigma of frequent H. pylori infection but infrequent gastric cancer: Is the magic key in Indian diet, host’s genetic make up, or friendly bug? Am J Gastroenterol. 2007;102:2113–2114.
Singh K, Ghoshal UC. Causal role of Helicobacter pylori infection in gastric cancer: an Asian enigma. World J Gastroenterol. 2006;12:1346–1351.
Graham DY. Helicobacter pylori infection in the pathogenesis of duodenal ulcer and gastric cancer: a model. Gastroenterology. 1997;113:1983–1991.
Park B, Shin A, Park SK, et al. Ecological study for refrigerator use, salt, vegetable, and fruit intakes, and gastric cancer. Cancer Causes Control. 2011;22:1497–1502.
Shikata K, Kiyohara Y, Kubo M, et al. A prospective study of dietary salt intake and gastric cancer incidence in a defined Japanese population: the Hisayama study. Int J Cancer. 2006;119:196–201.
Matsuzaka M, Fukuda S, Takahashi I, et al. The decreasing burden of gastric cancer in Japan. Tohoku J Exp Med. 2007;212:207–219.
Sasaki J, Akai S. Role of diagnostic and therapeutic improvements in the decline of gastric cancer mortality rate in Japan. Jpn J Cancer Res. 1985;76:149–153.
Cancer Control and Information Services, National Cancer Center for Cancer Control and Information Services. http://ganjoho.jp/professional/statistics/statistics.html. Last assessed 3/31/2014
Asaka M, Kimura T, Kudo M, et al. Relationship of Helicobacter pylori to serum pepsinogens in an asymptomatic Japanese population. Gastroenterology. 1992;102:760–766.
Rothman KJ, Greenland S, Lash TL. Modern epidemiology. Philadelphia: Lippincott, Williams & Wilkins; 2008.
Rothman KJ, Greenland S. Modern epidemiology. Philadelphia: Lippencott-Raven Publishers; 1998.
McClain JL. Japan, a modern history. New York: WW Norton & Company; 2003.
Population served by water supply as percent of total population. http://www.mhlw.go.jp/stf/seisakunitsuite/bunya/topics/bukyoku/kenkou/suido/database/kihon/suii.html Last assessed 3/31/2014.
Naito Y, Shimizu T, Haruna H, et al. Changes in the presence of urine Helicobacter pylori antibody in Japanese children in three different age groups. Pediatr Int. 2008;50:291–294.
Malaty HM, Tanaka E, Kumagai T, et al. Seroepidemiology of Helicobacter pylori and hepatitis A virus and the mode of transmission of infection: a 9-year cohort study in rural Japan. Clin Infect Dis. 2003;37:1067–1072.
Takachi R, Inoue M, Ishihara J, et al. Fruit and vegetable intake and risk of total cancer and cardiovascular disease: Japan Public Health Center-Based Prospective Study. Am J Epidemiol. 2008;167:59–70.
Shimazu T, Wakai K, Tamakoshi A, et al. Association of vegetable and fruit intake with gastric cancer risk among Japanese: a pooled analysis of four cohort studies. Ann Oncol. 2014;. doi:10.1093/annonc/mdu115.
Acknowledgments
The authors thank Dr. Akiko Shiotani for assistance in obtaining the data regarding the incidence of gastric cancer in Japan. Dr. Graham is supported in part by the Office of Research and Development Medical Research Service Department of Veterans Affairs, Public Health Service Grants R01 DK062813 and DK56338 which funds the Texas Medical Center Digestive Diseases Center. The contents are solely the responsibility of the authors and do not necessarily represent the official views of the VA or NIH.
Conflict of interest
Dr. Graham is a unpaid consultant for Novartis in relation to vaccine development for treatment or prevention of H. pylori infection. Dr. Graham is a paid consultant for RedHill Biopharma regarding novel H. pylori therapies and has received research support for culture of Helicobacter pylori. He is a consultant for Otsuka Pharmaceuticals regarding diagnostic breath testing. Dr. Graham has received royalties from Baylor College of Medicine patents covering materials related to 13C-urea breath test. Drs. Wang and Weber declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, C., Weber, A. & Graham, D.Y. Age, Period, and Cohort Effects on Gastric Cancer Mortality. Dig Dis Sci 60, 514–523 (2015). https://doi.org/10.1007/s10620-014-3359-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-014-3359-0