Abstract
Background
Acute liver failure is a potentially fatal disease of various etiologies for which liver transplantation is the only known curative treatment. Although the decision-making on transplantation is largely dependent on the severity of liver injury (based on predicting a fatal outcome), a statistical analysis to predict “survival” has not been extensively conducted. In this study, we investigate the medical history of patients in two distinct areas of Japan with the aim of identifying the predictors of survival in patients with acute liver injury (ALI).
Methods
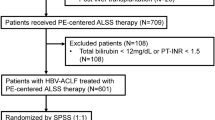
Datasets of 301 patients with ALI in two distinct areas (93 in southern Kyushu and 208 in northern Tohoku) of Japan, who were treated from 2004 to 2014, were included in the analysis.
Results
Among the enrolled 301 cases, 263 patients survived without transplantation. A PT-INR of ≥ 1.3 during the clinical course was found to be adequate for predicting a poor prognosis, because all of the fatal cases emerged from this population (hazard ratios: southern Kyushu, 0.2827; northern Tohoku, 0.1862). All surviving patients showed a reduction in their PT-INR during treatment, whereas the PT-INR did not decrease in the patients with a poor prognosis. A PT-INR of < 1.3 on days 7 and 8 efficiently predicted transplant-free survival (log-rank test: southern Kyushu, P = 0.0030; northern Tohoku, P = 0.0022).
Conclusions
A PT-INR of ≥ 1.3 during the clinical course might identify cases with a poor prognosis, while the recovery of the PT-INR to < 1.3 predicts transplant-free survival.





Similar content being viewed by others
Abbreviations
- ALI:
-
Acute liver injury
- ALF:
-
Acute liver failure
- PT:
-
Prothrombin time
- INR:
-
International normalized ratio
- PT[%]:
-
Prothrombin index
- ROC:
-
Receiver operating characteristic
- AUROC:
-
Area under ROC
- LOCF:
-
Last observation carried forward
- NA:
-
Nucleos(t)ide analog
- HGF:
-
Hepatocyte growth factor
- rh-HGF:
-
Recombinant human HGF
References
O’Grady JG, Schalm SW, Williams R. Acute liver failure: redefining the syndromes. Lancet. 1993;342:273–5.
Bernal W, Hyyrylainen A, Gera A, et al. Lessons from look-back in acute liver failure? A single centre experience of 3300 patients. J Hepatol. 2013;59:74–80.
Bernal W, Wendon J. Acute liver failure. N Engl J Med. 2013;369:2525–34.
Mochida S, Nakayama N. Acute liver failure and late onset hepatic failure (LOHF) in Japan (2014). Annual Report of the Study Group of Intractable Hepato-Biliary Study Group in Japan Supported by the Ministry of Health, Labor, and Welfare. 2016:116–35 (in Japanese).
Oketani M, Ido A, Nakayama N, et al. Etiology and prognosis of fulminant hepatitis and late-onset hepatic failure in Japan: summary of the annual nationwide survey between 2004 and 2009. Hepatol Res. 2013;43:97–105.
Mochida S, Takikawa Y, Nakayama N, et al. Diagnostic criteria of acute liver failure: a report by the Intractable Hepato-Biliary Diseases Study Group of Japan. Hepatol Res. 2011;41:805–12.
Fujiwara K, Yasui S, Yonemitsu Y, et al. Efficacy of high-dose corticosteroid in the early stage of viral acute liver failure. Hepatol Res. 2014;44:491–501.
Takikawa Y, Endo R, Suzuki K, et al. Early prediction of short-term development of hepatic encephalopathy in patients with acute liver disease unrelated to paracetamol. A prospective study in Japan. J Hepatol. 2009;51:1021–9.
Ueno Y, Ohmi T, Yamamoto M, et al. Orally-administered caspase inhibitor PF-03491390 is retained in the liver for prolonged periods with low systemic exposure, exerting a hepatoprotective effect against alpha-fas-induced liver injury in a mouse model. J Pharmacol Sci. 2007;105:201–5.
Nalpas B, Ichai P, Jamot L, et al. A proof of concept, phase II randomized European trial, on the efficacy of ALF-5755, a novel extracellular matrix-targeted antioxidant in patients with acute liver diseases. PLoS One. 2016;11:e0150733.
Ido A, Moriuchi A, Numata M, et al. Safety and pharmacokinetics of recombinant human hepatocyte growth factor (rh-HGF) in patients with fulminant hepatitis: a phase I/II clinical trial, following preclinical studies to ensure safety. J Transl Med. 2011;9:55.
Bernuau J. Selection for emergency liver transplantation. J Hepatol. 1993;19:486–7.
Mochida S, Nakayama N, Ido A, et al. Revised criteria for classification of the etiologies of acute liver failure and late-onset hepatic failure in Japan: a report by the Intractable Hepato-biliary Diseases Study Group of Japan in 2015. Hepatol Res. 2016;46:369–71.
Wiegand J, Wedemeyer H, Franke A, et al. Treatment of severe, nonfulminant acute hepatitis B with lamivudine vs placebo: a prospective randomized double-blinded multicentre trial. J Viral Hepat. 2014;21:744–50.
Tillmann HL, Hadem J, Leifeld L, et al. Safety and efficacy of lamivudine in patients with severe acute or fulminant hepatitis B, a multicenter experience. J Viral Hepat. 2006;13:256–63.
Yu JW, Sun LJ, Zhao YH, et al. The study of efficacy of lamivudine in patients with severe acute hepatitis B. Dig Dis Sci. 2010;55:775–83.
Drafting Committee for Hepatitis Management Guidelines and the Japan Society of Hepatology. JSH Guidelines for the management of hepatitis B virus infection. Hepatol Res. 2014;44 Suppl S1:1–58
Yamamoto K, Miyake Y, Ohira H, et al. Prognosis of autoimmune hepatitis showing acute presentation. Hepatol Res. 2013;43:630–8.
Karkhanis J, Verna EC, Chang MS, et al. Steroid use in acute liver failure. Hepatology. 2014;59:612–21.
Kakisaka K, Kataoka K, Suzuki Y, et al. Appropriate timing to start and optimal response evaluation of high-dose corticosteroid therapy for patients with acute liver failure. J Gastroenterol. 2017;52:977–85
Nalpas B, Francoz C, Ichai P, et al. Prothrombin index slope is an early prognostic marker in patients with severe acute liver diseases. Gut. 2012;61:1098–100.
Gohda E, Tsubouchi H, Nakayama H, et al. Purification and partial characterization of hepatocyte growth factor from plasma of a patient with fulminant hepatic failure. J Clin Invest. 1988;81:414–9.
Tsubouchi H, Hirono S, Gohda E, et al. Clinical significance of human hepatocyte growth factor in blood from patients with fulminant hepatic failure. Hepatology. 1989;9:875–81.
Miyazawa K, Tsubouchi H, Naka D, et al. Molecular cloning and sequence analysis of cDNA for human hepatocyte growth factor. Biochem Biophys Res Commun. 1989;163:967–73.
Tsubouchi H, Niitani Y, Hirono S, et al. Levels of the human hepatocyte growth factor in serum of patients with various liver diseases determined by an enzyme-linked immunosorbent assay. Hepatology. 1991;13:1–5.
Ishiki Y, Ohnishi H, Muto Y, et al. Direct evidence that hepatocyte growth factor is a hepatotrophic factor for liver regeneration and has a potent antihepatitis effect in vivo. Hepatology. 1992;16:1227–35.
Kosai K, Matsumoto K, Nagata S, et al. Abrogation of Fas-induced fulminant hepatic failure in mice by hepatocyte growth factor. Biochem Biophys Res Commun. 1998;244:683–90.
Yasuda H, Imai E, Shiota A, et al. Antifibrogenic effect of a deletion variant of hepatocyte growth factor on liver fibrosis in rats. Hepatology. 1996;24:636–42.
Bussolino F, Di Renzo MF, Ziche M, et al. Hepatocyte growth factor is a potent angiogenic factor which stimulates endothelial cell motility and growth. J Cell Biol. 1992;119:629–41.
Takikawa Y, Harada M, Wang T, et al. Usefulness and accuracy of the international normalized ratio and activity percent of prothrombin time in patients with liver disease. Hepatol Res. 2014;44:92–101.
Acknowledgements
This research and development program was partially supported by the Medical Research and Development Programs Focused on Technology Transfer: Adaptable and Seamless Technology Transfer Program through Target-Driven Research and Development (A-STEP) of Japan Agency for Medical Research and Development.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
535_2017_1421_MOESM1_ESM.docx
Supplemental Fig. 1. The outcomes of the whole study population stratified by PT-INR. (A) ROC curves for the PT(%) at the last observation (n = 301). (B) Kaplan–Meier curves for transplant-free survival to Day 30 in each group stratified by the two levels of PT-INR at the last observation (PT-INR < 1.3, PT-INR ≥ 1.3) (n = 301). Patients in the PT-INR < 1.3 group showed significantly higher rates of transplant-free survival than those in the PT-INR ≥ 1.3 group (Log-rank test: P = 0.0004, hazard ratio of PT-INR < 1.3 group/PT-INR ≥ 1.3 group: 0.2241 [95% CI: 0.09867–0.5091, Mantel–Haenszel]). (C) The outcomes by event and PT-INR < 1.3 recovery (n = 188). (D) Kaplan–Meier curves for each group stratified by PT-INR < 1.3 recovery at Day 8 or transplantation/death before Day 30 (n = 188). The patients in the PT < 1.3 recovery group showed significantly higher rates of transplant-free survival (Log-rank test: P < 0.0001, hazard ratio of PT-INR < 1.3 recovery group/no recovery group: 0.1593 [95% CI: 0.0734–0.3457, Mantel-Haenszel]). Supplemental Fig. 2. The patients outcomes stratified by PT(%). (A) ROC curves for the PT(%) at the last observation (n = 304). (B) Kaplan–Meier curves for transplant-free survival to Day 30 in each group stratified by the two levels of PT(%) at the last observation (PT(%) ≥ 60%, PT(%) < 60%) (n = 304). Patients in the PT(%) ≥ 60% group showed significantly higher rates of transplant-free survival than those in the PT(%) < 60% group (Log-rank test: P < 0.0001, hazard ratio of PT-INR < 1.3 group/PT-INR ≥ 1.3 group: 0.1919 [95% CI: 0.08761–0.4226, Mantel–Haenszel]). (C) The outcomes by event and PT(%) ≥ 60% recovery (n = 171). (D) Kaplan–Meier curves for each group stratified by PT(%) ≥ 60% recovery at Day 8 or transplantation/death before Day 30 (n = 171). Patients in the PT(%) ≥ 60% recovery group showed significantly higher rates of transplant-free survival (Log-rank test: P < 0.0001, hazard ratio of PT-INR < 1.3 group/PT-INR ≥ 1.3 group: 0.1293 [95% CI: 0.05977–0.2798, Mantel–Haenszel]). Supplemental Fig. 3. Correlation diagram between PT(%) and PT-INR. R2:decision coefficient (DOCX 3459 kb)
Rights and permissions
About this article
Cite this article
Mawatari, S., Moriuchi, A., Ohba, F. et al. The recovery of the PT-INR to less than 1.3 predicts survival in patients with severe acute liver injury. J Gastroenterol 53, 861–872 (2018). https://doi.org/10.1007/s00535-017-1421-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-017-1421-3