Abstract
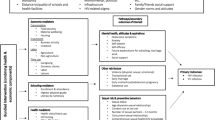
Little work has examined how individuals’ social affiliations—the venues in which they meet friends and engage in informal social interaction—influence their engagement with public health services. We investigate how links to these local places shape access to information and exposure to health-seeking behavior. Using longitudinal data from a respondent-driven sample of 618 young black men who have sex with men (YBMSM) in Chicago, we identify different sets of social venues that connect YBMSM. We then examine how YBMSM’s connections within this network influence their receipt of HIV prevention and treatment services and knowledge of pre-exposure prophylaxis (PrEP). Our results show that YBMSM’s positions within Chicago’s venue network shape the types of health-related services they access, net of demographic, structural, and community covariates. Men with affiliations that are linked to the city’s gay enclave are most likely to know about PrEP, while men with affiliations that are predominately in the black community demonstrate improved HIV treatment outcomes. Outreach engaging MSM beyond venues in gay enclaves is needed.


Similar content being viewed by others
References
Centers for Disease Control and Prevention. Lifetime risk of HIV diagnosis. NCHHSTP. 2016. http://www.cdc.gov/nchhstp/newsroom/2016/croi-press-release-risk.html. Accessed 5 June 2016.
Millett GA, Peterson JL, Flores SA, et al. Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: a meta-analysis. Lancet. 2012;380(9839):341–8.
Levy ME, Wilton L, Phillips G, et al. Understanding structural barriers to accessing HIV testing and prevention services among black men who have sex with men (BMSM) in the United States. AIDS Behav. 2014;18(5):972–96. doi:10.1007/s10461-014-0719-x.
Pierce SJ, Miller RL, Morales MM, Forney J. Identifying HIV prevention service needs of African American men who have sex with men: an application of spatial analysis techniques to service planning. J Public Health Manag Pract. 2007;13(1):S72–9.
Scott HM, Pollack L, Rebchook GM, Huebner DM, Peterson J, Kegeles SM. Peer social support is associated with recent HIV testing among young black men who have sex with men. AIDS Behav. 2014;18(5):913–20. doi:10.1007/s10461-013-0608-8.
Zinski A, Westfall AO, Gardner LI, et al. The contribution of missed clinic visits to disparities in HIV viral load outcomes. Am J Public Health. 2015;105(10):2068–75. doi:10.2105/AJPH.2015.302695.
Attia S, Egger M, Muller M, Zwahlen M, Low N. Sexual transmission of HIV according to viral load and antiretroviral therapy: systematic review and meta-analysis. AIDS. 2009;23(11):1397–14044.
Millett GA, Peterson JL, Wolitski RJ, Stall R. Greater risk for HIV infection of black men who have sex with men: a critical literature review. Am J Public Health. 2006;96(6):1007–19. doi:10.2105/AJPH.2005.066720.
Millett GA, Flores SA, Peterson JL, Bakeman R. Explaining disparities in HIV infection among black and white men who have sex with men: a meta-analysis of HIV risk behaviors. AIDS. 2007;21(15):2083–91. doi:10.1097/QAD.0b013e3282e9a64b.
Oster AM, Wiegand RE, Sionean C, et al. Understanding disparities in HIV infection between black and white MSM in the United States. AIDS. 2011;25(March):1103–12. doi:10.1097/QAD.0b013e3283471efa.
Frost SDW. Using sexual affiliation networks to describe the sexual structure of a population. Sex Transm Infect. 2007;83 Suppl 1(suppl_1):i37–42. doi:10.1136/sti.2006.023580.
Laumann EO, Ellingson S, Mahay J, Paik A, Youm Y. The sexual organization of the city. Chicago: University of Chicago Press; 2004.
Browning CR, Soller B, Jackson AL. Neighborhoods and adolescent health-risk behavior: an ecological network approach. Soc Sci Med. 2014;. doi:10.1016/j.socscimed.2014.06.028.
Walton E. Vital places: facilitators of behavioral and social health mechanisms in low-income neighborhoods. Soc Sci Med. 2014;122:1–12. doi:10.1016/j.socscimed.2014.10.011.
Delgado M. The role of Latina-owned beauty parlors in a Latino community. Soc Work. 1997;42:445–53.
Linnan L, Thomas S, D’Angelo H, Owens Ferguson Y. African American Barbershops adn beauty salons: an innovative approach to reducing health disparities through community building and health education. In: Minkler M, editor. Community organizing and community buidilng for health and welfare. New Brunswick, NJ: Rutgers University Press; 2012. p. 229–45.
Small ML. Unanticipated gains: origins of network inequality in everyday life. New York: Oxford University Press; 2009.
Bowles KE, Clark HA, Tai E, et al. Implementing rapid HIV testing in outreach and community settings: results from an advancing HIV prevention demonstration project conducted in seven U.S. cities. Public Health Rep. 2008;Suppl 3(123):78–85.
Centers for Disease Control. HIV testing in non-clinical settings. Div HIV/AIDS Prev Natl Cent HIV/AIDS, Viral Hepatitis, Sex Transm Dis Tuberc Prev Centers Dis Control Prev. 2015. http://www.cdc.gov/msmhealth/msm-programs.htm. Accessed 4 Dec 2015.
White House Office of National AIDS Policy. A National HIV/AIDS strategy for the United States. Washington, DC; 2010.
De P, Singh AE, Wong T, Yacoub W, Jolly AM. Sexual network analysis of a gonorrhoea outbreak. Sex Transm Infect. 2004;80(4):280–5. doi:10.1136/sti.2003.007187.
Klovdahl A, Graviss E, Yaganehdoost A, et al. Networks and tuberculosis: an undetected community outbreak involving public places. Soc Sci Med. 2001;52(5):681–94. doi:10.1016/S0277-9536(00)00170-2.
Binson D, Woods WJ, Pollack L, Paul J, Stall R, Catania JA. Differential HIV risk in bathhouses and public cruising areas. Am J Public Health. 2001;91(9):1482–6. doi:10.2105/AJPH.91.9.1482.
Thiede H, Jenkins RA, Carey JW, et al. Determinants of recent HIV infection among seattle-area men who have sex with men. Am J Public Health. 2009;99(S1):S157–64. doi:10.2105/AJPH.2006.098582.
Seal DW, Kelly JA, Bloom FR, et al. HIV prevention with young men who have sex with men: what young men themselves say is needed. AIDS Care. 2000;12(1):5–26. doi:10.1080/09540120047431.
MacKellar DA, Gallagher KM, Finlayson T, Sanchez T, Lansky A, Sullivan P. Surveillance of HIV risk and prevention behaviors of men who have sex with men: a national application of venue-based, time-space sampling. Public Health Rep. 2007;122(Supplement 1):39–47.
Kelly JA, St Lawrence JS, Diaz YE, et al. HIV risk behavior reduction following intervention with key opinion leaders of population: an experimental analysis. Am J Public Health. 1991;81(2):168–71.
Borgatti SP, Everett MG. Network analysis of 2-mode data. Soc Netw. 1997;19:243–69.
Fujimoto K, Williams ML, Ross MW. Venue-based affiliation networks and HIV risk-taking behavior among male sex workers. Sex Transm Dis. 2013;40(6):453–8. doi:10.1097/OLQ.0b013e31829186e5.
Schneider JA, Walsh T, Cornwell B, Ostrow D, Michaels S, Laumann EO. HIV health center affiliation networks of black men who have sex with men: disentangling fragmented patterns of HIV prevention service utilization. Sex Transm Dis. 2012;39(8):598–604. doi:10.1097/OLQ.0b013e3182515cee.
Gardner EM, McLees MP, Steiner JF, Del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis. 2011;52(6):793–800. doi:10.1093/cid/ciq243.
Mugavero MJ, Amico KR, Horn T, Thompson MA. The state of engagement in HIV care in the United States: from cascade to continuum to control. Clin Infect Dis. 2013;57(8):1164–71. doi:10.1093/cid/cit420.
Khanna AS, Michaels S, Skaathun B, et al. Preexposure prophylaxis awareness and use in a population-based sample of young black men who have sex with men. JAMA Intern Med. 2015;. doi:10.1001/jamainternmed.2015.6536.
Wacquant L. Urban outcasts: a comparative sociology of advanced marginality. Cambridge: Polity; 2008.
Wilson WJ. The truly disadvantaged: the inner city, the underclass, and public policy. Chicago: University of Chicago Press; 1987.
Borgatti SP, Everett MG, Freeman LC. UCINET for windows: software for social network analysis. Harvard, MA: Analytic Technologies; 2002.
Everitt BS, Landau S, Leese M, Stahl D. Cluster analysis. 5th ed. London: Wiley; 2011.
Paterson DL, Swindells S, Mohr J, et al. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med. 2000;133(1):21–30.
Morgan SL, Todd JJ. A diagnostic routine for the detection of consequential heterogeneity of causal effects. Sociol Methodol. 2008;38(1):231–81. doi:10.1111/j.1467-9531.2008.00204.x.
Fleiss JL, Williams JB, Dubro AF. The logistic regression analysis of psychiatric data. J Psychiatr Res. 1986;20(3):195–209.
Burt RS. The network structure of social capital. In: Research in organizational behavior; 2000, vol.22, p. 345–423.
Petroll AE, Mosack KE. Physician awareness of sexual orientation and preventive health recommendations to men who have sex with men. Sex Transm Dis. 2011;38(1):63–7. doi:10.1097/OLQ.0b013e3181ebd50f.
Watkins-Hayes C. The micro dynamics of support seeking: the social and economic utility of institutional ties for HIV-positive women. Ann Am Acad Pol Soc Sci. 2013;647:83–101. doi:10.1177/0002716213475775.
Voisin DR, Bird JDP, Shiu C-S, Krieger C. “It’s crazy being a Black, gay youth”. Getting information about HIV prevention: a pilot study. J Adolesc. 2013;36(1):111–9. doi:10.1016/j.adolescence.2012.09.009.
Choi K-H, Han C, Paul J, Ayala G. Strategies for managing racism and homophobia among U.S. ethnic and racial minority men who have sex with men. AIDS Educ Prev. 2011;23(2):145–58. doi:10.1521/aeap.2011.23.2.145.
Han C. They don’t want to cruise your type: gay men of color and the racial politics of exclusion. Soc Identities. 2007;13(1):51–67. doi:10.1080/13504630601163379.
Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674–97. doi:10.1037/0033-2909.129.5.674.
Lauby JL, Marks G, Bingham T, et al. Having supportive social relationships is associated with reduced risk of unrecognized HIV infection among black and Latino men who have sex with men. AIDS Behav. 2012;16(3):508–15. doi:10.1007/s10461-011-0002-3.
Gonzalez JS, Penedo FJ, Antoni MH, et al. Social support, positive states of mind, and HIV treatment adherence in men and women living with HIV/AIDS. Health Psychol. 2004;23(4):413–8. doi:10.1037/0278-6133.23.4.413.
Bouris A, Hill BJ, Fisher K, et al. Mother-son communication about sex and routine human immunodeficiency virus testing among younger men of color who have sex with men. J Adolesc Heal. 2015;57(5):515–22. doi:10.1016/j.jadohealth.2015.07.007.
Hemmige V, McFadden R, Cook S, Tang H, Schneider JA. HIV prevention interventions to reduce racial disparities in the United States: a systematic review. J Gen Intern Med. 2012;27(8):1047–67. doi:10.1007/s11606-012-2036-2.
Acknowledgements
Data from this project were collected with financial support from the National Institutes of Health (R01 DA033875). Support for this research was also provided by the Agency for Healthcare Research and Quality (R36 HS024167-01) and the National Institutes of Health (R01 MH100021). The content of this paper is the responsibility of the authors and does not reflect the official views of the AHRQ or the NIH. We thank all study respondents for participating. We also thank Alexander Currit, Adam Jonas, Aditya Khanna, Keith Green, Nicola Lancki and other members of the UConnect study team for their advice throughout the research process.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors do not have any conflicts of interest to report. The writing and content of this paper is the sole responsibility of the authors.
Human and animal rights
IRB approval from the University of Chicago and National Opinion Research Center was granted prior to the first wave of UConnect data collection in 2013.
Informed consent
Informed consent was obtained from all study participants and was a criterion for participation in the UConnect study. Participants were only eligible if they were able to provide informed consent at the time of the study visit.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Behler, R.L., Cornwell, B.T. & Schneider, J.A. Patterns of Social Affiliations and Healthcare Engagement Among Young, Black, Men Who Have Sex With Men. AIDS Behav 22, 806–818 (2018). https://doi.org/10.1007/s10461-016-1668-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-016-1668-3