Abstract
Purpose
To review the literature on the efficacy and safety of perineural steroid injections around the ilioinguinal, iliohypogastric, and genitofemoral nerves for chronic postoperative inguinal pain (CPIP).
Methods
A scoping review was performed to find all relevant case reports, case series, prospective or retrospective cohort studies, case–control studies, and randomized controlled trials (RCTs) where a steroid was used for perineural procedures around ilioinguinal, iliohypogastric, and/or genitofemoral nerves for CPIP. Databases searched included Ovid MEDLINE, EMBASE, CINHAL, Cochrane CENTRAL, and Google Scholar.
Results
A total of five publications were found—three studies were prospective case series, one a retrospective cohort study, and one a RCT. The most common steroids used were methylprednisolone and triamcinolone. The average methylprednisolone-equivalent dose used per procedure was 46 mg (SD 21.9). Procedural guidance included anatomic landmarks (three studies), nerve stimulation and ultrasound (one study), and computed tomography guidance (one study). Four studies reported analgesic benefit in 55–75 % of included patients, with one study documenting an effect up to 50 months later after steroid perineural injections. The RCT demonstrated no benefit of adding steroid to a local anesthetic in the perioperative setting but it did not enroll patients with existing neuropathic pain. No adverse outcomes of perineural steroids were documented within reviewed studies.
Conclusions
The paucity of data, heterogeneity and lack of appropriate control groups in the available literature precludes firm conclusions on the efficacy and safety of perineural steroids for CPIP. Future adequately powered, high-quality, placebo-controlled studies are needed.


Similar content being viewed by others
References
Rosenberg J, Bisgaard T, Kehlet H et al (2011) Danish Hernia Database recommendations for the management of inguinal and femoral hernia in adults. Dan Med Bull 58:42–43
Rutkow I (2003) Demographic and socioeconomic aspects of hernia repair in the United States in 2003. Surg Clin North Am 83:1045–1051
Bay-Nielsen M, Kehlet H, Strand L et al (2001) Quality assessment of 26 304 herniorrhaphies in Denmark: a prospective nationwide study. Lancet 358:1124–1128. doi:10.1016/S0140-6736(01)06251-1
Macrae WA (2008) Chronic post-surgical pain: 10 years on. Br J Anaesth 101:77–86. doi:10.1093/bja/aen099
Fitzgibbons RJ, Forse RA (2015) Groin hernias in adults. N Engl J Med 372:756–763. doi:10.1056/NEJMcp1404068
Jenkins J, O’Dwyer P (2008) Inguinal hernias. BMJ 124:687–691
Turk DC, Rudy TE (1987) IASP taxonomy of chronic pain syndromes: preliminary assessment of reliability. Pain 30:177–189
Kehlet H, Jensen TS, Woolf CJ (2006) Persistent postsurgical pain: risk factors and prevention. Lancet 367:1618–1625. doi:10.1016/S0140-6736(06)68700-X
Visser EJ (2006) Chronic post-surgical pain: epidemiology and clinical implications for acute pain management. Acute Pain 8:73–81. doi:10.1016/j.acpain.2006.05.002
Poobalan AS, Bruce J, Smith WCS et al (2003) A review of chronic pain after inguinal herniorrhaphy. Clin J Pain 19:48–54
Simons MP, Aufenacker T, Bay-Nielsen M et al (2009) European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia. doi:10.1007/s10029-009-0529-7
Staal E, Nienhuijs SW, Keemers-Gels ME et al (2008) The impact of pain on daily activities following open mesh inguinal hernia repair. Hernia 12:153–157. doi:10.1007/s10029-007-0297-1
Kalliomäki ML, Sandblom G, Gunnarsson U, Gordh T (2009) Persistent pain after groin hernia surgery: a qualitative analysis of pain and its consequences for quality of life. Acta Anaesthesiol Scand 53:236–246. doi:10.1111/j.1399-6576.2008.01840.x
Racz G, Hagstrom D (1992) Iliohypogastric and ilioinguinal nerve entrapment: diagnosis and treatment. Pain Dig 2:43–48
Devor M, Seltzer Z (1999) Pathophysiology of damaged nerves in relation to chronic pain. In: Textbook of pain. Churchill Livingstone, Edinburgh, United Kingdom, pp 129–164
Wantz G (1993) Testicular atrophy and chronic residual neuralgia as risks of inguinal hernioplasty. Surg Clin North Am 73:571–581
Fränneby U, Sandblom G, Nordin P (2006) Risk factors for long-term pain after hernia surgery. Ann Surg 244:212
Callesen T, Bech K, Nielsen R et al (1998) Pain after groin hernia repair. Br J Surg 85:1412–1414. doi:10.1046/j.1365-2168.1998.00864.x
Vuilleumier H, Hübner M, Demartines N (2009) Neuropathy after herniorrhaphy: indication for surgical treatment and outcome. World J Surg 33:841–845
Hua S, Chen Y (1989) Membrane receptor-mediated electrophysiological effects of glucocorticoid on mammalian neurons*. Endocrinology 124:687–691
Flower R, Blackwell G (1979) Anti-inflammatory steroids induce biosynthesis of a phospholipase A2 inhibitor which prevents prostaglandin generation. Nature 278:456–459
Abdi MS (2007) Epidural steroids in the management of chronic spinal pain: a systematic review. Pain 10:185–212
Bhatia A, Flamer D, Shah P (2015) Perineural steroids for trauma and compression-related peripheral neuropathic pain: a systematic review and meta-analysis. Can J Anesth 62:650–662
Knight C, Burnell J (1980) Systemic side-effects of extradural steroids. Anaesthesia 35:593–594
Olefsky J, Kimmerling G (1976) Effects of glucocorticoids on carbohydrate metabolism. Am J Med Sci 271:202–210
Stuck A, Minder C, Frey F (1989) Risk of infectious complications in patients taking glucocorticosteroids. Rev Infect Dis 11:954–963
Arksey H, O’Malley L (2005) Scoping studies: towards a methodological framework. Int J Soc Res Methodol 8:19–32
Palumbo P, Minicucci A, Nasti A et al (2007) Treatment for persistent chronic neuralgia after inguinal hernioplasty. Hernia 11:527–531. doi:10.1007/s10029-007-0268-6
Aroori S, Spence RA (2007) Chronic pain after hernia surgery—an informed consent issue. Ulster Med J 76:136–140
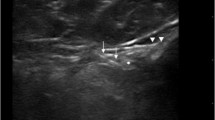
Thomassen I, van Suijlekom J, van de Gaag A et al (2013) Ultrasound-guided ilioinguinal/iliohypogastric nerve blocks for chronic pain after inguinal hernia repair. Hernia 17:329–332. doi:10.1007/s10029-012-0998-y
Kastler A, Aubry S, Piccand V et al (2012) Radiofrequency neurolysis versus local nerve infiltration in 42 patients with refractory chronic inguinal neuralgia. Pain Physician 15:237–244
McCleane G, Mackle E, Stirling I (1994) The addition of triamcinolone acetonide to bupivacaine has no effect on the quality of analgesia produced by ilioinguinal nerve block. Anaesthesia 49:819–820
Bouhassira D, Attal N, Alchaar H, Boureau F (2005) Comparison of pain syndromes associated with nervous or somatic lesions and development of a new neuropathic pain diagnostic questionnaire (DN4). Pain 114:29–36
Al-dabbagh A (2002) Anatomical variations of the inguinal nerves and risks of injury in 110 hernia repairs. Surg Radiol Anat 24:102–107
Whiteside J, Barber M, Walters M, Falcone T (2003) Anatomy of ilioinguinal and iliohypogastric nerves in relation to trocar placement and low transverse incisions. Am J Obstet Gynecol 189:1574–1578
Rab M, Dellon A (2001) Anatomic variability of the ilioinguinal and genitofemoral nerve: implications for the treatment of groin pain. Plast Reconstr Surg 108:1618–1623
Weintraud M, Marhofer P (2008) Ilioinguinal/iliohypogastric blocks in children: where do we administer the local anesthetic without direct visualization? Anesth Analg 106:89–93
Bhatia A, Brull R (2013) Is ultrasound guidance advantageous for interventional pain management? a systematic review of chronic pain outcomes. Anesth Analg 117:236–251
Bischoff J, Koscielniak-Nielsen Z, Kehlet H, Werner M (2012) Ultrasound-guided ilioinguinal/iliohypogastric nerve blocks for persistent inguinal postherniorrhaphy pain: a randomized, double-blind, placebo-controlled, crossover. Anesth Analg 114:1323–1329
Loos M, Scheltinga M, Roumen R (2010) Tailored neurectomy for treatment of postherniorrhaphy inguinal neuralgia. Surgery 147:275–281
Aasvang E, Kehlet H (2005) Surgical management of chronic pain after inguinal hernia repair. Br J Surg 92:795–801
Bhatia A, Flamer D, Shah PS, Cohen SP (2016) Transforaminal epidural steroid injections for treating lumbosacral radicular pain from herniated intervertebral discs: a systematic review and metaanalysis. Anesth Analg 122:857–870
La Cesa S, Tamburin S, Tugnoli V et al (2015) How to diagnose neuropathic pain? The contribution from clinical examination, pain questionnaires and diagnostic tests. Neurol Sci 36:2169–2175
van Hecke O, Kamerman P, Attal N et al (2015) Neuropathic pain phenotyping by international consensus (NeuroPPIC) for genetic studies: a NeuPSIG systematic review, Delphi survey, and expert panel. Pain 156:2337–2353
Farrar J, Portenoy R, Berlin J et al (2000) Defining the clinically important difference in pain outcome measures. Pain 88:287–294
Dworkin R, O’Connor A, Kent J et al (2013) Interventional management of neuropathic pain: NeuPSIG recommendations. Pain 154:2249–2261
Finnerup N, Attal N, Haroutounian S et al (2015) Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis. Lancet Neurol 14:162–173
Lange JFM, Kaufmann R, Wijsmuller AR et al (2015) An international consensus algorithm for management of chronic postoperative inguinal pain. Hernia 19:33–43. doi:10.1007/s10029-014-1292-y
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors Khan, Rai, Rajan, Jackson, and Bhatia have no conflicts of interest to declare.
Rights and permissions
About this article
Cite this article
Khan, J.S., Rai, A., Sundara Rajan, R. et al. A scoping review of perineural steroids for the treatment of chronic postoperative inguinal pain. Hernia 20, 367–376 (2016). https://doi.org/10.1007/s10029-016-1487-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10029-016-1487-5