Abstract
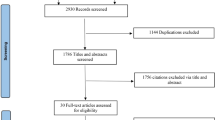
Various clinical trials have explored whether the pulsed dye laser (PDL) method is safe to treat scars, especially surgical scars. However, comprehensive evidence confirming the exact outcomes of PDL for treating surgical scars is lacking. The efficacy and safety of PDL in the treatment of surgical scars were determined through a review of several studies. The PubMed, Embase, Cochrane Library, and Web of Science databases were searched, and the main clinical outcomes were Vancouver Scar Scale (VSS) scores in terms of pigmentation, vascularity, pliability, and height. Review Manager 5.4 software was used for statistical analyses of the data; we chose a standardized mean difference (SMZ) to present the results with 95% confidence interval (CI). Overall, seven randomized controlled trials were used for this meta-analysis, all of these papers used 585 nm or 595 nm PDL with 7 mm or 10 mm spot size and a fluence of 3.5 to 10 J/cm2 for treating surgical scars; besides, the pulse duration ranged from 450 μs to 10 ms. We found that PDL significantly resulted in decreased VSS scores (P = 0.02) in four aspects: pigmentation (P = 0.0002), vascularity (P < 0.00001), pliability (P = 0.0002), and height (P = 0.0002). Moreover, scar improvement was similar when using 585 nm and 595 nm PDL in terms of pigmentation (P = 0.76), vascularity (P = 0.34), pliability (P = 0.64), and height (P = 0.57). Furthermore, our review indicated that PDL has no obvious adverse effects for most people, except transitory erythema and purpura. The meta-analysis showed that both 585 nm and 595 nm PDL therapy can effectively reduce the VSS score, suggesting that PDL can be a safe and effective method for the treatment of surgical scars.





Similar content being viewed by others
References
Lee Peng G, Kerolus JL (2019) Management of surgical scars. Facial Plast Surg Clin North Am 27:513–517
Ziolkowski N, Kitto SC, Jeong D, Zuccaro J, Adams-Webber T, Miroshnychenko A, Fish JS (2019) Psychosocial and quality of life impact of scars in the surgical, traumatic and burn populations: a scoping review protocol. BMJ Open 9:e021289
Tebble NJ, Adams R, Thomas DW, Price P (2006) Anxiety and self-consciousness in patients with facial lacerations one week and six months later. Br J Oral Maxillofac Surg 44:520–525
Marshall CD, Hu MS, Leavitt T, Barnes LA, Lorenz HP, Longaker MT (2018) Cutaneous scarring: basic science, current treatments, and future directions. Adv Wound Care (New Rochelle) 7:29–45
Anderson RR, Parrish JA (1983) Selective photothermolysis: precise microsurgery by selective absorption of pulsed radiation. Science 220:524–527
Liu A, Moy RL, Ross EV, Hamzavi I, Ozog DM (2012) Pulsed dye laser and pulsed dye laser-mediated photodynamic therapy in the treatment of dermatologic disorders. Dermatol Surg 38:351–366
Smit JM, Bauland CG, Wijnberg DS, Spauwen PHM (2005) Pulsed dye laser treatment, a review of indications and outcome based on published trials. Br J Plast Surg 58:981–987
Wanitphakdeedecha R, Jantarakolica T, Ng JNC, Yan C, Nanchaipruek Y, Jantanapornchai N, Manuskiatti W, Sudhipongpracha T (2021) The cost-effectiveness of pulsed-dye laser therapy among Thai patients with facial port-wine stain: a retrospective study and economic evaluation. Dermatol Ther (Heidelb) 11:465–473
Zhang L, Wu HW, Yuan W, Zheng JW (2017) Propranolol therapy for infantile hemangioma: our experience. Drug Des Dev Ther 11:1401–1408
Feaster B, Cline A, Feldman SR, Taylor S (2019) Clinical effectiveness of novel rosacea therapies. Curr Opin Pharmacol 46:14–18
Gao L, Qu H, Gao N, Li K, Dang E, Tan W, Wang G (2020) A retrospective analysis for facial telangiectasia treatment using pulsed dye laser and intense pulsed light configured with different wavelength bands. J Cosmet Dermatol 19:88–92
Alster TS, Williams CM (1995) Treatment of keloid sternotomy scars with 585 nm flashlamp-pumped pulsed-dye laser. Lancet 345:1198–1200
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA Cochrane Handbook for Systematic Reviews of Interventions version 6.2(updated February 2021). Cochrane, 2021. Available from https://www.training.cochrane.org/handbook
Nouri K, Jimenez GP, Harrison-Balestra C, Elgart GW (2003) 585-nm pulsed dye laser in the treatment of surgical scars starting on the suture removal day. Dermatol Surg 29:65–73 (discussion 73)
Conologue TD, Norwood C (2006) Treatment of surgical scars with the cryogen-cooled 595 nm pulsed dye laser starting on the day of suture removal. Dermatol Surg 32:13–20
Nouri K, Rivas MP, Stevens M, Ballard CJ, Singer L, Ma F, Vejjabhinanta V, Elsaie ML, George WE (2009) Comparison of the effectiveness of the pulsed dye laser 585 nm versus 595 nm in the treatment of new surgical scars. Lasers Med Sci 24:801–810
Ha JM, Kim HS, Cho EB, Park GH, Park EJ, Kim KH, Kim LS, Kim KJ (2014) Comparison of the effectiveness of nonablative fractional laser versus pulsed-dye laser in thyroidectomy scar prevention. Ann Dermatol 26:615–620
Kim DH, Ryu HJ, Choi JE, Ahn HH, Kye YC, Seo SH (2014) A comparison of the scar prevention effect between carbon dioxide fractional laser and pulsed dye laser in surgical scars. Dermatol Surg 40:973–978
Vazquez-Martinez O, Eichelmann K, Garcia-Melendez M, Miranda I, Avila-Lozano A, Vega D, Ocampo-Candiani J (2015) Pulsed dye laser for early treatment of scars after dermatological surgery. J Drugs Dermatol 14:1209–1212
Pongcharoen P, Pongcharoen B, Disphanurat W (2019) The effectiveness of a 595 nm pulsed-dye-laser in the treatment of surgical scars following a knee arthroplasty. J Cosmet Laser Ther 21:352–356
Dai R, Xie H, Hua W, Li XH, Li L (2017) The efficacy and safety of the fractional radiofrequency technique for the treatment of atrophic acne scar in Asians: a meta-analysis. J Cosmet Laser Ther 19:337–344
Baryza MJ, Baryza GA (1995) The Vancouver Scar Scale: an administration tool and its interrater reliability. J Burn Care Rehabil 16:535–538
Alam M, Pon K, Van Laborde S, Kaminer MS, Arndt KA, Dover JS (2006) Clinical effect of a single pulsed dye laser treatment of fresh surgical scars: randomized controlled trial. Dermatol Surg 32:21–25
Tierney E, Mahmoud BH, Srivastava D, Ozog D, Kouba DJ (2009) Treatment of surgical scars with nonablative fractional laser versus pulsed dye laser: a randomized controlled trial. Dermatol Surg 35:1172–1180
Anderson RR, Parrish JA (1981) Microvasculature can be selectively damaged using dye lasers: a basic theory and experimental evidence in human skin. Lasers Surg Med 1:263–276
Tan OT, Murray S, Kurban AK (1989) Action spectrum of vascular specific injury using pulsed irradiation. J Invest Dermatol 92:868–871
Kent RA, Shupp J, Fernandez S, Prindeze N, DeKlotz CMC (2020) Effectiveness of early laser treatment in surgical scar minimization: a systematic review and meta-analysis. Dermatol Surg 46:402–410
Cohen JL, Geronemus R (2016) Safety and efficacy evaluation of pulsed dye laser treatment, CO2 ablative fractional resurfacing, and combined treatment for surgical scar clearance. J Drugs Dermatol 15:1315–1319
Funding
WX received a research grant (No. 2020364003) from the Zhejiang Medical and Health Science and Technology Program, China (http://www.msttp.com/). The funder had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. This work was supported by the National Natural Science Foundation of China (81872517). These fundings were used in the study design, data collection and analysis, fellow’s service fees, and preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
None.
Informed consent
None.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article was registered in PROSPERO with registration number CRD42021230258.
Rights and permissions
About this article
Cite this article
Cai, Y., Zeng, X., Ying, J. et al. Efficacy and safety of pulsed dye laser for the treatment of surgical scars: a systematic review and meta-analysis. Lasers Med Sci 37, 1273–1282 (2022). https://doi.org/10.1007/s10103-021-03385-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-021-03385-z