Summary
Background
Funnel mesh implants can be used for both prevention and repair of parastomal hernia (PSH). We aimed to prove the practice of such implants as well as the magnetic resonance (MR) presentability in humans.
Methods
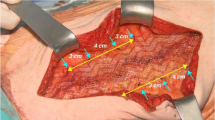
Five patients were surgically treated for laparoscopic PSH prevention, and five patients underwent laparoscopic repair of manifest and symptomatic PSH with iron-loaded 3-D funnel meshes in an intraperitoneal onlay technique. MR investigation was performed on postoperative day 7 to assess mesh delineation, and additionally 6 and 12 months postoperatively to evaluate hernia recurrences and biocompatibility of mesh integration.
Results
We could demonstrate precise mesh depiction and delineation with MR in all 10 cases, as well as accurate assessment of the surrounding tissue. No funnel alterations and no functional change of the stoma bowel patency occurred due to the tightly fitting funnel implant. We documented no mesh-related complications, no PSH formation, and no stoma prolapse occurrence during the follow-up period of 1 year comprising all ten cases.
Conclusion
The pilot use of a new method of MR investigation using a mesh with enhanced signal through the addition of iron particles into the polyvinylidene fluoride base material provides detailed mesh depiction. Furthermore, funnel mesh implantation seems to offer a safe and promising surgical alternative for both PSH prevention and treatment.




Similar content being viewed by others
Abbreviations
- PSH:
-
Parastomal hernia
- MRI:
-
Magnetic resonance investigation/imaging
- PVDF:
-
Polyvinylidene fluoride
- PP:
-
Polypropylene
- IPOM:
-
Intraperitoneal onlay mesh
- GRE:
-
Gradient echo sequence
- TSE:
-
Turbo spin-echo sequence
- MRT:
-
Magnetic resonance tomography
- STI:
-
Surgical textile implants
- CT:
-
Computed tomography
References
Amid PK. Groin hernia repair: open techniques. World J Surg. 2005;29(8):1046–51.
Cassar K, Munro A. Surgical treatment of incisional hernia. Br J Surg. 2002;89(5):534–45.
Seker D, Kulacoglu H. Long-term complications of mesh repairs for abdominal-wall hernias. J Long Term Eff Med Implants. 2011;21(3):205–18.
Krämer NA, Donker HC, Otto J, et al. A concept for magnetic resonance visualization of surgical textile implants. Invest Radiol. 2010;45(8):477–83.
Hansen NL, Barabasch A, Distelmaier M, et al. First in-human magnetic resonance visualization of surgical mesh implants for inguinal hernia treatment. Invest Radiol. 2013;48(11):770–8.
Cingi A, Cakir T, Sever A, et al. Enterostomy site hernias: a clinical and computerized tomographic evaluation. Dis Colon Rectum. 2006;49(10):1559–63.
Hotouras A, Murphy J, Thaha M, et al. The persistent challenge of parastomal herniation: a review of the literature and future developments. Colorectal Dis. 2013;15(5):e202–14.
Jänes A, Cengiz Y, Israelsson LA. Randomized clinical trial of the use of a prosthetic mesh to prevent parastomal hernia. Br J Surg. 2004;91(3):280–2.
Serra-Aracil X, Bombardo-Junca J, Moreno-Matias J, et al. Randomized, controlled, prospective trial of the use of a mesh to prevent parastomal hernia. Ann Surg. 2009;249(4):583–7.
Berger D. Prevention of parastomal hernias by prophylactic use of a specially designed intraperitoneal onlay mesh (Dynamesh IPST). Hernia. 2008;12(3):243–6.
Tam KW, Wei PL, Kuo LJ, et al. Systematic review of the use of a mesh to prevent parastomal hernia. World J Surg. 2010;34(11):2723–9.
Williams NS, Nair R, Bhan C. Stapled mesh stoma reinforcement technique (SMART)—a procedure to prevent parastomal herniation. Ann R Coll Surg Engl. 2011;93(2):169.
Köhler G, Koch OO, Antoniou S, Lechner M, Mayer F, Klinge U, Emmanuel K. Parastomal hernia repair with a 3-D mesh device and additional flat mesh repair of the abdominal wall. Hernia. 2014;18(5):653–61.
Hansson BM, Slater NJ, van der Velden AS, Groenewoud HM, Buyne OR, de Hingh IH, Bleichrodt RP. Surgical techniques for parastomal hernia repair: a systematic review of the literature. Ann Surg. 2012;255(4):685–95.
Penttinen R, Grönroos JM. Mesh repair of common abdominal hernias: a review on experimental and clinical studies. Hernia. 2008;12(4):337–44.
Antoniou SA, Antoniou GA, Koch OO, et al. Lower recurrence rates after mesh-reinforced versus simple hiatal hernia repair: a meta-analysis of randomized trials. Surg Laparosc Endosc Percutan Tech. 2012;22(6):498–502.
Ciritsis A, Hansen NL, Barabasch A, et al. Time-dependent changes of magnetic resonance imaging-visible mesh implants in patients. Invest Radiol. 2014;49(7):439–44.
Klinge U, Klosterhalfen B, Ottinger AP, et al. PVDF as a new polymer for the construction of surgical meshes. Biomaterials. 2002;23(16):3487–93.
Berger D, Bientzle M. Polyvinylidene fluoride: a suitable mesh material for laparoscopic incisional and parastomal hernia repair! A prospective, observational study with 344 patients. Hernia. 2009;13(2):167–72.
Lee L, Saleem A, Landry T, Latimer E, Chaudhury P, Feldman LS. Cost effectiveness of mesh prophylaxis to prevent parastomal hernia in patients undergoing permanent colostomy for rectal cancer. J Am Coll Surg. 2014;218(1):82–91.
Köhler G, Emmanuel K, Schrittwieser R. Single-port parastomal hernia repair by using 3-D textile implants. JSLS. 2014;18(3):pii: e2014.00034.
Wara P. Parastomal hernia repair. An update. Minerva Chir. 2011;66(2):123–8.
Acknowledgments
The kind statistical support by Mag. Christian Steinlechner is greatly acknowledged
Conflict of interest
G. Köhler, H. Wundsam, L. Pallwein-Prettner, O.O. Koch, and K. Emmanuel have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Köhler, G., Wundsam, H., Pallwein-Prettner, L. et al. Magnetic resonance visible 3-D funnel meshes for laparoscopic parastomal hernia prevention and treatment. Eur Surg 47, 127–132 (2015). https://doi.org/10.1007/s10353-015-0319-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10353-015-0319-7