Abstract
Background
Cranial reconstruction with autologous bone is still the gold standard although several biomaterials are available to re-establish the integrity of the cranial vault. Due to their biological and morphological characteristics, hydroxyapatite implants show promising results in small clinical cohort studies, especially within the paediatric population. Its biocompatibility and osteoconductivity should allow the formation of osseous bridging at the skull-prosthesis interface.
Objective
To examine the possible occurrence of osteointegration and to quantify it.
Methods
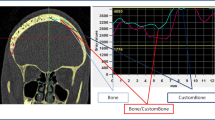
A retrospective study of patients with a hydroxyapatite implant from 2010 to 2014 at our neurosurgical department was conducted. Demographic, surgical and radiological data were studied. A senior neuroradiologist, a staff member neurosurgeon and a resident neurosurgeon independently performed the radiological evaluation. A new software analysis technique was developed to objectively quantify the degree of osteointegration.
Results
Seventeen implants were evaluated with an average patient age of 39 years and a mean follow-up of 155 weeks. Through radiologic evaluation, osseous bridging was deemed higher than 50% in six prostheses and higher than 75% in three. In five patients, no osteointegration could be seen. The remaining patients exhibited sparse signs of osteointegration, estimated between 10 and 50%. Software analysis showed an average osteointegration ratio of 37.4% with a 400-HU filter and 27.3% with a 700-HU filter.
Conclusion
In this small retrospective study of cranial hydroxyapatite implants, osteointegration did occur and to a degree of more than 50% in 1/3 of the patients.




Similar content being viewed by others
References
Brie J, Chartier T, Chaput C, Delage C, Pradeau B, Caire F, Boncoeur M-P, Moreau J-J (2013) A new custom made bioceramic implant for the repair of large and complex craniofacial bone defects. J Cranio-Maxillofac Surg 41:403–407. https://doi.org/10.1016/j.jcms.2012.11.005
Cheng YK, Weng HH, Yang JT, Lee MH, Wang TC, Chang CN (2008) Factors affecting graft infection after cranioplasty. J Clin Neurosci 15:1115–1119. https://doi.org/10.1016/j.jocn.2007.09.022
Fini M, Giavaresi G, Salamanna F, Veronesi F, Martini L, De Mattei M, Tschon M (2011) Harmful lifestyles on orthopedic implantation surgery: a descriptive review on alcohol and tobacco use. J Bone Miner Metab 29:633–644. https://doi.org/10.1007/s00774-011-0309-1
Frassanito P, De Bonis P, Mattogno PP, Mangiola A, Novello M, Brinchi D, Pompucci A, Anile C (2013) The fate of a macroporous hydroxyapatite cranioplasty four years after implantation: macroscopical and microscopical findings in a case of recurrent atypical meningioma. Clin Neurol Neurosurg 115:1496–1498. https://doi.org/10.1016/j.clineuro.2012.11.032
Fricia M, Passanisi M, Salamanna F, Parrilli A, Giavaresi G, Fini M (2015) Osteointegration in custom-made porous hydroxyapatite cranial implants: from reconstructive surgery to regenerative medicine. World Neurosurg 84:591.e511–591.e596. https://doi.org/10.1016/j.wneu.2015.03.027
Galluzzi P, De Francesco S, Giacalone G, Cerase A, Monti L, Vallone IM, Lazzeretti L, Venturi C, Hadjistilianou T (2011) Contrast-enhanced magnetic resonance imaging of fibrovascular tissue ingrowth within synthetic hydroxyapatite orbital implants in children. Eur J Ophthalmol 21:521–528. https://doi.org/10.5301/ejo.2011.6298
Hardy H, Tollard E, Derrey S, Delcampe P, Peron JM, Freger P, Proust F (2012) Clinical and ossification outcome of custom-made hydroxyapatite prothese for large skull defect. Neuro-Chirurgie 58:25–29. https://doi.org/10.1016/j.neuchi.2011.09.006
Kiyokawa K, Hayakawa K, Tanabe HY, Inoue Y, Tai Y, Shigemori M, Tokutomi T (1998) Cranioplasty with split lateral skull plate segments for reconstruction of skull defects. J Craniomaxillofac Surg 26:379–385
Lopez Gonzalez A, Perez Borreda P, Conde Sardon R (2015) Fracture of a HTR-PMI cranioplastic implant after severe TBI. Childs Nerv Syst 31:333–336. https://doi.org/10.1007/s00381-014-2493-5
Martini L, Staffa G, Giavaresi G, Salamanna F, Parrilli A, Serchi E, Pressato D, Arcangeli E, Fini M (2012) Long-term results following cranial hydroxyapatite prosthesis implantation in a large skull defect model. Plast Reconstr Surg 129:625e–635e. https://doi.org/10.1097/PRS.0b013e318244220d
Mastrogiacomo M, Scaglione S, Martinetti R, Dolcini L, Beltrame F, Cancedda R, Quarto R (2006) Role of scaffold internal structure on in vivo bone formation in macroporous calcium phosphate bioceramics. Biomaterials 27:3230–3237. https://doi.org/10.1016/j.biomaterials.2006.01.031
Matsuno A, Tanaka H, Iwamuro H, Takanashi S, Miyawaki S, Nakashima M, Nakaguchi H, Nagashima T (2006) Analyses of the factors influencing bone graft infection after delayed cranioplasty. Acta Neurochir 148:535–540; discussion 540. https://doi.org/10.1007/s00701-006-0740-6
Messina G, Dones I, Nataloni A, Franzini A (2011) Histologically demonstrated skull bone integration in a hydroxyapatite prosthesis in a human. Acta Neurochir 153:1717–1718. https://doi.org/10.1007/s00701-011-1014-5
Movassaghi K, Ver Halen J, Ganchi P, Amin-Hanjani S, Mesa J, Yaremchuk MJ (2006) Cranioplasty with subcutaneously preserved autologous bone grafts. Plast Reconstr Surg 117:202–206
Ono H, Sase T, Tanaka Y, Takasuna H (2017) Histological assessment of porous custom-made hydroxyapatite implants 6 months and 2.5 years after cranioplasty. Surg Neurol Int 8:8. https://doi.org/10.4103/2152-7806.198735
Park SP, Kim JH, Kang HI, Kim DR, Moon BG, Kim JS (2017) Bone flap resorption following cranioplasty with autologous bone: quantitative measurement of bone flap resorption and predictive factors. J Korean Neurosurg Soc 60:749–754. https://doi.org/10.3340/jkns.2017.0203.002
Rienzo AD, Iacoangeli M, di Somma LGM, Alvaro L, Nocchi N, Scerrati M (2012) Shape modifications of porous hydroxyapatite prostheses to improve rigid implant fixation: experience in 12 cases. Surg Neurol Int 3:161
Spirnak JP, Nieves N, Hollsten DA, White WC, Betz TA Gadolinium-enhanced magnetic resonance imaging assessment of hydroxyapatite orbital implants. Am J Ophthalmol 119:431–440. https://doi.org/10.1016/S0002-9394(14)71228-0
Sprio S, Fricia M, Maddalena GF, Nataloni A, Tampieri A (2016) Osteointegration in cranial bone reconstruction: a goal to achieve. J Appl Biomater Funct Mater 14:e470–e476. https://doi.org/10.5301/jabfm.5000293
Staffa G, Nataloni A, Compagnone C, Servadei F (2007) Custom made cranioplasty prostheses in porous hydroxy-apatite using 3D design techniques: 7 years experience in 25 patients. Acta Neurochir 149:161–170; discussion 170. https://doi.org/10.1007/s00701-006-1078-9
Staffa G, Barbanera A, Faiola A, Fricia M, Limoni P, Mottaran R, Zanotti B, Stefini R (2012) Custom made bioceramic implants in complex and large cranial reconstruction: a two-year follow-up. J Craniomaxillofac Surg 40:e65–e70. https://doi.org/10.1016/j.jcms.2011.04.014
Stefini R, Esposito G, Zanotti B, Iaccarino C, Fontanella MM, Servadei F (2013) Use of “custom made” porous hydroxyapatite implants for cranioplasty: postoperative analysis of complications in 1549 patients. Surg Neurol Int 4:12. https://doi.org/10.4103/2152-7806.106290
Stefini R, Zanotti B, Nataloni A, Martinetti R, Scafuto M, Colasurdo M, Tampieri A (2015) The efficacy of custom-made porous hydroxyapatite prostheses for cranioplasty: evaluation of postmarketing data on 2697 patients. J Appl Biomater Funct Mater 13:e136–e144. https://doi.org/10.5301/jabfm.5000211
Stenderup K, Rosada C, Justesen J, Al-Soubky T, Dagnaes-Hansen F, Kassem M (2004) Aged human bone marrow stromal cells maintaining bone forming capacity in vivo evaluated using an improved method of visualization. Biogerontology 5:107–118. https://doi.org/10.1023/B:BGEN.0000025074.88476.e2
Winkler PA, Stummer W, Linke R, Krishnan KG, Tatsch K (2000) Influence of cranioplasty on postural blood flow regulation, cerebrovascular reserve capacity, and cerebral glucose metabolism. J Neurosurg 93:53–61. https://doi.org/10.3171/jns.2000.93.1.0053
Zaccaria L, Tharakan SJ, Altermatt S (2016) Hydroxyapatite ceramic implants for cranioplasty in children: a single-center experience. Childs Nerv Syst 33:343–348
Zanotti B, Zingaretti N, Almesberger D, Verlicchi A, Stefini R, Ragonese M, Guarneri GF, Parodi PC (2014) Enhancing dermal and bone regeneration in calvarial defect surgery. Indian J Plast Surg 47:325–332. https://doi.org/10.4103/0970-0358.146581
Zanotti B, Verlicchi A, Indiani S, Scarparo SA, Zingaretti N, Parodi PC (2015) Spontaneous fractures in custom-made porous hydroxyapatite cranioplasty implants: is fragility the only culprit? Acta Neurochir 157:517–523. https://doi.org/10.1007/s00701-014-2319-y
Zanotti B, Verlicchi A, Stefini R, Salgarelli AC, Zingaretti N, Parodi PC, Matteo C, Robiony M (2015) Surgical pitfalls with custom-made porous hydroxyapatite cranial implants. Plastic and Aesthetic Research 2:7–11
Acknowledgements
Software analysis technique was developed together with Materialise (Leuven, Belgium).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Each patient signed an informed consent. Approval of the Ethics Committee of the hospital was obtained.
Competing interests
The authors declare that they have no competing interests.
Additional information
Comments
Even if there are a number of papers dealing with HA cranioplasty implants, very few papers have really examined the possibility of osteointegration. Since HA cranioplasty is expensive, the plus offered by this method of cranial reconstruction is bone integration. This makes HA a biological material differently from all the other materials used for cranioplasty (PEEK, PMMA, titanium...) which are materials not integrated into the skull and acting as a foreign body.
There are very few published papers with a good CT follow-up study to demonstrate osteointegration. Furthermore, to my knowledge, this is the first study to demonstrate a relationship between CT data and gadolinium MRI data. MRI can show the presence of small new vessels within the cranioplasty than confirming bone colonisation.
The results of the study with a long follow-up in an adult population show that in a majority of cases, osteointegration did occur even if to a different degree.
With the limit of the small number of cases and of the retrospective data collection, these patients show that it is possible and feasible to use a biological material for cranial reconstruction.
The authors have described one case of HA cranioplasty fracture 2 years after implantation. There is an important message never presented before: we can probably measure with gadolinium MRI (this is the only message never presented before the presence of osteointegration was already reported in a few cases in live patients).
Franco Servadei
Milan, Italy
This article is part of the Topical Collection on Neurosurgical technique evaluation
Rights and permissions
About this article
Cite this article
Maenhoudt, W., Hallaert, G., Kalala, JP. et al. Hydroxyapatite cranioplasty: a retrospective evaluation of osteointegration in 17 cases. Acta Neurochir 160, 2117–2124 (2018). https://doi.org/10.1007/s00701-018-3694-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-018-3694-6