Abstract
Purpose
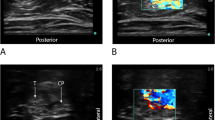
Ultrasound-guided long-axis in-plane sciatic perineural catheter insertion has been described but not validated. For the popliteal-sciatic nerve, we hypothesized that a long-axis in-plane technique, placing the catheter parallel and posterior to the nerve, results in faster onset of sensory anesthesia compared to a short-axis in-plane technique.
Methods
Preoperatively, patients receiving a popliteal-sciatic perineural catheter were randomly assigned to either the long-axis or short-axis technique. Mepivacaine 2 % was administered via the catheter following insertion. The primary outcome was time to achieve complete sensory anesthesia. Secondary outcomes included procedural time, onset time of motor block, and pain on postoperative day 1.
Results
Fifty patients were enrolled. In the long-axis group (n = 25), all patients except 1 (4 %) had successful catheter placement per protocol. Two patients (8 %) in the long-axis group and 1 patient (4 %) in the short-axis group (n = 25) did not achieve sensory anesthesia by 30 min and were withdrawn. Seventeen of 24 (71 %) and 17 of 22 (77 %) patients in the short-axis and long-axis groups, respectively, achieved the primary outcome of complete sensory anesthesia (p = 0.589). The short-axis group (n = 17) required a median (10th–90th ‰) of 18.0 (8.4–30.0) min compared to 18.0 (11.4–27.6) min for the long-axis group (n = 17, p = 0.208) to achieve complete sensory anesthesia. Procedural time was 6.5 (4.0–12.0) min for the short-axis and 9.5 (7.0–12.7) min for the long-axis (p < 0.001) group. There were no statistically significant differences in other secondary outcomes.
Conclusion
Long-axis in-plane popliteal-sciatic perineural catheter insertion requires more time to perform compared to a short-axis in-plane technique without demonstrating any advantages.


Similar content being viewed by others
References
Singelyn FJ, Aye F, Gouverneur JM. Continuous popliteal sciatic nerve block: an original technique to provide postoperative analgesia after foot surgery. Anesth Analg. 1997;84:383–6.
Ilfeld BM, Morey TE, Wang RD, Enneking FK. Continuous popliteal sciatic nerve block for postoperative pain control at home: a randomized, double-blinded, placebo-controlled study. Anesthesiology. 2002;97:959–65.
White PF, Issioui T, Skrivanek GD, Early JS, Wakefield C. The use of a continuous popliteal sciatic nerve block after surgery involving the foot and ankle: does it improve the quality of recovery? Anesth Analg. 2003;97:1303–9.
Singelyn FJ, Gouverneur JM, Gribomont BF. Popliteal sciatic nerve block aided by a nerve stimulator: a reliable technique for foot and ankle surgery. Reg Anesth. 1991;16:278–81.
Perlas A, Brull R, Chan VW, McCartney CJ, Nuica A, Abbas S. Ultrasound guidance improves the success of sciatic nerve block at the popliteal fossa. Reg Anesth Pain Med. 2008;33:259–65.
Ilfeld BM, Fredrickson MJ, Mariano ER. Ultrasound-guided perineural catheter insertion: three approaches but few illuminating data. Reg Anesth Pain Med. 2010;35:123–6.
Mariano ER, Cheng GS, Choy LP, Loland VJ, Bellars RH, Sandhu NS, Bishop ML, Lee DK, Maldonado RC, Ilfeld BM. Electrical stimulation versus ultrasound guidance for popliteal-sciatic perineural catheter insertion: a randomized controlled trial. Reg Anesth Pain Med. 2009;34:480–5.
Mariano ER, Loland VJ, Sandhu NS, Bellars RH, Bishop ML, Afra R, Ball ST, Meyer RS, Maldonado RC, Ilfeld BM. Ultrasound guidance versus electrical stimulation for femoral perineural catheter insertion. J Ultrasound Med. 2009;28:1453–60.
Mariano ER, Loland VJ, Sandhu NS, Bishop ML, Lee DK, Schwartz AK, Girard PJ, Ferguson EJ, Ilfeld BM. Comparative efficacy of ultrasound-guided and stimulating popliteal-sciatic perineural catheters for postoperative analgesia. Can J Anaesth. 2010;57:919–26.
Wang AZ, Gu L, Zhou QH, Ni WZ, Jiang W. Ultrasound-guided continuous femoral nerve block for analgesia after total knee arthroplasty: catheter perpendicular to the nerve versus catheter parallel to the nerve. Reg Anesth Pain Med. 2010;35:127–31.
Tammam TF. Ultrasound-guided infragluteal sciatic nerve block: a comparison between four different techniques. Acta Anaesthesiol Scand. 2013;57:243–8.
Tammam TF. Ultrasound-guided sciatic nerve block: a comparison between four different infragluteal probe and needle alignment approaches. J Anesth. 2013. doi:10.1007/s00540-013-1753-y
Mariano ER, Kim TE, Funck N, Walters T, Wagner MJ, Harrison TK, Giori N, Woolson S, Ganaway T, Howard SK. A randomized comparison of long-and short-axis imaging for in-plane ultrasound-guided femoral perineural catheter insertion. J Ultrasound Med. 2013;32:149–56.
Sahin L, Gurkan Y. “Figure of four” position and long-axis sciatic nerve scan with ultrasound facilitates sciatic perineural catheter placement. Agri. 2010;22:175–7.
Sandhu NS, Capan LM. Ultrasound-guided infraclavicular brachial plexus block. Br J Anaesth. 2002;89:254–9.
Buys MJ, Arndt CD, Vagh F, Hoard A, Gerstein N. Ultrasound-guided sciatic nerve block in the popliteal fossa using a lateral approach: onset time comparing separate tibial and common peroneal nerve injections versus injecting proximal to the bifurcation. Anesth Analg. 2010;110:635–7.
Cuvillon P, Nouvellon E, Ripart J, Boyer JC, Dehour L, Mahamat A, L’Hermite J, Boisson C, Vialles N, Lefrant JY, de La Coussaye JE. A comparison of the pharmacodynamics and pharmacokinetics of bupivacaine, ropivacaine (with epinephrine) and their equal volume mixtures with lidocaine used for femoral and sciatic nerve blocks: a double-blind randomized study. Anesth Analg. 2009;108:641–9.
Prasad A, Perlas A, Ramlogan R, Brull R, Chan V. Ultrasound-guided popliteal block distal to sciatic nerve bifurcation shortens onset time: a prospective randomized double-blind study. Reg Anesth Pain Med. 2010;35:267–71.
Perlas A, Wong P, Abdallah F, Hazrati LN, Tse C, Chan V. Ultrasound-guided popliteal block through a common paraneural sheath versus conventional injection: a prospective, randomized, double-blind study. Reg Anesth Pain Med. 2013;38:218–25.
de Tran QH, Gonzalez AP, Bernucci F, Pham K, Finlayson RJ. A randomized comparison between bifurcation and prebifurcation subparaneural popliteal sciatic nerve blocks. Anesth Analg. 2013;116:1170–5.
Andersen HL, Andersen SL, Tranum-Jensen J. Injection inside the paraneural sheath of the sciatic nerve: direct comparison among ultrasound imaging, macroscopic anatomy, and histologic analysis. Reg Anesth Pain Med. 2012;37:410–4.
Ilfeld BM, Le LT, Ramjohn J, Loland VJ, Wadhwa AN, Gerancher JC, Renehan EM, Sessler DI, Shuster JJ, Theriaque DW, Mariano ER; PAINfRETM Investigators. The effects of local anesthetic concentration and dose on continuous infraclavicular nerve blocks: a multicenter, randomized, observer-masked, controlled study. Anesth Analg. 2009;108:345–50.
Ilfeld BM, Loland VJ, Gerancher JC, Wadhwa AN, Renehan EM, Sessler DI, Shuster JJ, Theriaque DW, Maldonado RC, Mariano ER. The effects of varying local anesthetic concentration and volume on continuous popliteal sciatic nerve blocks: a dual-center, randomized, controlled study. Anesth Analg. 2008;107:701–7.
Kan JM, Harrison TK, Kim TE, Howard SK, Kou A, Mariano ER. An in vitro study to evaluate the utility of the “air test” to infer perineural catheter tip location. J Ultrasound Med. 2013;32:529–33.
Acknowledgments
The authors gratefully acknowledge the invaluable assistance of the entire operating and recovery room staff at the VA Palo Alto Health Care System, especially our Regional Anesthesia and Acute Pain Medicine Fellows, Drs. Jack Kan, Nate Ponstein, Brett Miller, Justin Workman, and Genie Kim.
Conflict of interest
Dr. Mariano has received unrestricted educational program funding paid to his institution from I-Flow Corporation (Lake Forest, CA, USA). This company had no input into any aspect of the present study design and implementation; data collection, analysis and interpretation; or manuscript preparation. Dr. Mariano has received research grant funding from the Foundation for Anesthesia Education and Research.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Edward Kim, T., Howard, S.K., Funck, N. et al. A randomized comparison of long-axis and short-axis imaging for in-plane ultrasound-guided popliteal-sciatic perineural catheter insertion. J Anesth 28, 854–860 (2014). https://doi.org/10.1007/s00540-014-1832-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-014-1832-8