Abstract
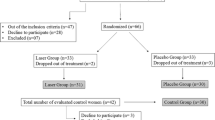
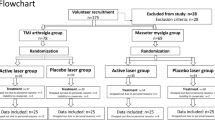
The aim was to analyze the non-specific effects (placebo, spontaneous remission, and regression to the mean) of the low-level laser therapy (LLLT) in women with myofascial pain (painful temporomandibular disorder (TMD)), as well as to differentiate between responders and non-responder clusters to active and placebo LLLT according to the anxiety levels, salivary cortisol, use of oral contraceptives, and premenstrual period. Sixty-four women diagnosed with myofascial pain (Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD)) were included, divided into laser (n = 20), placebo group (n = 21), and 23 controls (without treatment (WT)). The LLLT applied was 780 nm, masseter and temporal = 5 J/cm2 (20 mW–0.5 W/cm2), and TMJ area = 7.5 J/cm2 (30 mW–0.8 W/cm2), eight sessions, twice a week. The pain intensity (visual analogue scale (VAS)), anxiety (Beck Anxiety Inventory), salivary cortisol, and menstrual cycle’s data at the baseline, T1–T8, and 30 days after LLLT (follow-up) were evaluated. The laser group showed 80% of pain reduction, placebo 85%, and WT 43% in T8. Women with severe anxiety and at the premenstrual period did not reduce pain with any LLLT. Active and placebo LLLT had similar effectiveness during the treatment period; however, women with moderate anxiety, cortisol levels above 10 ng/ml, and without contraceptive use maintain analgesia longer with active LLLT than placebo (follow-up 30 days). Women with low levels of anxiety, salivary cortisol below 10 ng/ml, and with contraceptive use showed the higher pain reduction. The analgesia promoted by LLLT in women with myofascial pain is a result of non-specific effects during the treatment period, although active LLLT is more effective in maintaining the analgesia after treatment (30 days) for the cluster of women with moderate anxiety, salivary cortisol above 10 ng/ml, and without contraceptive use.





Similar content being viewed by others
References
Dıraçoglu D et al (2008) Temporomandibular dysfunction and risk factors for anxiety and depression. J Back Musculoskelet Rehabil 29(3):487–491
Nahman-Averbuch H et al (2016) Relationship between personality traits and endogenous analgesia: the role of harm avoidance. Pain Pract 16(1):38–45
Reissmann DR et al (2014) Temporomandibular disorder pain is related to the general disposition to be anxious. J Oral Facial Pain Headache 28(4):322–330
Drobek W, Schoenaers J, De Laat A (2002) Hormone-dependent fluctuations of pressure pain threshold and tactile threshold of the temporalis and masseter muscle. J Oral Rehabil 29(11):1042–1051
Lim PF et al (2010) Development of temporomandibular disorders is associated with greater bodily pain experience. Clin J Pain 26(2):116–120
Chen J et al (2015) Efficacy of low-level laser therapy in the treatment of TMDs: a meta-analysis of 14 randomised controlled trials. J Oral Rehabil 42(4):291–299
Iyomasa MM et al (2013) Zymographic and ultrastructural evaluations after low-level laser irradiation on masseter muscle of HRS/J strain mice. Lasers Med Sci 28(3):777–783
Silveira PC et al (2013) Effects of low-level laser therapy (GaAs) in an animal model of muscular damage induced by trauma. Lasers Med Sci 28(2):431–436
de Melchior MO et al (2013) Does low intensity laser therapy reduce pain and change orofacial myofunctional conditions? Cranio 31(2):133–139
De Moraes Maia ML et al (2014) Evaluation of low-level laser therapy effectiveness on the pain and masticatory performance of patients with myofascial pain. Lasers Med Sci 29(1):29–35
Sancakli E et al (2015) Early results of low-level laser application for masticatory muscle pain: a double-blind randomized clinical study. BMC Oral Health 15(1):131
Magri LV et al (2017) Effectiveness of low-level laser therapy on pain intensity, pressure pain threshold, and SF-MPQ indexes of women with myofascial pain. Lasers Med Sci 32(2):419–428
Schiffman EL (2010) The research diagnostic criteria for temporomandibular disorders. V: methods used to establish and validate revised Axis I diagnostic algorithms. J Orofac Pain 24(1):63–78
Hill CM, Walker RV (2001) Salivary cortisol determination and self-rating scales in the assessment of stress in patients undergoing the extraction of wisdom teeth. Br Dent J 191:513–515
Kobayashi H et al (2017) Diurnal changes in distribution characteristics of salivary cortisol and immunoglobulin a concentrations. Int J Environ Res Public Health 31:14(9)
Smyth J et al (1997) Individual differences in the diurnal cycle of cortisol. Psychoneuroendocrinology 22:89–105
Kirschbaum C et al (1999) Impact of gender, menstrual cycle phase, and oral contraceptives on the activity of the hypothalamus-pituitary-adrenal axis. Psychosom Med 61:154–162
Oken BS (2008) Placebo effects: clinical aspects and neurobiology. Brain 131(11):2812–2823
Colagiuri B et al (2015) The placebo effect: from concepts to genes. Neuroscience 307:171–190
Jakovljevic M (2014) The placebo-nocebo response: controversies and challenges from clinical and research perspective. Eur Neuropsychopharmacol 24(3):333–341
Frisaldi E, Piedimonte A, Benedetti F (2015) Placebo and nocebo effects: a complex interplay between psychological factors and neurochemical networks. Am J Clin Hypn 57(3):267–284
Morton V, Torgerson DJ (2003) Effect of regression to the mean on decision making in health care. BMJ 326(7398):1083–1084
Hróbjartsson A, Gøtzsche PC (2010) Placebo interventions for all clinical conditions. Cochrane Database Syst Ver 1:CD003974
Ferreira ML et al (2013) The smallest worthwhile effect of nonsteroidal anti-inflammatory drugs and physiotherapy for chronic low back pain: a benefit-harm trade-off study. J Clin Epidemiol 66(12):1397–1404
O'Brien EM et al (2010) Patient-centered perspective on treatment outcomes in chronic pain. Pain Med 11(1):6–15
Zeppieri G Jr et al (2012) Preliminary results of patient-defined success criteria for individuals with musculoskeletal pain in outpatient physical therapy settings. Arch Phys Med Rehabil 93(3):434–440
Dworkin RH et al (2008) Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J Pain 9(2):105–121
Jo KB et al (2016) Association of pain intensity, pain-related disability, and depression with hypothalamus-pituitary-adrenal axis function in female patients with chronic temporomandibular disorders. Psychoneuroendocrinology 69:106–115
Slade GD et al (2016) Painful temporomandibular disorder: decade of discovery from OPPERA studies. J Dent Res 95(10):1084–1092
Godfrey KM et al (2014) Salivary cortisol and cold pain sensitivity in female twins. Ann Behav Med 47(2):180–188
Salameh E et al (2015) Investigation of the relationship between psychosocial stress and temporomandibular disorder in adults by measuring salivary cortisol concentration: a case-control study. J Indian Prosthodont Soc 15(2):148–152
Vilanova LS et al (2015) Hormonal fluctuations intensify temporomandibular disorder pain without impairing masticatory function. Int J Prosthodont 8(1):72–74
Berger M et al (2015) Association between estrogen levels and temporomandibular disorders: a systematic literature review. Prz Menopauzalny 14(4):260–270
Devall AJ, Lovick TA (2010) Differential activation of the periaqueductal gray by mild anxiogenic stress at different stages of the estrous cycle in female rats. Neuropsychopharmacology 35(5):1174–1185
Acknowledgments
This study was financially supported by Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) and Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures were performed in accordance with the guidelines of the Brazilian Ethics Committee on Human Research. This study was conducted after approval by the Ethics Committee of the School of Dentistry of Ribeirão Preto (under protocol 33658114.7.0000.5419). All subjects were informed about the study and signed a consent form. Patients who composed the placebo group and did not have pain reduction after the study completion were invited to receive treatment with LLLT, in the same parameters of the active laser group.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Magri, L.V., Carvalho, V.A., Rodrigues, F.C.C. et al. Non-specific effects and clusters of women with painful TMD responders and non-responders to LLLT: double-blind randomized clinical trial. Lasers Med Sci 33, 385–392 (2018). https://doi.org/10.1007/s10103-017-2406-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-017-2406-4