Abstract
Aims
Nonalcoholic fatty liver disease (NAFLD) is a hepatic manifestation of metabolic syndrome and is closely associated with insulin resistance (IR). The ZJU index is based on body mass index (BMI), fasting plasma glucose (FPG), triglycerides (TG) and the serum alanine aminotransferase-to-aspartate transaminase ratio, and is proven to be a novel and effective parameter for screening NAFLD in the Chinese population. We aimed to analyze the relationship between the ZJU index and IR.
Methods
A cross-sectional study of 3329 Chinese adults was performed. Blood pressure (BP), anthropometric measurements and biochemical parameters were tested. The BMI, ZJU index and homeostasis model assessment of IR (HOMA-IR) were calculated.
Results
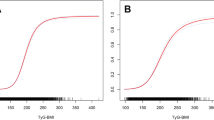
In both genders, BP, waist circumference, BMI, total cholesterol, TG, low-density lipoprotein cholesterol levels, FPG, postprandial glucose levels, fasting insulin and the HOMA-IR gradually increased, while the HDL-C decreased across the quartiles of the ZJU index (P < 0.001). The logistic regression analysis showed that the risk of IR was significantly elevated in the highest quartile of the ZJU index. Additionally, the area under the receiver operating characteristic curve of the ZJU index was 0.833 (95 % CI 0.809–0.858) in males and 0.788 (95 % CI 0.758–0.818) in females and was relatively higher than other common variables.
Conclusions
The ZJU index is a useful indicator for recognizing IR in the Chinese general population.

Similar content being viewed by others
References
Laakso M, Kuusisto J (2014) Insulin resistance and hyperglycaemia in cardiovascular disease development. Nat Rev Endocrinol 10(5):293–302
DeFronzo RA, Tobin JD, Andres R (1979) Glucose clamp technique: a method for quantifying insulin secretion and resistance. Am J Physiol 237(3):E214–E223
Matthews DR, Hosker JP, Rudenski AS et al (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28(7):412–419
Katsuki A, Sumida Y, Gabazza EC et al (2001) Homeostasis model assessment is a reliable indicator of insulin resistance during follow-up of patients with type 2 diabetes. Diabetes Care 24(2):362–365
Venkataraman K, Khoo CM, Leow MK et al (2013) New measure of insulin sensitivity predicts cardiovascular disease better than HOMA estimated insulin resistance. PLoS One 8(9):e74410
Miller WG, Thienpont LM, Van Uytfanghe K et al (2009) Toward standardization of insulin immunoassays. Clin Chem 55(5):1011–1018
Wang J, Xu C, Xun Y et al (2015) ZJU index: a novel model for predicting nonalcoholic fatty liver disease in a Chinese population. Sci Rep 5:16494
Lu J, Bi Y, Wang T, Wang W et al (2014) The relationship between insulin-sensitive obesity and cardiovascular diseases in a Chinese population: results of the REACTION study. Int J Cardiol 172(2):388–394
Du T, Yuan G, Zhang M et al (2014) Clinical usefulness of lipid ratios, visceral adiposity indicators, and the triglycerides and glucose index as risk markers of insulin resistance. Cardiovasc Diabetol 13:146
Asrih M, Jornayvaz FR (2015) Metabolic syndrome and nonalcoholic fatty liver disease: is insulin resistance the link? Mol Cell Endocrinol 418(Pt 1):55–65
Zhang Y, Zhang T, Zhang C (2014) Prediction of metabolic syndrome by non-alcoholic fatty liver disease in northern urban Han Chinese population: a prospective cohort study. PLoS One 9(5):e96651
Ning G, Reaction Study Group (2012) Risk evaluation of cAncers in Chinese diabeTic individuals: a lONgitudinal (REACTION) study. J Diabetes 4:172–173
Qu H, Wang H, Deng M, Wei H, Deng H (2014) Associations between longer habitual day napping and non-alcoholic fatty liver disease in an elderly Chinese population. PLoS One 9(8):e105583
Kim SH, Moon JY, Lim YM et al (2015) Association of insulin resistance and coronary artery remodeling: an intravascular ultrasound study. Cardiovasc Diabetol 14:74
Zhang Y, Lu X, Hong J et al (2010) Positive correlations of liver enzymes with metabolic syndrome including insulin resistance in newly diagnosed type 2 diabetes mellitus. Endocrine 38(2):181–187
Sookoian S, Pirola CJ (2012) Alanine and aspartate aminotransferase and glutamine-cycling pathway: their roles in pathogenesis of metabolic syndrome. World J Gastroenterol 18(29):3775–3781
Kawamoto R, Kohara K, Kusunoki T et al (2012) Alanine aminotransferase/aspartate aminotransferase ratio is the best surrogate marker for insulin resistance in non-obese Japanese adults. Cardiovasc Diabetol 11:117
Ochoa JE, Gallo JA, Correa MM (2015) Insulin resistance and beat-to-beat cardiovascular dynamics: a constant relationship across different body mass index and blood pressure categories. J Clin Endocrinol Metab 100(2):569–577
Acknowledgments
The authors wish to thank all the research staffs who have given their time so generously over the course of the REACTION study. This study was supported by the Grants from the Chinese Society of Endocrinology and the National Natural Science Foundation of China (81070639, 81270911, 30771038 and 30570744), and National Key Clinical Specialties Construction Program of China.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Baolan Ji, Hua Qu, Hang Wang, Huili Wei, and Huacong Deng declare that they have no conflict of interest.
Human and animal rights
The ethical committee of Shanghai Jiaotong University, and the First Affiliated Hospital of Chongqing Medical University approved this study. All procedures followed were performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed consent
Informed consent was obtained from all patients for being included in the study.
Additional information
Managed by Massimo Porta.
Rights and permissions
About this article
Cite this article
Ji, B., Qu, H., Wang, H. et al. The ZJU index: a useful indicator for recognizing insulin resistance in the Chinese general population. Acta Diabetol 53, 817–823 (2016). https://doi.org/10.1007/s00592-016-0878-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-016-0878-5